Introduction
Surgeons and hospitals need continuous feedback from patients about surgical outcomes to maintain and improve the quality of their surgery. The Department of Otorhinolaryngology at Lovisenberg Diaconal Hospital performs ongoing quality control evaluations of nasal septal surgery by post-operatively contacting and assessing patients by mail and/or telephone. Our early results for the first year after surgery have been previously published,Reference Haye, Egeland, Døsen, Gay, TarAngen and Shiryaeva1 and show positive results comparable to those in a review by Rhee et al.Reference Rhee, Sullivan, Frank, Kimbell and Garcia2 Long-term prospective outcome studies after septoplasty are few, with widely differing degrees of success.Reference Tsang, Nguyen, Sivesind and Cervin3 Van Egmond et al.,Reference Van Egmond, Rovers, Tillema and van Neerbeek4 in their review of long-term outcomes, concluded that more long-term studies were needed to assess the durability of symptom improvement after septoplasty.
Septoplasty consists of straightening the structural elements of the nasal septum. Our early post-operative results indicate that the realignment was successful. However, we do not know if the modified cartilage and bones retain their inherent structure and keep their new position over time. Therefore, Lovisenberg Diaconal Hospital's Department of Otorhinolaryngology initiated the present study primarily to evaluate whether the improvement in nasal surgery outcomes was stable after three to four years. Our secondary aim was to assess the relationships between surgical outcomes and clinical, surgical and demographic variables.
Materials and methods
The study was approved by the Ethics Committee of Lovisenberg Diaconal Hospital. It included patients who underwent septoplasty with or without turbinoplasty at Lovisenberg Diaconal Hospital between April 2014 and December 2015. Patients were aged at least 17 years, and had no nasal or sinus disease other than allergy. Some patients had previously undergone either septoplasty or rhinoplasty. Review of their surgical records revealed no sequelae that caused difficulties in performing the secondary septoplasty, and these patients were therefore included in the study.
Procedures
The Department of Otorhinolaryngology at Lovisenberg Diaconal Hospital routinely uses the Nasal Surgical QuestionnaireReference Haye, Amlie, Shireyaeva and Døsen5 to assess the results of nasal septal surgery. The pre-operative version of this questionnaire is completed by the patient in the morning on the day of surgery. The post-operative version, together with a cover letter signed by a surgeon in our department and a prepaid return envelope, is routinely mailed to each patient six months after surgery to assess the early surgical results. Patients who do not return their questionnaire within three weeks are sent a reminder letter with the same questionnaire. For this study, the Nasal Surgical Questionnaire was also mailed to each patient three years post-operatively (to assess late surgical results).
The Nasal Surgical Questionnaire instructions ask patients to respond to each question indicating how they felt on a normal day without any infection. In order to minimise seasonal effects, mailings of the Nasal Surgical Questionnaire were suspended during the summer holiday season from mid-June and resumed in mid-August, which increased the response interval for some patients. This summer hiatus coincides with the main pollen season.
Both the pre- and post-operative versions of the Nasal Surgical Questionnaire contain a visual analogue scale (VAS) for nasal obstruction experienced during the day and at night. The VAS has a 10 cm line, with the left end representing no obstruction and the right end representing complete obstruction. Patients are asked to rate their experience of nasal obstruction on the scale with a vertical line. Each item score reflects the distance in millimetres as measured from the left-hand side of the scale to the patient's marked line.
For other nasal symptoms and therapies, four-point Likert scales are used with the following response categories: none, mild, moderate, and severe or daily symptoms or daily use. In addition, questions about smoking habits and nasal allergies are included. Since November 2014, the Nasal Surgical Questionnaire has also included an item asking about the presence of allergy at the time of the response.
The post-operative version of the Nasal Surgical Questionnaire has three additional questions that are not included in the pre-operative version: ‘At present, is your breathing completely, much or somewhat improved, unchanged or worse?’; ‘After your septoplasty, have you had any new nasal operation?’; and ‘After your septoplasty, have you received any new nasal trauma?’.
Patients who did not return either the initial or the reminder questionnaire (35 per cent the first year, 38 per cent the fourth year) were contacted and interviewed by telephone. The telephone interviews took place mostly outside the main pollen season. In the telephone interviews, the patients were asked to rate their sense of nasal obstruction on a numerical rating scale ranging from 0 to 10 (0 = no obstruction and 10 = complete obstruction) in lieu of the VAS. The numerical rating scale response was multiplied by 10 to be comparable to the VAS score and was included in the analysis. Our prior work has shown this to be a valid approach, given the good correlation between the VAS and the numerical rating scale.Reference Haye, Døsen, Tarangen and Shiryaeva6 For the early post-operative assessments, a female nurse performed half of the telephone interviews, while a male nasal surgeon performed the other half as well as all of the late post-operative assessments. Both interviewers were unknown to the patients.
Patients reporting either no improvement or a worsening of nasal obstruction at the early post-operative assessment are offered a consultation free of charge to address their ongoing symptoms. Their symptoms and signs are evaluated, and, when indicated, additional treatment is offered. Patients who needed secondary septoplasty and/or additional turbinoplasty were included in the study. Patients who later developed chronic rhinosinusitis were excluded.
In addition to patient-reported symptoms assessed with the Nasal Surgical Questionnaire, the following surgical and clinical characteristics were recorded by the surgeon immediately after the operation: type of prior nasal surgery performed, grade of septal deviation (large = touching or nearly touching the lateral wall, medium = occupying 50 per cent or more of the lumen, or small = occupying less than 50 per cent of the lumen), side of septal deviation (right, left or both sides), side of submucous turbinoplasty (right, left or both sides), presence and type of turbinate hypertrophy (bony, mucous membrane or combined), and presence of crusting, bleeding, synechia or secretion.
Of the demographic variables, age might affect primary healing and influence later connective tissue changes, so we decided to compare the surgical results of older (age above the mean of the cohort) with younger patients to evaluate the impact of age. As patients with more severe nasal obstruction (higher VAS scores) have greater potential for improvement than those with milder symptoms, we also compared patients with pre-operative obstruction scores above the cohort mean with those who had scores below this mean.
Statistical analysis
Descriptive statistics (means, standard deviations and frequencies) were used to summarise sample characteristics and questionnaire responses. Because of the non-parametric nature of the nasal obstruction VAS and numerical rating scale scores (Kolmogorov–Smirnov p < 0.05), Mann–Whitney U tests were used to evaluate group differences and Wilcoxon signed-rank tests were used to evaluate within-subject changes in nasal obstruction scores over time. All of the analyses were two-sided, and statistical significance was defined as p < 0.05. Statistical analyses were performed using IBM SPSS software, version 24.0 (IBM, Armonk, New York, USA).
Results
Of the 604 surgically recorded patients (434 males and 170 females, with a mean age of 35.7 years (range, 17–75 years)), 534 (88.4 per cent) completed the pre-operative questionnaire, 579 (95.5 per cent) completed the early post-operative questionnaire and 542 (89.7 per cent) completed the late post-operative questionnaire. The mean response time was 7.5 months (range, 6–12 months) after surgery for the early assessment and 40 months (range, 36–48 months) for the late assessment.
There was significant improvement in both daytime and night-time nasal obstruction scores from the pre-operative assessment to both the early and late post-operative assessments (Table 1). The improvement in nasal obstruction was largest from the pre-operative assessment to the early post-operative assessment, within the first year after surgery. Twenty-seven patients successfully underwent corrective septal or turbinate surgery for nasal obstruction after the early post-operative assessment. In order to investigate the differences between the early and late responses to the primary surgery, we excluded the 27 patients who had corrective surgery performed. We found a significant worsening in both daytime and night-time nasal obstruction from the early to the late post-operative assessment (with score increases of 5.3 and 9.7, respectively).
Table 1. Comparison of pre-operative and early and late post-operative ratings of daytime and night-time nasal obstruction
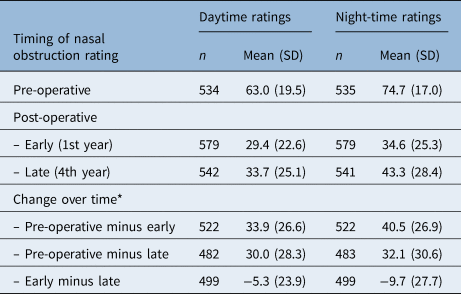
* p < 0.001 for all comparisons of change over time. SD = standard deviation
Pre-operative severity
Patients with more severe pre-operative nasal obstruction (VAS score range of 63–100), compared to those with less severe pre-operative nasal obstruction, had significantly larger reductions in VAS scores at both the early and late post-operative assessments (Table 2). Despite their greater improvement, however, patients with more severe nasal obstruction pre-operatively continued to have more severe nasal obstruction at both the early and late post-operative assessments compared with patients who had less severe nasal obstruction pre-operatively. The change in nasal obstruction from the early to late post-operative assessments was equal between the groups.
Table 2. Comparison of pre- and post-operative nasal obstruction ratings according to low versus high pre-operative nasal obstruction severity*

* A low level of pre-operative nasal obstruction severity was defined as ratings of 0–62, and a high level of severity was defined as ratings of 63–100. SD = standard deviation
Patient age
Older patients (aged 36–75 years) had significantly more improvement in nasal obstruction than younger ones (aged 17–35 years) (Table 3) at both the early and late post-operative assessments. However, the slight increase in nasal obstruction from the early to the late post-operative assessment was similar in both age groups.
Table 3. Comparison of pre- and post-operative nasal obstruction ratings in older versus younger patients

SD = standard deviation
Patient gender
The nasal obstruction scores of female patients during the day were slightly, but not significantly, worse than those of males at the pre-operative (p = 0.67) and the early (p = 0.67) and late (p = 0.54) post-operative assessments. At night, these were significant pre-operatively (p = 0.03) and at early assessment (p = 0.04). However, the pre-operative to early (day p = 0.69, night p = 0.61) and late (day p = 0.45, night p = 0.39) post-operative changes in nasal obstruction were similar for both genders. This was also the case for early to late post-operative changes (day p = 0.73, night p = 0.26).
Nasal allergy
Patients with and without nasal allergy had similar nasal obstruction scores at the pre-operative (day p = 0.25, night p = 0.44) and early (day p = 0.28, night p = 0.50) and late (day p = 0.33, night p = 0.50) post-operative assessments, and had similar changes over time. There were similarly small increases in nasal obstruction from the early to the late post-operative assessments for both groups (day p = 0.80, night p = 0.91).
Smoking
Daily smokers had significantly higher pre-operative nasal obstruction scores than non-smokers both during the day and at night (Table 4). The improvement after surgery, however, was similar for both smokers and non-smokers from the pre-operative to both the early and late post-operative assessments, and from the early to the late post-operative assessments.
Table 4. Comparison of pre- and post-operative nasal obstruction ratings in smokers versus non-smokers

SD = standard deviation
Septal deviation
Patients with a substantial septal deviation reported more pre-operative nasal obstruction than those with moderate deviations, and this was significant for daytime ratings (Table 5). The improvement in nasal obstruction was better for patients with substantial deviation (significant only from pre-operative to early post-operative assessment for night-time ratings), and therefore the final post-operative results were similar for both groups.
Table 5. Comparison of pre- and post-operative nasal obstruction ratings according to medium versus large septal deviations

SD = standard deviation
In comparing patients with one-sided septal deviation (right or left) with those in whom the septum deviated to both sides, we found no significant differences, and the increase in obstruction scores from the early to late post-operative assessments was similar for both groups (day p = 0.48, night p = 0.72).
Patients with septal deviation and bony turbinal hypertrophy underwent septoplasty and turbinoplasty. They were compared to patients without turbinal hypertrophy who were only treated with septoplasty, and no significant differences between these two groups were evident. The deterioration in nasal obstruction from early to late post-operative assessment was similar (day p = 0.53, night p = 0.92).
Other nasal symptoms and treatments
The percentage of patients reporting considerable crusting was similar across all assessments (about 9 per cent), whereas sneezing and watery secretion were reduced by 50 per cent at the early and late post-operative assessments. Pre-operatively, 8 per cent of patients used nasal decongestants on a daily basis, and this was reduced at both post-operative assessments. The use of antihistamines remained the same over time, but the use of corticosteroid nasal spray at both post-operative assessments was reduced compared to the pre-operative level.
Discussion
The study results show significant improvement in patient-reported nasal obstruction following nasal septal surgery as measured in both the first and the fourth year after surgery. The degree of improvement observed in this study is comparable to that reported in a review article.Reference Rhee, Sullivan, Frank, Kimbell and Garcia2 As nasal obstruction in the 27 re-operated patients was greatly improved post-operatively and might have biased the early to late post-operative results for the total cohort, their results were not included in comparisons of the early and late results. In the rest of the cohort, nasal obstruction significantly increased from the early to the late post-operative assessment, by 5.3 points during the day and 9.7 points at night. This slight worsening of nasal obstruction may not be clinically significant during the day, but at night it might contribute to reduced sleep quality.
Prior studies on late post-operative assessment of septoplasty have yielded varied findings. In their landmark clinical trial showing the efficacy of septoplasty in comparison to non-surgical treatment, Van Egmond et al.Reference Van Egmond, Rovers, Hannink, Hendriks and van Heerbeek7 also showed that post-operative improvement for the 102 patients who underwent septoplasty with or without turbinate surgery seemed to peak at 6 months, followed by a slight deterioration in the treatment effect at 24 months. Similarly, Valsamidis et al.Reference Valsamidis, Titelis, Rachovitsas, Konstantinidis, Markou and Triaridis8 found that in 40 non-allergic patients treated with septoplasty and turbinoplasty, nasal obstruction decreased over the first 6 months, but increased thereafter to the 36 month follow up. Moreover, Samarei and MabarianReference Samarei and Mabarian9 found that in 137 non-allergic patients, those treated with septoplasty alone experienced improved nasal obstruction up to 24 months after surgery but worsened thereafter, whereas those who also underwent turbinoplasty continued to improve up to 48 months.
In contrast, a study by De Sousa Fontes et al.Reference De Sousa Fontes, Sandrea Jiménez and Chacaltana Ayerve10 showed no change in post-operative improvement from six weeks to five years in patients who underwent septoplasty. Haavisto and SipiläReference Haavisto and Sipilä11 found that post-operative improvements deteriorated from 6 months to 10 years in 24 patients who underwent septoplasty with or without turbinoplasty, although they used ratings only for the decongested narrow side, so their results may be less comparable to studies using overall ratings of nasal obstruction. In a retrospective study of septoplasty outcomes, Sundh and SunnergrenReference Sundh and Sunnergren12 found that 53 per cent of patients with outcome ratings at 3–5.5 years after septoplasty (n = 99) reported that nasal obstruction was either not improved or had worsened, compared with only 19 per cent of patients with outcome ratings at 6 months (n = 68). Although the methodologies and results of previous studies vary, the majority show, in accordance with our own results, that initial post-operative improvement in nasal obstruction deteriorates over time.
Comparisons of surgical outcomes for septoplasty alone versus septoplasty with turbinoplasty have also yielded inconsistent findings in prior studies. Two studiesReference Samarei and Mabarian9,Reference Yamasaki, Levesque, Bleier, Busaba, Gray and Holbrook13 have shown that, after initial post-operative improvement, the long-term outcome deteriorated only in patients undergoing septoplasty, but not in those who underwent both septoplasty and turbinoplasty. In both studies, turbinoplasty was performed because of enlarged turbinates. In one of the studies,Reference Yamasaki, Levesque, Bleier, Busaba, Gray and Holbrook13 only 58 of the original 567 patients were included in the analysis at the 24-month follow up because the study was still ongoing, although there seemed to be no evidence of selection bias related to this small subsample. In contrast, Van Egmond et al.Reference Van Egmond, Rovers, Hannink, Hendriks and van Heerbeek7 reported no difference in the outcomes of septoplasty and septoplasty with turbinate surgery after one year. In a five-year longitudinal studyReference Illum14 of 37 patients randomly assigned to septoplasty with or without turbinoplasty, no difference in satisfaction was found between the groups. Although our study did not include random assignment, our findings support the view that there is no difference in the outcome between septoplasty and septoplasty with turbinoplasty if the additional turbinoplasty is performed because of an enlarged bony turbinate.
Our findings are also generally consistent with those of other studies reporting septoplasty outcomes in relation to pre-operative disease and symptom characteristics. One prospectiveReference Konstantinidis, Triaridis, Triaridis, Karagiannidis and Kontzoglou15 and one retrospective studyReference Toyserkani and Frisch16 showed, in accordance with our findings, that patients with higher pre-operative ratings of nasal obstruction have better improvement after surgery than those with lower ratings. This is not surprising, as the potential for improvement is much greater when the pre-operative score is higher. However, despite their larger post-operative improvement over time, the final result indicated that those with higher pre-operative scores still had more post-operative nasal obstruction than patients with lower pre-operative scores. In the study by Van Egmond et al.,Reference Van Egmond, Rovers, Hannink, Hendriks and van Heerbeek7 there was slightly more improvement among patients with severe septal deviations than among those with small or moderate deviations, but this difference was not clinically significant. In our study, the slightly better improvement in obstruction after surgery in patients with large than in those with medium-sized septal deviations did not explain the greater improvement among those with worse pre-operative nasal obstruction.
Prior studies have reported no influence of genderReference Sundh and Sunnergren12 or allergyReference Sundh and Sunnergren12,Reference Dinis and Haider17 on septoplasty results up to five years after surgery, which is consistent with our findings. Although we found no long-term studies of the effect of smoking on septoplasty outcomes, a short-term prospectiveReference Yazici, Sayin, Erdim, Gunes and Kayhan18 and a retrospective studyReference Andrews, Jones, Moody, Vincent, Teixeira and Thomas19 found no influence of smoking on nasal surgery results. In our study, smokers, not surprisingly, had significantly more severe nasal obstruction pre-operatively than non-smokers, but both the early and the late post-operative assessments showed similar levels of improvement for both smokers and non-smokers. Thus, the current evidence indicates that gender, allergy and smoking are not important factors in determining either the short- or the long-term results of septoplasty.
Lastly, there was no difference in the proportion of patients reporting crusting, sneezing, secretion or use of nasal medications from the early to late post-operative assessments. Thus, these additional symptoms seem to be largely unaffected by septoplasty at both the early and late post-operative assessment times.
Strengths of this study include its prospective design and high response rates. The fact that it was performed at one hospital minimised variations in the surgical protocol, but may limit the generalisability of the findings. In our clinic of six nasal surgeons, variations in the technique and experience of individual surgeons may have affected the overall results of the clinic, and it is a limitation that these potential confounds were not addressed in this study. However, these variations are most likely to have had an impact at the first post-operative assessment six months after surgery. Patients who reported no improvement or worse results at this assessment were recalled for consultation and additional therapy when indicated. Thus, by the time of the late assessment reported in this study, poor surgical outcomes related to individual surgeons’ technique and experience would likely have been addressed. This does not preclude more subtle effects on surgical outcome related to individual surgeons, and larger studies are needed to evaluate this potential confound.
Another study limitation is that the validated outcome measure used in this study, the Nasal Surgical Questionnaire, differs from measures used in other studies, which may have influenced our findings and could limit their comparability to other study results. Moreover, our primary outcome, the Nasal Surgical Questionnaire's VAS for nasal obstruction, focused on a specific symptom, unlike other studies that assessed outcomes more broadly, including both disease-specific and more general quality of life measures. Although the measure used in this study is valid for the purpose of this study, our symptom-focused approach limits the comparability of our findings to those of other studies.
• Substantial improvement of nasal obstruction was reported at one and four years after septoplasty
• Nasal obstruction worsened slightly, particularly at night, from the first to fourth post-operative year
• This post-operative worsening was similar for septoplasty and for septoplasty combined with turbinoplasty
• Patients aged over 35 years and those with severe pre-operative nasal obstruction reported greater post-operative improvement
• Improvement was slightly better for large versus medium-sized septal deviations, but with no difference based on septal deviation laterality
• Gender, smoking, and nasal allergy did not influence early or late assessments of septoplasty improvements
The data were obtained by two different modes (mail and telephone), and we cannot exclude the possibility that patients might rate their surgical outcomes differently in questionnaires than in telephone interviews. Patients asked to provide subjective retrospective and comparative ratings might be expected to respond more positively when interviewed by hospital staff, particularly by someone they know, than they would if responding to a questionnaire by mail. Therefore, to enhance objectivity and reduce pressure to respond positively in the telephone interviews, the patients in this study were not reminded of their prior ratings, their ratings were numeric, and the interviewers were unknown to the patients. This approach seems to have been effective, as we found that telephone respondents did not respond more positively, and they actually reported significantly less symptom improvement than mail respondents at the early post-operative assessment (early p < 0.01, late p = 0.06). This finding may reflect a tendency for patients with less positive results to avoid mailed questionnaires and only respond when contacted by telephone, a tendency that could lead to biased results in studies that rely only on mail responses.
We plan to continue evaluating these patients in the future, as there is a need for even longer-term prospective studies using numerical ratings of septoplasty results.
Acknowledgement
The study was funded by Lovisenberg Diaconal Hospital, Oslo, Norway.
Competing interests
None declared







