Introduction
Paediatric sleep-disordered breathing covers a spectrum from simple snoring to partial or complete temporary airway obstruction during sleep (obstructive sleep apnoea (OSA)).Reference Loughlin and Carroll1,Reference Bonuck, Chervin and Cole2 UK studies show 12 per cent of 4- to 5-year-old children snore and up to 2 per cent have OSA.Reference Loughlin and Carroll1,Reference Bonuck, Chervin and Cole2 Snoring can cause micro-arousals and impact sleep quality, and obstruction causes sleep fragmentation or even hypoxia.Reference Biggs, Walter and Nisbet3,Reference Primhak and Kingshott4 Paediatric sleep-disordered breathing has been linked to disturbances in concentration and behaviour during the dayReference Mitchell and Kelly5 leading to reduction in academic performance,Reference Galland, Spruyt and Dawes6 quality of life issues for both children and their families,Reference Lee, Kang and Weng7,Reference Torretta, Rosazza and Pace8 and anxiety and concern for the family overnight.Reference Mitchell and Kelly5
A common cause of sleep-disordered breathing is large adenoids and tonsils, and the most common treatment is adenotonsillectomy.9 Around 16 000 paediatric tonsillectomy procedures took place in England in 2016 for OSA, at a cost of £30 million to the National Health Service (NHS), making it one of the most common surgical procedures for children in the UK.9 Surgery has benefits but also risks, especially bleeding, and, in very rare cases, can be life-threatening.Reference Connolly, Tomaselli and McKenna Benoit10 There is also inter-regional variation in UK surgical rates,Reference Suleman, Clark and Goldacre11 in part reflecting variation in natural history: some children have no long-term sequelaeReference Tal, Veloso, Goldbart, Bertrand and Sánchez12 and some improve spontaneously without surgery.Reference Marcus, Moore, Rosen, Giordani, Garetz and Taylor13
There is limited exploration of treatment pathways for paediatric sleep-disordered breathing. A US qualitative study of parentReference Boss, Links and Saxton14 and health professionalReference Boss, Links, Saxton, Cheng and Beach15 decision-making in paediatric sleep-disordered breathing found that parents reported urgently seeking treatment because of fear that their child would stop breathing or because of behavioural or cognitive delays. Tonsillectomy is the third most common surgical procedure in the USA.Reference Wilkes16 In 2011, it was reported that more than 530 000 tonsillectomy procedures were performed in children and adolescents in the USA every year because of recurrent throat infections or sleep-disordered breathing.Reference Randel17 However, according to parents, surgery was often considered as a last resort and parents had explored alternate therapies prior to seeing a surgeon. The authors concluded that shared decision-making, in which parents receive evidence-based information regarding risks, benefits and alternative treatments, may reduce parental decision conflict and improve decision quality.Reference Boss, Links and Saxton14,Reference Boss, Links, Saxton, Cheng and Beach15 However, no decision support tools were generated, and a similar study within the UK context is warranted.
Therefore, we explored the views, concerns and decision-making of UK parents, general practitioners and hospital doctors about sleep-disordered breathing of children in their care. The aim was to better understand the care pathway for these children and determine what is important to well-being and peace of mind for parents and children.
Materials and methods
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. A favourable ethical opinion was obtained from South Central – Hampshire B Research Ethics Committee (reference number: 18/SC/0378), approval to go ahead with the study was obtained from the Health Research Authority (Integrated Research Application System identification: 239892) and research and development approval was received from Newcastle upon Tyne Hospitals NHS Foundation Trust (research and development number: 8841).
Recruitment
A clinical secretary screened upcoming ENT appointments on a monthly basis to identify eligible patients aged 2–9 years with sleep-disordered breathing symptoms. The appointment letter included a study information sheet. At the appointment, parents of patients were invited by their clinician to consent to the collection of a small amount of clinical data about their child and for the parent to complete a validated questionnaire. Patients with serious comorbidities or existing health conditions were excluded. With consent, parent contact details were passed on to the study team who invited them to participate in an in-depth qualitative interview.
Sample
Parents were purposively sampled in order to ensure variation in regard to gender and age of child. General practitioners who might refer children to ENT for sleep-disordered breathing and hospital doctors involved in treating children with sleep-disordered breathing (such as respiratory paediatricians and consultant ENT surgeons) were approached by the study team through known contacts as a convenience sample.
Interviews
All participants were sent a letter confirming their interview along with an information sheet and were asked to sign a consent form prior to the interview taking place. A study identification number was allocated to each participant once consent had been given. Parent participants received a £10 high street shopping voucher to compensate for time and travel expenses. Interviews were carried out either face to face or over the telephone at the convenience of the participant. Interviews lasted up to one hour and were semi-structured based on flexible topic guides (see Figure 1 in the supplementary material, available on The Journal of Laryngology & Otology website).
The topic guides, based on the literature and discussion among the study team, explored symptoms, impact, management and treatment of paediatric sleep-disordered breathing (reported here) plus views about data collection tools and willingness to be randomised into a surgical trial. Interviews, conducted between September 2018 and April 2019 by a trained and experienced qualitative researcher (RMW) who was unknown to the participants, were audio recorded, transcribed verbatim, anonymised and coded following standard procedures of rigorous qualitative analysis.Reference Rapley and Silverman18 Coding was then discussed within the research team as part of the development of the themes presented here.
Results
Participants
Eleven parents, out of 23 approached, consented to participate in the in-depth qualitative interviews (3 declined, 6 were unable to be contacted using the details provided and 3 lost contact before the consent and interview were completed). Five parents were interviewed face to face and six were interviewed by telephone (Table 1). Five general practitioners and six hospital doctors also participated, and most were interviewed over the telephone, with two face to face interviews (Table 2). The emergent themes are presented below, with illustrative quotations.
Table 1. Parent or guardian participants

DIPSP = decision-making in paediatric sleep disorders parent
Table 2. Health professional participants
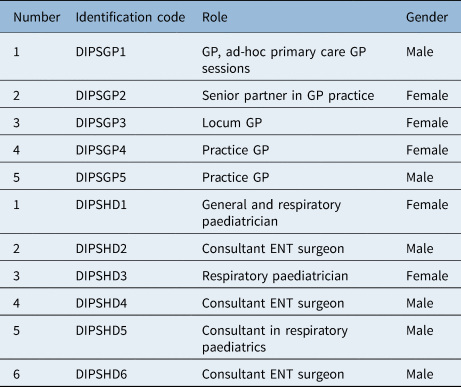
DIPSGP = decision-making in paediatric sleep disorders general practitioner; GP = general practitioner; DIPSHD = decision-making in paediatric sleep disorders hospital doctor
Sleep-disordered breathing identification
All sampled general practitioners recalled regularly seeing adults with sleep-disordered breathing but felt they very rarely saw children with sleep-disordered breathing despite regular paediatric consultations. Our sample of hospital doctors, by nature of their role, regularly saw children with sleep-disordered breathing. In fact, one ENT consultant commented on seeing more patients for sleep-disordered breathing than they did for tonsillitis. This was reported to be as a result of increased patient awareness and the increasingly strict guidelines for the management of sore throat and indications for tonsillectomy:
I've seen more for sleep disordered breathing, rather than tonsillitis now…15 years ago, it would have pretty much all been tonsillitis…the guidelines for not doing as many tonsillectomies for tonsillitis has certainly had an impact, I think. (Decision-making in paediatric sleep disorders, hospital doctor 6)
Parents in our sample fell into one of two distinct categories of lived experience of a child's sleep-disordered breathing. Just over half of the parents knew that there was an issue with their child's breathing at night but had struggled to get the problem acknowledged by their general practitioner. One parent recalled being made to feel dishonest. Although this lack of acknowledgement motivated most parents to push for a referral, it led one parent to stop bringing up the issue:
I just feel like I was never really listened to…we've been to two doctors’ medical groups because we moved and even the first one, they were the same…almost like a brush off, ‘He's fine. Yes, they're big [tonsils] but they're fine.’ I do feel as a parent…when it's your child and you're being ignored that makes you quite annoyed about it, doesn't it? …when I'm pushing for [child's name] and just being ignored you almost then think, ‘I'm just making it up. It's me, I'm making it up. That's not really happening.’ You do start to question whether you're just imagining it, or, you know, is it Munchausen that you have when you push illnesses on your children? … so, I just stopped even mentioning it. (Decision-making in paediatric sleep disorders, parent 1)
The second group of parents in our sample had not considered sleep-disordered breathing as an issue. Their children had either been under hospital investigation for another chronic issue such as hearing loss or had attended hospital for an acute problem such as tonsillitis or a chest infection. Sleep-disordered breathing had emerged during a comprehensive paediatric ENT assessment. A couple of parents recalled feeling guilty about their oversight, although both recounted having previously spoken to their health visitor and having been reassured that there was nothing to worry about:
She's always made a bit of a noise when she was a baby. I just put it down to being normal because nobody told me. The health visitor witnessed her sleeping, and nobody really said, ‘Oh, that's not normal.’ So, I didn't really realise. (Decision-making in paediatric sleep disorders, parent 15)
Parents worry their child will stop breathing
Parents in our sample were unanimous in their concern about the serious night-time consequences of sleep-disordered breathing. Parents described their children as having large tonsils which resulted in snoring and stopping breathing at night:
Just massively enlarged tonsils…he was sleeping in our bed and we noticed that he actually did hold his breath…and he is quite a bad snorer. (Decision-making in paediatric sleep disorders, parent 13)
Parents also spoke about the significant psychological effects on themselves and their child's sibling(s) including anxiety, stress and sleep deprivation from co-sleeping or watching to make sure their child was breathing:
Well, it disturbed my sleep, so it had an effect on me because I was constantly watching her and making sure she was breathing. (Decision-making in paediatric sleep disorders, parent 6)
In addition, many parents reported that their child would be tired in the morning and more prone to mood swings or behavioural issues. Other less frequently cited symptoms included nasal congestion, mouth breathing, poor academic performance, susceptibility to ear or throat infections and bedwetting. Two parents cited problems with hearing as their primary concern.
There was a disconnect in our study between parents being concerned about serious night-time consequences and general practitioners being more worried about the daytime symptoms. For the few children with sleep-disordered breathing that general practitioners could recall seeing, general practitioners reported a variety of physical, behavioural and emotional symptoms, such as tiredness, low mood, irritability, tantrums, lack of concentration, grunting, being spaced out, restlessness, high temperature, reduction in school performance and high rates of upper respiratory infections. General practitioners did however also acknowledge loud snoring, stopping breathing and adopting unusual positions in bed at night. Many of the general practitioners in our sample reported that it was mainly parental worry or family anxiety that triggered further investigation and that many parents wanted things ‘fixed’. General practitioners recalled this was often because of family sleep deprivation with siblings sharing with noisy snorers and parents staying awake to check on their child:
The parents are worried. That's the main thing I suppose…Most of them are quite worried about it and I confirm that there might be some obstruction and they want it sorted really. (Decision-making in paediatric sleep disorders, general practitioner 2)
Some general practitioners felt that they should take more notice of daytime behavioural symptoms as this was often a more common presentation:
If what they're doing is being dozy during in the day and sleeping and bad behaviour…maybe we should have a higher index or suspicion that there's something going on during the night…I think that might be worth eliminating if somebody is presenting with these kinds of symptoms. (Decision-making in paediatric sleep disorders, general practitioner 2)
Hospital doctors in our sample made a very clear distinction between night-time and daytime symptoms, relying primarily on those experienced during the night. The most common night-time symptoms were reported to be regular night-time waking and snoring, but hospital doctors reported other symptoms such as spells when children stop breathing, restlessness, disturbed sleeping patterns, bedwetting and mouth breathing (with neck extended):
You know, it's often first of all the night-time itself, I usually like to know a little bit about what time they go to bed and what time they wake up to set the context…I then focus on when they're asleep as to whether they are noisy or not and then trying to ascertain whether it's snoring or something else…then we get into the morning time symptoms. How easy are they to wake up, are they full of beans and full of life? (Decision-making in paediatric sleep disorders, hospital doctor 5)
Hospital doctors were naturally cautious when only behavioural symptoms were reported:
The most common reason that they would come and see me…would be that they're waking, all the time, through the night, and coming into the parents’ room. But in my experience, that's more often behavioural than OSA. (Decision-making in paediatric sleep disorders, hospital doctor 1)
Daytime symptoms were reported by hospital doctors to include tiredness, irritability, naughtiness, picky eating, difficulty breathing and hyperactivity. Reduced academic performance, inattention and poor behaviour at school were also reported by hospital doctors as symptoms but of less importance to overall diagnosis as this could be a result of several different factors:
I always ask about how they're doing at school, but I think, in the kids we see, there are so many variables feed into how they do at school that, again, it's difficult to say how much is due to their sleep and how much isn't. (Decision-making in paediatric sleep disorders, hospital doctor 3)
Other symptoms reported by hospital doctors included upper respiratory infections, runny nose, tonsillitis, very large tonsils or adenoids, delayed growth, and failure to thrive. Once again parental anxiety featured heavily in a hospital doctor's account of reported symptoms:
Usually, when a child's got sleep-disordered breathing, the parents have got a bit of sleep disturbance as well. Sometimes they're overly anxious – well, ‘overly’ depends on the severity of the apnoea, I suppose, but sometimes parents are very anxious. (Decision-making in paediatric sleep disorders, hospital doctor 4)
Referral and diagnosis routes are not always straight forward
In terms of diagnosis, some general practitioners in our sample reported that sleep-disordered breathing would not be their first concern given this combination of symptoms and lack of time within a single consultation. In addition, one general practitioner would want to rule out more serious and rarer conditions (such as leukaemia) first:
It's probably one which I wouldn't go to straight away because there can be so many reasons for this presentation…it's often that they're all intertwined with physical and mental health, and working out what the initial factor may be outside of the scope of the first 10-minute consultation. (Decision-making in paediatric sleep disorders, general practitioner 1)
Hospital doctors in the sample reported identifying children with sleep-disordered breathing whether they had been referred for it or not:
Yes, but more often than not, they're [general practitioners] not referring for that [OSA]. Certainly, in my experience, they refer them with respiratory problems, and then it's something that gets picked up as part of the clinic. The parents say that they snore all the time. (Decision-making in paediatric sleep disorders, hospital doctor 1)
Just over half of the parents reported asking their general practitioner for a referral to ENT where sleep-disordered breathing was diagnosed. One request followed information gleaned from an overnight trip to accident and emergency for tonsillitis while another followed from social media:
So, he had behavioural issues at school…I was doing some reading online, and somebody shared a post on Facebook about the amount of children who are wrongly diagnosed, and it's to do with their sleep pattern. Some of the things that they were talking about was, ‘Does your child snore at night? Does he sleep with his mouth open? Does he have instances where they stop breathing?’ and in all those situations, the answer was yes. So, I went to see the doctor and they saw us pretty much straightaway…she referred him. (Decision-making in paediatric sleep disorders, parent 4)
Three parents had their children referred to ENT by their general practitioner but for hearing problems or tonsillitis, and the children were only subsequently diagnosed with sleep-disordered breathing. One parent, who had spoken to their general practitioner a number of times about their child's sleep-disordered breathing symptoms was eventually referred to ENT and the child was ultimately diagnosed via a recommendation from a hospital allergologist.
We found out he had a peanut allergy two years ago and we've been having the tests with Dr [name] at [local hospital]. The last time we went I mentioned it to her that I thought in the night-time he was really struggling with his breathing again. He's allergic to dust mites as well, so that's another…You know, it all mixes in doesn't it? So, when she looked, she said, ‘Oh yes his tonsils are really big.’ And I said, ‘Yes, but I've said this to the doctor [general practitioner] numerous times and I just kept getting fobbed off,’ and she said, ‘Well I've put it in my notes to the doctor and I'll say that I think he should be referred to ENT’. So sure enough as soon as she did that we got a referral. (Decision-making in paediatric sleep disorders, parent 1)
Modern technology can aid investigation and diagnosis
In terms of investigation, most general practitioners in our sample reported wanting to look in the patient's throat to see if they had large tonsils. However, they might also measure neck size, listen to the chest, take the patient's temperature, take a blood test for thyroid function or request a chest X-ray, but as there are other issues that cause tiredness, some general practitioners would request a full blood count, a ferritin (iron) level and renal function test. Some general practitioners would ask the family to keep a sleep diary to establish the severity and frequency of symptoms including standing outside the child's room to listen to what their breathing was like. For some general practitioners, this would also aid in making a funding request for NHS tonsil surgery access:
So, symptom diary. Not just to check out if anything else is causing the sleep problems, but also if there needs to be a funding request, if you can demonstrate the severity of the symptoms and the feature of the symptoms, that would be really helpful for when the ENT team come, or whoever is seeing the patient in hospital, to complete a funding request. (Decision-making in paediatric sleep disorders, general practitioner 1)
Hospital doctors in the sample were unanimous that they would start with a detailed history of the patient's symptoms, followed by a thorough examination of the child. For those children where the history was unclear, hospital doctors reported requesting sleep studies. These either took place in hospital overnight or with home pulse oximetry. Hospital doctors reported that modern technology was making history-taking much easier as many parents recorded their child's sleep disordered breathing on their smart phones, a sentiment echoed by one of the parents:
Increasingly we ask people if they can, and often they bring it in without being asked, bring us a video of it. That's incredibly helpful if they've managed to capture the top part of the child and you can see their face and neck and top chest. The top of the chest you can often tell quite a lot by watching, so that's useful. (Decision-making in paediatric sleep disorders, hospital doctor 5)
Some parents had done their own investigating either by searching online, reading literature provided by the doctor or by asking friends for their experience. However, other parents reported they either did not want to, or did not need to, do any research as they had experienced similar symptoms themselves or had another child with similar symptoms:
I'm more one for going to the doctor and seeing what they say. I've got my own health problems at the minute and I don't think Dr Google is always what it's cracked up to be. (Decision-making in paediatric sleep disorders, parent 15)
Patient weight
Many of the general practitioners in the sample talked about the issue of sleep-disordered breathing and weight and that if the child was overweight, they would suggest weight loss and only refer for further investigation if the child had a normal body mass index. Weight was also raised as an issue by a couple of the hospital doctors and was a reason to discuss potential issues with sleep; however, it was also a reason not to refer for surgery. Parents did not talk about their child's weight in any of the interviews.
Adenotonsillectomy is the treatment of choice
In the first instance, general practitioners in our sample would advise diet and lifestyle changes plus weight loss and making sure bedding was allergy free and positioned so that the child's head was upright as well as trying different sleep positions. Some general practitioners felt that another option might be a steroid nasal spray, commonly used for adults with congestion, but only within the permitted age groups and only if they were proven effective in children. For children with an uncertain aetiology or a clear history of OSA, or if the symptom diary showed a disrupted sleep pattern and altered behaviour during the day, then general practitioners would request a referral for further investigation. General practitioners reported that parents of children with sleep-disordered breathing simply wanted to be referred, and like most patients, were looking for a quick fix:
So, ‘I have these symptoms. Well, I need to have an operation, or I need a pill. (Decision-making in paediatric sleep disorders, general practitioner 1)
General practitioners reported making a shared decision with parents to refer patients for a definitive diagnosis from an ENT specialist early on. General practitioners would explain to parents that a referral was for further investigation or management, explaining that there may or may not be the need for an operation under general anaesthetic with the associated risks such as bleeding, sore throat and infection. General practitioners also reported the importance of involving children in the decision-making process by giving them age-appropriate explanations of what might happen. Although general practitioners reported that parents worried about the risks of surgery, this concern was outweighed by the fear that their chid might stop breathing:
…’I'm just so worried that they'll stop breathing at night.’ That fear, I think, seems to outweigh, for most parents, the risk of surgery. (Decision-making in paediatric sleep disorders, general practitioner 3)
General practitioners also felt that as a child's anatomy would change, and if they were more prone to snoring at a young age, then watchful waiting might be the best option. Despite this, general practitioners felt it was important to let parents know that they were taking their concerns seriously and would review patients being treated via watchful waiting:
‘…so, they don't feel they are just being abandoned’ (decision-making in paediatric sleep disorders, general practitioner 2).
General practitioners felt they had limited treatment options other than watchful waiting or referral:
There's a limit to what you can do, really. It's either wait and see or refer. (Decision-making in paediatric sleep disorders, general practitioner 3)
For hospital doctors in the sample, where there was clear indication of sleep-disordered breathing, the primary treatment choice was adenotonsillectomy. Despite clearly explaining the associated risk, such as bleeding, infection and anaesthetic risks, hospital doctors reported that this was often the preferred treatment option for parents too. For less clear cases, most hospital doctors reported a more cautious wait and see approach. Despite being the lowest risk treatment strategy, hospital doctors reported watchful waiting was often the most difficult strategy to recommend:
So sometimes doing nothing is the safest thing to do but isn't the easiest thing to persuade people to do. (Decision-making in paediatric sleep disorders, hospital doctor 5)
Other treatments, each mentioned by a single doctor, included antibiotics, nasal steroids and positioning to prevent children sleeping on their backs.
Most parents in the sample were (pleased to be) offered an adenotonsillectomy for their child, and many of them recalled having been informed of the associated risks and benefits. The remaining couple of parents were happy to either have their child monitored via a sleep study or to wait and see if their child grew out of their symptoms. Previously, parents had managed their child's sleep-disordered symptoms with decongestants, pain relief, antibiotics and other measures including leaving the window on a night vent, propping their child up with pillows, giving reassurance and being relaxed about food avoidance.
More information is needed
General practitioners in the sample suggested that more education for teachers and health visitors might help in highlighting the symptoms of sleep-disordered breathing:
…more education for health visitors, because I suspect they're the group that probably are at the best position to identify it…because they're the ones; they're the ones that will get the parents saying they don't sleep. (Decision-making in paediatric sleep disorders, general practitioner 3)
Hospital doctors in the sample suggested more information should be made available for parents and children because much of the literature was focused on sleep-disordered breathing in adults:
I don't know whether there is enough information out there to be honest. It's dominated by the adult market, I think. Very dominated. (Decision-making in paediatric sleep disorders, hospital doctor 5)
While one parent thought that guidelines targeted at general practitioners would be useful:
Maybe it's just something they're [general practitioners] not, not, not trained in…just to help have some guidelines probably. (Decision-making in paediatric sleep disorders, parent 1)
Discussion
Our research echoes that from the USA,Reference Boss, Links and Saxton14,Reference Boss, Links, Saxton, Cheng and Beach15 in that parents sought treatment for paediatric sleep-disordered breathing because of fear that their child would stop breathing. However, it differs in that, in our sample, surgery was considered the treatment of choice in the UK whereas it was considered a last resort in the USA.
• Sleep-disordered breathing is common, and obstructive sleep apnoea (OSA) may affect up to 1 in 30 children
• Paediatric OSA can have serious consequences if left untreated, but children may present with behavioural problems and poor attention
• Obesity is a risk factor and is thought to be responsible for rising levels of paediatric OSA
• General practitioners reported rarely seeing children with sleep-disordered breathing despite hospital doctors regularly seeing this condition
• Routes to referral and diagnosis were not straightforward but modern technology, such as smart phones, aided investigation
• Adenotonsillectomy was the treatment of choice particularly for parents
Despite general practitioners being asked to be vigilant for paediatric OSA,Reference Harrison, Edmiston and Mitchell19 the general practitioners in our study reported rarely seeing children with sleep-disordered breathing. Our findings are consistent with other research evidence that has shown that general practitioner consultations can result in under reporting of sleep problems in children. For example, in one study, parents reported that general practitioners raised sleep problems in only 10.1 per cent of symptomatic children.Reference Blunden, Lushington and Lorenzen20 Another study reported that only 15 per cent of symptomatic children from two community-based general paediatric clinics had documentation of sleep problems in case notes, with diagnosis recorded in 2 per cent and treatment not recorded at all.Reference Chervin, Archbold, Panahi and Pituch21 A further study reported that only 34 per cent of US paediatricians were confident in evaluating sleep problems in children and adolescents, with only 25 per cent confident to treat them.Reference Owens22
Other research has also highlighted problems with securing appropriate general practitioner referral to ENT. In one study, parents of children experiencing recurrent sore throat and tonsillitis also reported the need to request or even demand referral for the surgical removal of the child's tonsils.Reference Lock, Baker and Brittain23 Adult ENT patients experiencing recurrent sore throat have also reported negotiating the potential barriers facing them in accessing treatment.Reference McSweeney, Rousseau, Wilson, Wilkes and Haighton24
It was interesting to note that modern technology was reported to aid investigation in our study. With the emergence of coronavirus disease 2019 (Covid-19) and guidance published in January 2021 by the World Health Organisation recommending ‘use of pulse oximetry monitoring at home as part of a package of care’,25 there has been widespread enthusiasm for, and ownership of, pulse oximeters by lay people, with many people with acute Covid-19 learning how to use a pulse oximeter and willing to take regular readings.Reference Greenhalgh, Knight, Inda-Kim, Fulop, Leach and Vindrola-Padros26 An increase in use of paediatric pulse oximeters at home may consequently increase the identification of symptoms related to sleep-disordered breathing by parents.
There was a clear disconnect in our study between parents being concerned about serious night-time consequences of paediatric sleep-disordered breathing and general practitioners being more worried about the daytime symptoms. Similar disparities have been reported between physician and adult patients’ perceptions of the problems of habitual snoring.Reference Scott, Ah-See, Richardson and Wilson27 Although general practitioners have recently been encouraged to focus on daytime symptoms,Reference Harrison, Edmiston and Mitchell19 we found that the hospital doctors in our study made a very clear distinction between night-time and daytime symptoms, relying primarily on those experienced during the night. Some general practitioners in our study also reported that sleep-disordered breathing would not be their first concern given the combination of symptoms and lack of time within a single consultation.
Our results confirm the views of Savini et al. that there is a need to increase clinician awareness of paediatric OSA to reduce the rate of late diagnosis and avoid OSA-related sequelae.Reference Savini, Ciorba, Bianchini, Stomeo, Corazzi and Vicini28 The NHS patient website does not refer directly to sleep-disordered breathing but only to OSA, and there is no information specific to children (https://www.nhs.uk/conditions/sleep-apnoea/). Although the NHS site recommends consulting a general practitioner who ‘may refer to a specialist sleep clinic for tests’, the ‘gold standard’ treatment for adult OSA is continuous positive airway pressure (CPAP),29 but this is not well tolerated by children.Reference Savini, Ciorba, Bianchini, Stomeo, Corazzi and Vicini28 According to the National Institute for Health and Care Excellence (NICE) children should be referred to a paediatric ENT specialist if they have clinical features of adenotonsillar hypertrophy, symptoms of persistent snoring and features of OSA syndrome.30 NICE also state that secondary care treatment for OSA in children with clinical evidence of adenotonsillar hypertrophy should be adenotonsillectomy but that CPAP may need to be considered in rare cases where adenotonsillectomy is contraindicated or not likely to be beneficial.Reference Powell, Kubba, O'Brien and Tremlett31
Guidelines for the management of OSA are only available for adult patients.32 In the current study, parents suggested a need for guidelines for general practitioners to aid diagnosis of sleep-disordered breathing in children. This is particularly important as general practitioners are well placed to identify and refer children with sleep-disordered breathing. In contrast, general practitioners reported that more education and training should be aimed at health visitors and teachers who, they believed, were more likely to see first-hand the symptoms of sleep-disordered breathing. Therefore, multidisciplinary guidelines for the management of OSA in children may be needed.
This paper reports the first qualitative study to investigate parent and health professional decision-making in paediatric sleep-disordered breathing in the UK. Data are based on 22 in-depth qualitative interviews carried out by an experienced qualitative researcher, but the research was carried out in only one geographical location, and the sample of parents included only one father. Further research is needed within other regions and with a greater variation in sample.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0022215121004242.
Acknowledgements
We thank all the parents, hospital doctors and general practitioners who participated in this research. This work was supported by the Newcastle upon Tyne Hospitals NHS Charity. The authors have no competing financial interests.
Competing interests
None declared




