Published online by Cambridge University Press: 21 September 2023
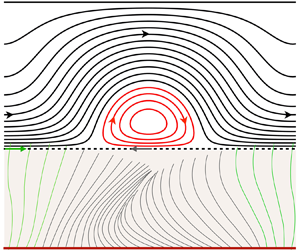
We present numerical and analytical predictions of mucociliary clearance based on the continuum description of a viscoelastic mucus film, where momentum transfer from the beating cilia is represented via a Navier-slip boundary condition introduced by Bottier et al. (PLoS Comput. Biol., vol. 13, issue 7, 2017a, e1005552). Mucus viscoelasticity is represented via the Oldroyd-B model, where the relaxation time and the viscosity ratio have been fitted to experimental data for the storage and loss moduli of different types of real mucus, ranging from healthy to diseased conditions. We solve numerically the fully nonlinear governing equations for inertialess flow, and develop analytical solutions via asymptotic expansion in two limits: (i) weak viscoelasticity, i.e. low Deborah number; (ii) low cilia beat amplitude (CBA). All our approaches predict a drop in the mucus flow rate in relation to the Newtonian reference value, as the cilia beat frequency is increased. This relative drop increases with decreasing CBA and slip length. In diseased conditions, e.g. mucus properties characteristic of cystic fibrosis, the drop reaches 30 % in the physiological frequency range. In the case of healthy mucus, no significant drop is observed, even at very high frequency. This contrasts with the deterioration of microorganism propulsion predicted by the low-amplitude theory of Lauga (Phys. Fluids, vol. 19, issue 8, 2007, 083104), and is due to the larger beat amplitude and slip length associated with mucociliary clearance. In the physiological range of the cilia beat frequency, the low-amplitude prediction is accurate for both healthy and diseased conditions. Finally, we find that shear-thinning, modelled via a multi-mode Giesekus model, does not significantly alter our weakly viscoelastic and low-amplitude predictions based on the Oldroyd-B model.