Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Sekar, Prithivirajan
S, Narendranath
and
Desai, Vijay
2021.
Recent progress in in vivo studies and clinical applications of magnesium based biodegradable implants – A review.
Journal of Magnesium and Alloys,
Vol. 9,
Issue. 4,
p.
1147.
Su, Yun-Han
Pan, Cheng-Tang
Tseng, Yu-Sheng
Zhang, Ji
and
Chen, Wen-Fan
2021.
Rare earth element cerium substituted Ca–Si–Mg system bioceramics: From mechanism to mechanical and degradation properties.
Ceramics International,
Vol. 47,
Issue. 14,
p.
19414.
He, Fupo
Yuan, Xinyuan
Lu, Teliang
Wang, Yao
Feng, Songheng
Shi, Xuetao
Wang, Lin
Ye, Jiandong
and
Yang, Hui
2022.
Preparation and characterization of novel lithium magnesium phosphate bioceramic scaffolds facilitating bone generation.
Journal of Materials Chemistry B,
Vol. 10,
Issue. 21,
p.
4040.
Radhakrishnan, Anitha
Sreekumaran, Sreekanth
Anjali, Sudha
Resmi, Rajalekshmi
and
Saravana, Ramakrishna Perumal
2022.
Tissue Engineering.
p.
469.
Bavya Devi, K.
Lalzawmliana, V.
Saidivya, Maktumkari
Kumar, Vinod
Roy, Mangal
and
Kumar Nandi, Samit
2022.
Magnesium Phosphate Bioceramics for Bone Tissue Engineering.
The Chemical Record,
Vol. 22,
Issue. 11,
He, Zhijing
Jiao, Chen
Zhang, Hanxu
Xie, Deqiao
Ge, Mengxing
Yang, Youwen
Wu, Guofeng
Liang, Huixin
Shen, Lida
and
Wang, Changjiang
2022.
Fabrication of a zirconia/calcium silicate composite scaffold based on digital light processing.
Ceramics International,
Vol. 48,
Issue. 18,
p.
25923.
He, Fupo
Yuan, Xinyuan
Fu, Wenhao
Huang, Wenhao
Chen, Tengyun
Feng, Songheng
Wang, Huaiyu
and
Ye, Jiandong
2023.
Preparation of lithium-containing magnesium phosphate-based composite ceramics having high compressive strength, osteostimulation and proangiogenic effects.
Biomedical Materials,
Vol. 18,
Issue. 6,
p.
065008.
Díaz-Puertas, Rocío
Rodríguez-Cañas, Enrique
Bello-Perez, Melissa
Fernández-Oliver, Marta
Mallavia, Ricardo
and
Falco, Alberto
2023.
Viricidal Activity of Thermoplastic Polyurethane Materials with Silver Nanoparticles.
Nanomaterials,
Vol. 13,
Issue. 9,
p.
1467.
He, Fupo
Rao, Jin
Zhou, Jielin
Fu, Wenhao
Wang, Yao
Zhang, Yihang
Zuo, Fei
and
Shi, Haishan
2023.
Fabrication of 3D printed Ca3Mg3(PO4)4-based bioceramic scaffolds with tailorable high mechanical strength and osteostimulation effect.
Colloids and Surfaces B: Biointerfaces,
Vol. 229,
Issue. ,
p.
113472.
Mouli, Karaka VVNR Chandra
Reddy, Yakkaluru Ramamohan
and
Prakash, Kode Jaya
2024.
An experimental approach to characterize the performance of PCD and PCBN tools in milling nano Al-8081-Zr/Mg/TiO2 metal matrix composites using multi-sensor data fusion.
Proceedings of the Institution of Mechanical Engineers, Part C: Journal of Mechanical Engineering Science,
Vol. 238,
Issue. 12,
p.
5699.
Chen, Tengyun
Shuai, Wei
Fu, Wenhao
Li, Yanfei
Wen, Renzhi
Fu, Qiuyu
He, Fupo
and
Yang, Hui
2024.
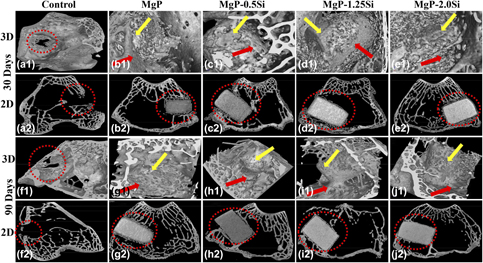
Improving mechanical strength and osteo-stimulative capacity of 3D-printed magnesium phosphate ceramic scaffolds by magnesium silicate additives.
Ceramics International,
Vol. 50,
Issue. 21,
p.
43458.
Sarkar, Kaushik
2024.
Research progress on biodegradable magnesium phosphate ceramics in orthopaedic applications.
Journal of Materials Chemistry B,
Vol. 12,
Issue. 35,
p.
8605.