Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Chyzy, Adam
Pawelski, Damian
Vivcharenko, Vladyslav
Przekora, Agata
Bratychak, Michael
Astakhova, Olena
Breczko, Joanna
Drozdzal, Pawel
and
Plonska-Brzezinska, Marta E.
2022.
Microwave-Assisted Synthesis of Modified Glycidyl Methacrylate–Ethyl Methacrylate Oligomers, Their Physico-Chemical and Biological Characteristics.
Molecules,
Vol. 27,
Issue. 2,
p.
337.
Kim, Se-jeong
Byun, Hayeon
Lee, Sangmin
Kim, Eunhyung
Lee, Gyeong Min
Huh, Seung Jae
Joo, Jinmyoung
and
Shin, Heungsoo
2022.
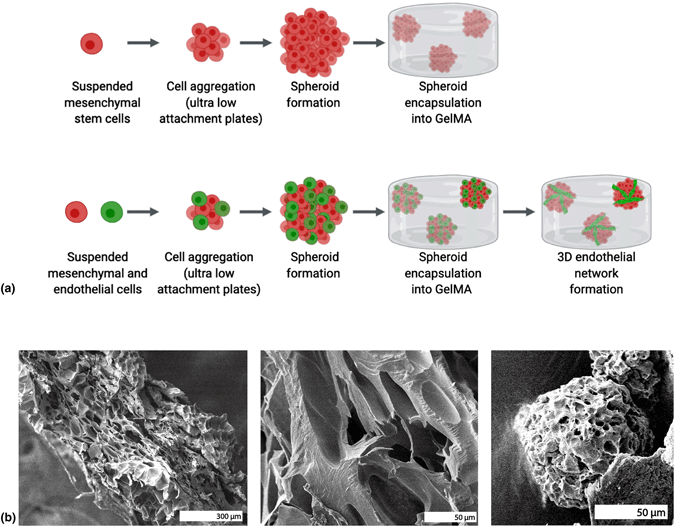
Spatially arranged encapsulation of stem cell spheroids within hydrogels for the regulation of spheroid fusion and cell migration.
Acta Biomaterialia,
Vol. 142,
Issue. ,
p.
60.
Gering, Christine
Párraga, Jenny
Vuorenpää, Hanna
Botero, Lucía
Miettinen, Susanna
and
Kellomäki, Minna
2022.
Bioactivated gellan gum hydrogels affect cellular rearrangement and cell response in vascular co-culture and subcutaneous implant models.
Biomaterials Advances,
Vol. 143,
Issue. ,
p.
213185.
Azuraini, Mat Junoh
Vigneswari, Sevakumaran
Huong, Kai-Hee
Khairul, Wan M.
H.P.S., Abdul Khalil
Ramakrishna, Seeram
and
Amirul, Al-Ashraf Abdullah
2022.
Surface Modification of Sponge-like Porous Poly(3-hydroxybutyrate-co-4-hydroxybutyrate)/Gelatine Blend Scaffolds for Potential Biomedical Applications.
Polymers,
Vol. 14,
Issue. 9,
p.
1710.
Weygant, Joshua
Koch, Fritz
Adam, Katrin
Tröndle, Kevin
Zengerle, Roland
Finkenzeller, Günter
Kartmann, Sabrina
Koltay, Peter
and
Zimmermann, Stefan
2023.
A Drop-on-Demand Bioprinting Approach to Spatially Arrange Multiple Cell Types and Monitor Their Cell-Cell Interactions towards Vascularization Based on Endothelial Cells and Mesenchymal Stem Cells.
Cells,
Vol. 12,
Issue. 4,
p.
646.
Schulik, Jana
Salehi, Sahar
Boccaccini, Aldo
Schrüfer, Stefan
Schubert, Dirk
Arkudas, Andreas
Kengelbach-Weigand, Annika
Horch, Raymund
and
Schmid, Rafael
2023.
Comparison of the Behavior of 3D-Printed Endothelial Cells in Different Bioinks.
Bioengineering,
Vol. 10,
Issue. 7,
p.
751.
Genç, Hatice
Cianciosi, Alessandro
Lohse, Raphael
Stahlhut, Philipp
Groll, Jürgen
Alexiou, Christoph
Cicha, Iwona
and
Jüngst, Tomasz
2023.
Adjusting Degree of Modification and Composition of gelAGE-Based Hydrogels Improves Long-Term Survival and Function of Primary Human Fibroblasts and Endothelial Cells in 3D Cultures.
Biomacromolecules,
Vol. 24,
Issue. 3,
p.
1497.
Simińska-Stanny, Julia
Hachemi, Feza
Dodi, Gianina
Cojocaru, Florina D.
Gardikiotis, Ioannis
Podstawczyk, Daria
Delporte, Christine
Jiang, Guohua
Nie, Lei
and
Shavandi, Amin
2023.
Optimizing phenol-modified hyaluronic acid for designing shape-maintaining biofabricated hydrogel scaffolds in soft tissue engineering.
International Journal of Biological Macromolecules,
Vol. 244,
Issue. ,
p.
125201.
Singh, Archana
Dalal, Neha
and
Tayalia, Prakriti
2023.
An interplay of matrix stiffness, dimensionality and adhesivity on cellular behavior.
Biomedical Materials,
Vol. 18,
Issue. 2,
p.
025010.
Cojocaru, Elena
Ghitman, Jana
Pircalabioru, Gratiela Gradisteanu
Zaharia, Anamaria
Iovu, Horia
and
Sarbu, Andrei
2023.
Electrospun/3D-Printed Bicomponent Scaffold Co-Loaded with a Prodrug and a Drug with Antibacterial and Immunomodulatory Properties.
Polymers,
Vol. 15,
Issue. 13,
p.
2854.
Iijima, Yuta
Uenaka, Norino
Morimoto, Mayu
Sato, Daiki
Hirose, Satomi
Sakitani, Naoyoshi
Shinohara, Masahiro
Funamoto, Kenichi
Hayase, Gen
and
Yoshino, Daisuke
2024.
Biological characterization of breast cancer spheroid formed by fast fabrication method.
In vitro models,
Vol. 3,
Issue. 1,
p.
19.
Kapoor, Devesh
Verma, Kanika
Jain, Smita
and
Sharma, Swapnil
2024.
Biomaterial-based Hydrogels.
p.
67.
Park, Se Yeon
Koh, Won-Gun
and
Lee, Hyun Jong
2024.
Enhanced hepatotoxicity assessment through encapsulated HepG2 spheroids in gelatin hydrogel matrices: Bridging the gap from 2D to 3D culture.
European Journal of Pharmaceutics and Biopharmaceutics,
Vol. 202,
Issue. ,
p.
114417.
Jeong, Seo Yule
Kim, Ju-Kang
Lee, Yu Bin
Moon, Kyoung-Sik
and
Woo, Dong Ho
2024.
A method to measure the receptor-mediated Ca2+ transients in non-adherent THP-1 monocytes using gelatin methacryloyl for immobilization in a bath perfusion system.
Molecular & Cellular Toxicology,
Yu, Jiangnan
Ni, Min
Liu, Kai
Pan, Pengfei
Li, Xiaoli
Zhang, Jin
Deng, Tianwen
Wang, Qilong
Xu, Ximing
and
Cao, Xia
2025.
Electrospinning of microspheres with ectodermal mesenchymal stem cells for vascular regeneration.
European Polymer Journal,
Vol. 224,
Issue. ,
p.
113716.