Section 1: Otolaryngology
Introduction
The Lancet Commission on Global Surgery has highlighted issues relating to the provision of affordable surgical and anaesthesia care in low- and lower- to middle-income countries.Reference Meara, Leather, Hagander, Alkire, Alonso and Ameh1 Their recommendations suggest that a trained surgical provider is required to achieve this; furthermore, international non-governmental organisations need to integrate with local training programmes and accept an educational role to their work. Non-governmental organisations need to have training components integrated into their programmes to ensure the durability of their effect, with the ultimate goal of high-quality training being achieved in-country in a self-sufficient manner. In exploring possibilities for innovation, it is noted that low-cost simulation is one way to develop and ensure competency that is not at the expense of patient care or scarce hospital supplies.
Simulation
The acquisition of competencies can be accelerated by simulation practice, thereby reducing training time.Reference Bhutta2 Such simulation, with some healthy imagination, can be low in cost. In addition, it has the advantages of being readily available, and unconstrained by students’ or trainees’ working hours.
Temporal bone dissection
This model of simulation would still be considered the ‘gold standard’ for ear surgery training (Figure 1). Many dissection manuals are freely available on the internet, to guide trainees through the surgical anatomy, negating the need for continuous direct supervision or instruction.3

Fig. 1. Temporal bone dissection course at Mulago Hospital, Uganda.
Basic requirements to provide a temporal bone dissection course include: a ready supply of cadaveric temporal bones, trainers (local and/or visiting faculty), equipment and space to run the course.
In some lower- to middle-income countries, cadaveric temporal bones may be easier to acquire, though not always; in some cultures, the use of cadaveric material may be culturally sensitive and even considered taboo. Notwithstanding the above, screening of cadaveric supplies for infectious diseases would be required considering that the specimens are aerosolised by drilling. Screening may or may not be routine practice in the under-resourced areas.
In lower- to middle-income countries, equipment may be the most challenging hurdle. In many scenarios, there may be insufficient equipment for the operating theatre, let alone for a dissection room. The same equipment should not be shared between each site. Basic needs are: an operating microscope, suction, a drill and basic middle-ear instruments. In many lower- to middle-income countries, the power supply is prone to fluctuations. This can lead to blowing bulbs on microscopes and electrical damage to equipment, which in turn may prove difficult or expensive to replace. The use of a surge protector through which the power is channelled can help prevent fluctuations, but is not a guarantee against damage. Furthermore, the power requirements are large, given the amount of electrical equipment required.
Finding a suitable place to run a temporal bone dissection course, with suitable power supply and furniture, may be another stumbling point. Like most resources, space is often limited in low-resource settings.
When the provision or use of cadaveric temporal bones is not feasible, artificial temporal bones may form a useful substitute. One such example is the Pettigrew temporal bone, into which disease processes such as cholesteatoma, tympanic membrane perforations and ossicular chain conditions can be incorporated.4
Three-dimensional printers are becoming much more affordable and may eventually provide a less expensive source for such models. Once an appropriate printer is available, often all that is required is a software addition.
The use of animal models has been researched as a viable alternative to cadaveric supplies. Both bovine and ovine models have some benefits, and may allow for development of technical drilling skills. However, ultimately there are important and significant anatomical differences when compared to human anatomy that will limit the role of these models.
In some parts of the world, hammer and gouge mastoidectomy is still taught and advocated, where there is no access to modern mastoid surgery equipment. In many areas, patients may not be able to afford to travel to larger centres and such techniques could be potentially lifesaving. The Developing World ENT website includes a guide for this technique (along with a wealth of other useful information).5
Other simulation
Whilst computer-generated models and virtual simulation are becoming popular in high-income countries, the cost usually prohibits their use in lower- to middle-income countries. However, innovative simulation models can often teach specific tasks. Numerous simple training models have been devised to teach and enable the practice of ventilation tube insertion, for example.
Taking this a step further, an Ear Trainer has been developed specifically for training the skills required for ear surgery, both with and without a microscope, in the low-resource setting (Figure 2). Importantly, it is affordable up-front and lacks consumable costs.Reference Clark, Westerberg and Mitchell6
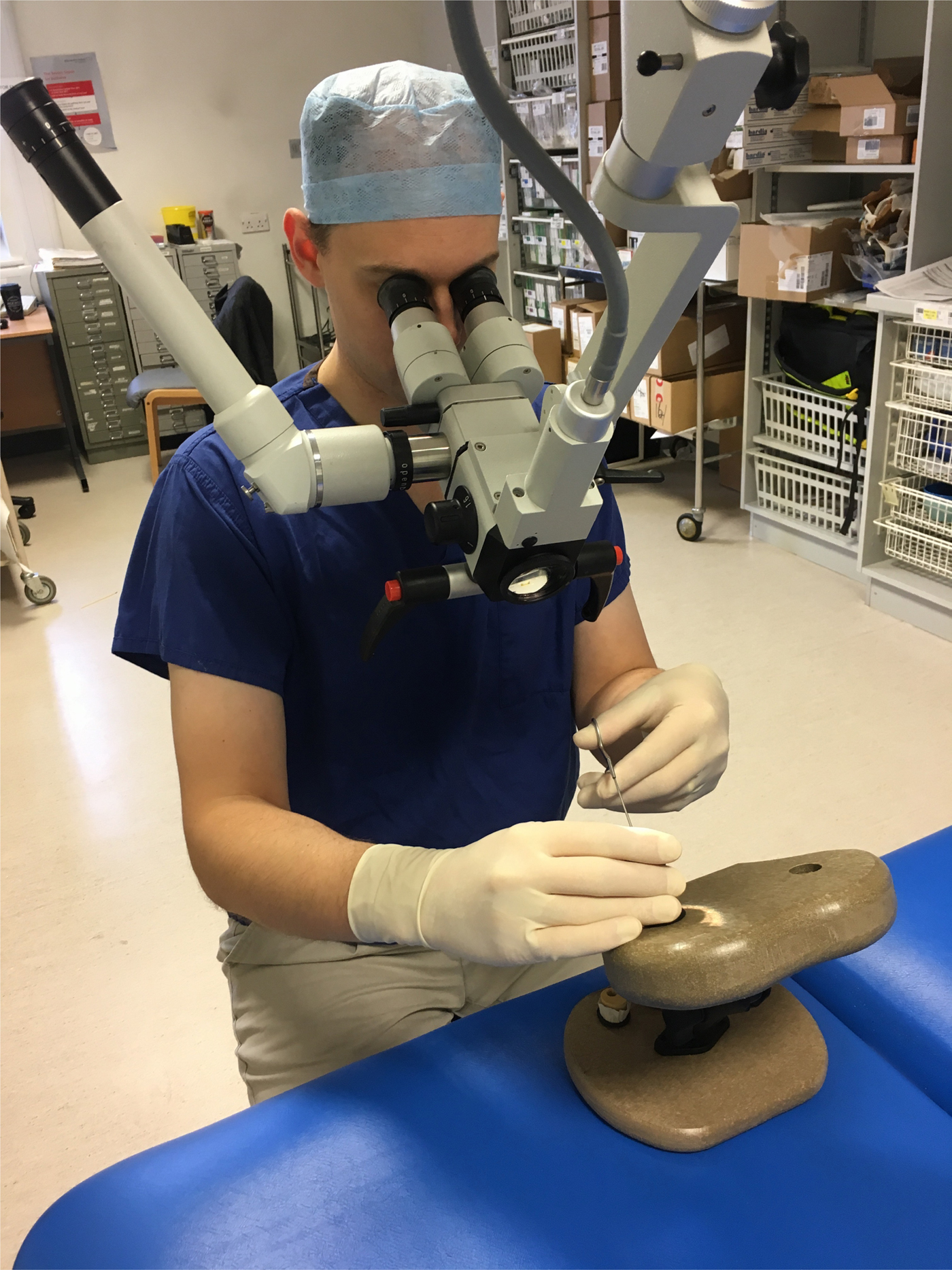
Fig. 2. A low-cost, low-fidelity ear surgery simulator undergoing validation testing.
With a series of accompanying videos demonstrating techniques and skills to practice, the tasks that have been developed (foreign body removal, ventilation tube insertion, tympanomeatal flap elevation, myringoplasty and middle-ear manipulation skills) have been validated. These show that the Ear Trainer simulator is a realistic representation of the ear canal and middle ear, and that experts perform the tasks better than novices. Such validation has been conducted in high-income countries and lower- to middle-income countries, indicating that the simulator is fit for the task. Whether this actual simulator is employed, or the principles and tasks it employs are adapted for use on novel simulators, the end-goal of achieving surgical skill acquisition can be achieved.
Training in lower- to middle-income country settings
Ear camps
A common set-up for delivering otology humanitarian care is the ear camp. This often involves a team of surgeons, anaesthetists, audiologists and nursing staff visiting a place of need for a short period of time in order to undertake a concentrated period of patient assessment and operating, often in conjunction with in-house training and service development.
Such camps should allow for interaction between visiting surgeons and the local team, and are an ideal opportunity to teach. The ear camp should demonstrate good technique, leading by example on the cases encountered, with pre-, peri- and post-operative discussions. They should involve the observation of local trainee operating and hands-on teaching, as is common to all surgical training programmes (Figure 3). In addition, the ear camp should provide the opportunity to run temporal bone dissection courses and tutorials.

Fig. 3. Intra-operative training of the local staff by a visiting team.
However, ear camps are not without their potential pitfalls. They may have a negative impact on local personnel by increasing workload. Furthermore, they may leave behind patients who develop complications that the local faculty have difficulty managing because of a lack of experience or resources. Certainly, they need to be undertaken sympathetically and with consideration. Some camps are largely ‘self-contained’, engage little with local staff, and focus on the quantity of patients being treated to appease donors and funding agencies rather than having a focus on training. Concerning all types of humanitarian care, there are certainly problems to avoid.Reference Welling, Ryan, Burris and Rich7
Focusing the learning objective in these settings is important and necessary to ensure they are in line with the local training needs, being sympathetic to the capabilities and resources of the local staff and to the skills required to manage the local pathology.
‘Brief – intervention – debrief’ is a training technique effective in any setting. An explanation of what is going to be taught or demonstrated is provided, with a pre-intervention assessment, followed by the intervention (or teaching of the skill), with subsequent evaluation. Reflection is arguably the most important of the steps. It is equally important for the visiting faculty to reflect on their experience in the low-resource setting; the ingenuity often required to manage patients with extensive disease in a low-resource setting is transferable to their home institution.
The use of mental practice has been investigated in relation to the provision of surgical care. This concept involves a period of relaxation prior to a procedure, whereby the surgeon recites a mental script that outlines, step-by-step, the surgical approach they are about to undertake. Such an approach has been shown to help an individual learn a cognitive task. Whilst surgery is part a technical skill, the constant decision making – for example, deciding upon which instrument to use next, dealing with different anatomy or unexpected pathology, managing the team around you, and guiding an assistant – means that in reality surgery is a complex cognitive task.Reference Mick, Dadgostar, Ndoleriire, Lea, Clark and Westerberg8, Reference Conlin, Lea, Bance, Chadha, Kilty and Kozak9 Mental practice and imagery work well in this scenario, in high- and low-resource settings.
Post-training fellowships
An initiative taken from a successful orthopaedic training model involves getting a trainee who has completed their training (in a high-income country) to undertake a sustained period (four to six months) of work in a low-income country setting.
This has been successful in Cambodia, a country that had a large burden of untreated ear disease with few surgeons trained to manage these patients. The fellowship programme, run from the UK (but open for application from any country) allows a surgeon to provide a sustained period of training to local surgeons who have little or no previous ear surgery experience. The first of these fellowships focused largely on training the local surgeons to perform a successful myringoplasty. The extended period of time allowed for a structured development programme, and the parallel training of an audiologist allowed for follow-up assessments.
This training model has been shown to be effective, and is now progressing to the training of mastoidectomy skills with subsequent fellows.Reference Clark and Huins10 This serves as an example of what might be achievable elsewhere.
Curriculum development and examinations
Whilst education and training in lower- to middle-income countries can be provided by visiting staff from high-income countries, ultimately one will aim for the majority of training to be provided by the local faculty in a self-sufficient training programme. In this way, developing a suitable curriculum will be an important primary step. What is included might reasonably vary from country to country, depending upon local resources and pathology.
Formative assessment of trainees in lower- to middle-income countries is performed less frequently than in high-income countries. This is at least partly explained by the sheer volume of clinical care required for them to provide.
The National In-Training Exam from Canada has been taken to Uganda. This allowed local trainees to see how they compared to Canadian residents, and may have served as a useful example or inspiration, or at least provided a formative assessment when few existed.
Review of these examinations assists the local programmes in assessing and improving existing curricula content. However, direct transfer of national in-training examinations from high-income countries to lower- to middle-income countries may not differentiate progress as well as in high-income countries, given the different emphasis during residency training (article in preparation – communication from author DN). Anecdotally, one criticism of high-income country examinations is their emphasis on theoretical concepts at the expense of practical knowledge assessment.
Competency-based training and assessment
Recently, high-income country training programmes have embraced competency-based training and assessment. For example, in 2005 in the UK, as part of the Modernising Medical Careers programme for post-graduate medical training, such changes were implemented through government policy. In 2017 in Canada, ENT trainees converted from ‘time-based’ residency programmes to ‘competency-based’ medical education, through a Royal College of Physicians and Surgeons of Canada initiative. This was in part a response to reduced junior doctor working hours with increased workload intensity, which had resulted in a reduced opportunity for personal reflection and feedback from colleagues.
Arguably, training programmes in lower- to middle-income countries have been using a competency-based medical education format for training. Junior residents are required to gain competency in the assessment and management of patients with surgical disorders by necessity. The sheer volume of clinical cases necessitates that trainees become competent early, in order to manage many conditions with little direct supervision. In many respects, high-income country training programmes could learn from their experience in this area.
Training in high-income settings
Fellowships
There are many examples where surgeons from low-resource settings obtain additional training through a high-income country setting. This is often informally arranged, though restrictions on visas, income and effects on local training programmes are logistical issues that can prevent such plans from materialising. It is important, in order for maximum benefit to be obtained, that an educational licence (or its local equivalent) is sought, such that the individual can function as a trainee under supervision rather than simply as an observer.
A theoretical concern is that those exposed to such training may be reluctant to return to their home country, but instead be attracted to the higher potential earnings and status of high-income countries. The ‘push’ and ‘pull’ factors surrounding this issue are complex and not easily addressed. However, one possible solution is to ask the faculty to sign ‘institutional bonding forms’, which state that the individual will return and serve in their home departments following training.Reference Kasper and Bajunirwe11
Addressing the objectives of the fellowship at the outset is important to manage the expectations of all involved. Such fellowships should allow an individual to: see how things can be done when appropriate resources are available, learn techniques that were otherwise not taught in the local programmes and provide inspiration for when they return home. This will apply not only to the clinical experience they obtain, but also to how a successful training programme can run.
Practically speaking, the authors have not had the experience of trainees not wanting to return to treat patients in their home countries, and there has been no need for any bonding contracts. This might well have been helped by promises of faculty appointments and opportunities for promotion once the additional training had been completed, and by the mentoring relationships gained during the training abroad.
Medical Training Initiative
The Medical Training Initiative is intended for suitably qualified overseas post-graduate specialists. These individuals undertake a fixed period (usually one to two years) of training in the UK before returning to their own healthcare systems. For ENT trainees, this is organised through ENT UK.12 Specifically, the trainee is appointed into a recognised training post within the National Health Service. They are given appropriate supervision and education to enable them to acquire useful and suitable skills and knowledge. Trainees receive the same quality of training as UK trainees. Similar examples exist in other high-income countries.
Distance learning and online resources
There are numerous useful resources available freely through the internet, to guide and teach the aspiring otologist. Open access journals, for example, are available online to the reader, without financial, legal or technical barriers, other than those inseparable from gaining access to the internet itself. Many institutional libraries have been given special or complimentary access to various databases and resources that are otherwise not free.
An example of such work relates to Professor Johannes Fagan's Open Access Atlas of Otolaryngology, Head and Neck Operative Surgery,13 and his Open Access Guide to Audiology and Hearing Aids for Otolaryngologists.14 Fagan made these texts available in recognition of the fact that an operative text book might cost colleagues working in some countries as much as two months’ salary. The articles have already been downloaded more than 1.2 million times, and continue at a rate of 1 download every minute. With translations in French, and some chapters in Portuguese and Spanish, the target audience is growing. The texts have no copyright restrictions, and readers are encouraged to copy and quote from them. The ability to track what is downloaded allows the authors to assess which chapters are best received and which are the most popular topics. This resource is an excellent example of what can be achieved. It is proving to be increasingly available to most parts of the world, and simply requires the reader to have internet access.
Many high-income countries have global health organisations with corresponding websites that contain an array of educational resources.15–18
Distance learning courses can also provide education, and may be of particular benefit to high-income country surgeons wishing to undertake work in the humanitarian care setting. The University of British Columbia, for example, has a Branch of International Surgical Care, with online courses on: surgical care in international health; global disability and surgical care; surgical care in humanitarian disaster response; and programme planning and evaluation, with a surgical care focus.
These courses, and others soon to be offered, can be combined for a Certificate in Global Surgical Care or a Master's degree in global surgical care. All courses are fully online, designed for a busy professional to learn in their own time. This format also facilitates collaborative discussions between surgeons from high-income countries and those from lower- to middle-income countries.
Other training needs
Most of the focus on training has traditionally been about the acquisition of clinical skills and knowledge. However, to develop a local service programme, managerial skills are also required.
Regarding leadership training, clinicians need to have skills to help them establish, administer and expand their service programmes. This will include training on how to appeal for resources, present a business case for new equipment or new facilities, and/or other leadership skills. Skills are required to negotiate contracts with companies, including warranties, service contracts and training. Team-building skills should help any developing team.
Concerning physical wellness, physician burnout, and its corollary physician resilience, is of growing interest in surgical divisions within high-income countries. It is recognised that surgeons (and other medical personnel) are prone to burnout, given the often immense workload and long hours. This is conceivably of even greater concern in lower- to middle-income countries, where the burden of disease is considerable relative to the human resources available to manage these patients. Surgeons in lower- to middle-income countries are an invaluable resource that needs to be supported. That notwithstanding, anecdotally, coping skills and resilience in surgeons in lower- to middle-income countries are more highly developed. These skills are arguably transferable to surgeons in high-income countries.
The importance of research has become an increasing priority in lower- to middle-income countries. Aside from obvious benefits in improving the provision of care to patients, research can help trainees advance their career and can increase international awareness of local institutions. Rightly or wrongly, the adage ‘publish or perish’ has been largely adopted by institutions in lower- to middle-income countries. Unfortunately, although the areas of research are still readily available and the interests of researchers are high, the funding opportunities are not always forthcoming, especially in lower- to middle-income countries. Collaborative research has proven helpful in overcoming such hurdles. Such opportunities allow doctors in resource-limited settings to be involved in research, acquire more publications and at times earn supplemental income. The collaborators, on the other hand, find an avenue to get involved in global health and humanitarian activities, and gain an additional learning opportunity.
Case study: training in Uganda
ENT surgical outreaches to Uganda have been ongoing for about 15 years. Initially, there was only one ENT residency programme in Uganda. A second programme started in 2010, with support from international collaborations. Visiting teams continue to provide medical and surgical care to the patients who need it, but focus on providing hands-on training to local faculty and trainees. Local faculties prefer this approach, as limited experience in several areas of the discipline are supplemented by interaction with international subspecialised surgeons. The visiting faculty also play a large role in increasing exposure of the local teams to advances in the discipline, such as endoscopic sinus surgery and ear surgery, which have been better embraced now. The visits also contribute to ground-breaking work. For example, through such outreach programmes, the first cochlear implant surgery was performed in Uganda in 2008.
Access to faculty and educational materials from well-established institutions in high-resource countries augments the local teaching faculty and the educational curriculum. For instance, shifting the teaching curriculum to module-based training has allowed the visiting faculty to focus on the transfer of specific skills during a relatively short visit.
Limitations in operating theatre access and associated infrastructure have necessitated the use of simulation. These usually involve low-cost, low-fidelity models that focus on the improvement of hand–eye co-ordination skills under a microscope. Practice with models like the Ear Trainer has enhanced the otomicroscopy skills of the junior residents. This has translated into self-perceived improvements regarding the clinical examination of patients and technical skills in the operating theatre.
Resident and faculty exchange programmes have focused on the acquisition of different skills and knowledge. Over the years of collaboration, Uganda has benefitted from the training of three otologists and two rhinologists through fellowship programmes, and currently these specialists serve as faculty in the different programmes in Uganda. In addition, there has been an increase in the quality and number of research publications through the collaborations.
The Royal College of Physicians and Surgeons of Canada developed the ‘CanMEDS’ framework, which identifies and describes the abilities physicians require, a framework that is not unique to high-resource countries. Exchange programmes have allowed first-hand experience with this framework in an educational environment, leading to its adoption in Uganda. Additionally specific to Uganda, observing the integration of training programmes across a high-resource country (via the national Royal College of Physicians and Surgeons of Canada) has challenged Ugandan surgeons to share resources between the two otolaryngology residency programmes in the country, such as the temporal bone dissection laboratory. This will hopefully ultimately involve a unified student matching programme and a common final examination at the end of the training.
An important, yet often unrecognised benefit of visits by outside surgeons is the influence it has on team building, from preparation for the visit, to interaction between the teams, or even formal scheduled talks on team work and career building. These aspects of surgical care provision are often overlooked in an environment that struggles simply with the volume of patients requiring care.
Section 2: Audiology
Introduction
Audiologists are primarily the health professional of choice in dealing with hearing loss, particularly when surgical or pharmaceutical interventions are no longer an option. They also provide an essential service in supporting ENT surgeons undertaking ear surgery, in both helping to select those patients suitable for surgery and in assessing the outcomes and success of that surgery, providing an invaluable quality control check.
Audiology is a relatively new profession in several parts of the world, particularly in lower- to middle-income countries, where a single audiologist could be serving a population of millions. For example, Malawi, with a population of 12.5 million people, currently has only 2 native ENT specialists and 1 volunteer audiologist from the USA. They currently have four Malawian trainees studying for a Master's degree in audiology through a UK university.19 Malaysia, with a population of just over 30 million, requires 100 new audiologists to be trained annually over the next 20 years in order to meet health service demands.20 China has approximately 2000 audiologists for a population of 1.3 billion, with other hearing care professionals also providing hearing care. In comparison, the Bureau of Labour Statistics in America reported, in 2016, that between 12 000 and 13 000 audiologists were currently employed (excluding self-employed audiologists), with an additional 3800 audiologists required over the next 7 years to meet their demands.Reference Aidil, Dzulkarnain, Pandi, Rahmat and Zakaria21
Audiologists, however, are not the only healthcare professionals dealing with patients who have ear-related or hearing issues. In high-income countries such as the UK, USA, Australia and New Zealand, tertiary education is the required entry route to the profession. Professional and registration bodies contribute to the training curricula, and set minimum qualification and skill requirements for those diagnosing and treating hearing loss. In low- to middle-income settings, this privilege is not afforded to the majority of the estimated 360 million people living with hearing loss around the world.22 Ear and hearing healthcare can be provided by anyone, including primary healthcare workers, community-based workers, technicians, teachers at schools for the deaf, nurses, ENT specialists, and commercial representatives from hearing aid companies, resulting in a noticeable overlap in the scope of practice amongst all. A survey conducted by Goulios and Patuzzi highlighted this difficulty in defining the range of hearing healthcare providers and professionals in various countries, listing over 20 different titles, with varying job descriptions, all providing care for patients with hearing loss.23
High- versus lower- to middle-income country settings
Hearing loss has not been high on the list of priorities for developing countries. This is unsurprising given the incidence of what are viewed as far more life-threatening conditions such as human immunodeficiency virus (HIV) and malaria, and the perceived unaffordability of hearing rehabilitation methods and technologies. However, it has been increasingly recognised that this view is no longer valid and that the economic burden of hearing loss to all countries cannot be ignored.Reference Goulios and Patuzzi24 This figure has been estimated in the region of 750 billion dollars globally. Unaddressed hearing loss has been shown to pose a significant burden, not just to the healthcare systems in lower- to middle-income countries, but to the economy as a whole. Education, societal costs and loss of productivity are all contributing factors.
In order to address growing needs, and aid training and education, hearing care professionals at various levels in lower- to middle-income countries have had access to the World Health Organization (WHO) training manuals for primary ear and hearing care. The four manuals range from a basic to an advanced level, and include a student handbook. Their provision aimed to reduce the burden of ear disease and hearing loss worldwide.18 However, a more strategic and concentrated effort is required, on a country-by-country basis, to address specific needs.
The initiation of education programmes is essential; these should be affordable and relevant to the demographic they serve. This will require the support of government agencies, policy-makers, professional associations and educational institutions, together with initiatives of organisations like the WHO and the United Nations. This will enable both high- and low-income countries to address and overcome some of the challenges in delivering audiology training, including the lack of audiology and hearing care programmes, the lack of awareness of the profession and of hearing loss itself, and the lack of funding for hearing healthcare.23
Training needs to address evolving issues in hearing loss, such as a growing elderly population, and an increasing incidence and prevalence of hearing loss related to recreational noise exposure. Further, the training of audiologists requires an extensive amount of clinical placement and supervision. This is difficult enough in high-income countries such as the UK, and will be even more challenging in lower- to middle-income countries that have very few centres, if indeed any at all. For example, Bangladesh has audiological services and hearing aid fittings available only in the capital and major cities.25 Goulios and Patuzzi comprehensively address these and many other issues regarding audiology education and training. They proposed a conceptual model that can be used as a first step to develop sustainable and cost-effective education models, which can be adapted for use for varying populations and requirements.23
E-learning and online learning
Telehealth has gained much popularity in the past several years. Its advantages have led to it being considered a service delivery model that increases accessibility and cost effectiveness, in both developed and developing countries, while addressing problems like poor infrastructure and a lack of trained clinicians.
Internet connectivity and mobile telephone technologies are rapidly improving and expanding capabilities for hearing healthcare, allowing the use of smartphones for hearing testing, clinical examination of the ears and remote monitoring.Reference Alauddin, Joarder, Suzuki, Kobayashi and Koga26–29 The use of tele-audiology in education and training is similarly accessible, with the internet making available a plethora of online resources that are free and available on demand, including open access journals, online forums and conferences, and short training seminars (e.g. the British Society of Audiology Lunch and Learn e-seminarsReference Yousuf Hussein, Swanepoel, Biagio de Jager, Myburgh, Eikelboom and Hugo28). Various devices and adaptations to smartphones that enable their use as clinical tools are becoming more commonplace, and therefore more affordable, thus allowing training in remote locations with poor infrastructure (e.g. the Cupris Health PlatformReference Van Tonder, Swanepoel, Mahomed-Asmail, Myburgh and Eikelboom30 and HearScope31). Some of these devices have already been successfully tested in lower- to middle-income countries, making them viable options for education and training in these settings. In addition, a systematic review of simulated learning environment tools for audiology education suggests that the simulated learning environment is an effective tool for basic level training.20
Universities are now also offering Master's degrees in audiology that are completely online. This allows working clinicians to upskill and expand their scope of practice, regardless of their location, as long as they have connectivity, and can do so while still retaining their employment. Shorter courses, certificates and stand-alone modules that enable self-paced learning are also gaining popularity. These also reduce the cost to the individual or employer, as compared to funding a full degree.
Future directions
Audiology as a profession, much like other healthcare professions, will continue to grow and evolve. The challenges we face now are sure to be replaced with new challenges driven by technological changes, an improved understanding of hearing loss and the initiatives of influential organisations such as the WHO. What remains clear and urgent is the dearth of skilled clinicians to address ear and hearing care across the globe.32 Awareness and advocacy of hearing loss are crucial. This can only be achieved with collaborations between policy-makers, educational institutions, professional organisations and commercial organisations of both high- and lower- to middle-income countries, working together to develop and share innovative ways of training and education, and thus address the global burden of hearing loss.
Case study: training at All Ears Cambodia
In 2003, All Ears Cambodia formed as a non-governmental organisation in response to: a severe shortage and maldistribution of ENT and audiology services, a high burden of preventable conditions, and widespread misconceptions about ear care and hearing loss. Cambodia's healthcare system was being rebuilt following collapse across a cruel and torrid history. Many challenges still remain today, including the need to improve upon healthcare coverage, regulation and quality, and to nationally scale up human resources for ear and hearing care using an integrated and equitable approach.
With a determination to reach the hardest hit, All Ears Cambodia targets disadvantaged and high-risk groups such as children with HIV, craniofacial abnormalities or multiple disabilities, street children, women and girls at risk of human trafficking, vulnerable older people, and families on low incomes. Patient referral is co-ordinated through a network of: local and international non-governmental organisations, government hospitals and other healthcare providers, schools, and community partnerships.
Services are delivered by mid-level clinicians specialised in both primary ear healthcare and audiology, whose competencies span microsuction, hearing aid fitting, ear mould manufacturing, nurse training, prevention education and rural outreach, for example. These clinicians are trained and retrained to operate in challenging environments, with a mix of skills required that is well suited to the provision of efficient, quality primary and secondary healthcare services which are aligned to the health needs of the population.
Considerations for this role begin early, at the recruitment stage into the School of Audiology and Primary Ear Health Care at All Ears Cambodia. Flexible selection criteria assist in the formation and nurturing of a more balanced workforce profile that better reflects, understands and serves a diverse population. Training is intensive across the full-time two-year in-house course. The course comprises daily clinical mentoring from the outset, and frequent tutorials, practical sessions, assessments and rural outreach visits. A close relationship between the training environment and subsequent job requirements helps to foster the necessary attributes required for a smooth transition into a demanding role.
The strong culture of continuing professional development at All Ears Cambodia is not commonly found across the country, yet it is doubly important owing to a multitude of factors that are amplified in Cambodia. Such factors include pre-service education quality, foreign language literature, rural professional isolation, clinician motivation, case complexity among target groups and the birth of relatively new professions such as audiology.
The very first cohort of trainees that graduated over a decade ago are now senior clinicians actively engaged in the teaching and management of the next generation of clinicians at All Ears Cambodia. As interest in ear and hearing care begins to grow, their experience and leadership will be invaluable in continuing to influence the national agenda, to ensure care reaches all Cambodians.
Acknowledgements
Ned Carter, past Head of School at All Ears Cambodia, Phnom Penh.
Competing interests
None declared





