Published online by Cambridge University Press: 19 December 2023
In this paper, we present an analytic solution for pulse wave propagation in a flexible arterial model with tapering, physiological boundary conditions and variable wall properties (wall elasticity and thickness). The change of wall properties follows a profile that is proportional to  $r^\alpha$, where
$r^\alpha$, where  $r$ represents the lumen radius and
$r$ represents the lumen radius and  $\alpha$ is a material coefficient. The cross-sectionally averaged velocity and pressure are obtained by solving a hyperbolic system derived from the mass and momentum conservations, and they are expressed in Bessel functions of order
$\alpha$ is a material coefficient. The cross-sectionally averaged velocity and pressure are obtained by solving a hyperbolic system derived from the mass and momentum conservations, and they are expressed in Bessel functions of order  $(4-\alpha )/(3-\alpha )$ and
$(4-\alpha )/(3-\alpha )$ and  $1/(3-\alpha )$, respectively. The solution is successfully validated by comparing it with numerical results from three-dimensional (3-D) fluid–structure interaction simulations. Subsequently, the solution is employed to study pulse wave propagation in an arterial model, revealing that the wall properties and the physiological outlet boundary conditions, such as the resistor–capacitor–resistor (RCR) model, play a crucial role in characterizing the input impedance and reflection coefficient. At low-frequency range, the input impedance is found to be insensitive to the wall properties and is primarily determined by the RCR parameters. At high-frequency range, the input impedance oscillates around the local characteristic impedance, and the oscillation amplitude varies non-monotonically with
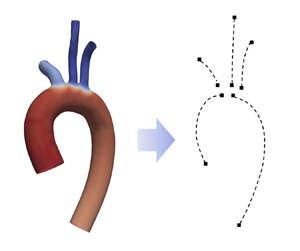
$1/(3-\alpha )$, respectively. The solution is successfully validated by comparing it with numerical results from three-dimensional (3-D) fluid–structure interaction simulations. Subsequently, the solution is employed to study pulse wave propagation in an arterial model, revealing that the wall properties and the physiological outlet boundary conditions, such as the resistor–capacitor–resistor (RCR) model, play a crucial role in characterizing the input impedance and reflection coefficient. At low-frequency range, the input impedance is found to be insensitive to the wall properties and is primarily determined by the RCR parameters. At high-frequency range, the input impedance oscillates around the local characteristic impedance, and the oscillation amplitude varies non-monotonically with  $\alpha$. Expressions for the input impedance at both low-frequency and high-frequency limits are presented. This analytic solution is also successfully applied to model flow inside a patient-specific arterial tree, with the maximum relative errors in pressure and flow rate never exceeding
$\alpha$. Expressions for the input impedance at both low-frequency and high-frequency limits are presented. This analytic solution is also successfully applied to model flow inside a patient-specific arterial tree, with the maximum relative errors in pressure and flow rate never exceeding  $1.6\,\%$ and
$1.6\,\%$ and  $9.0\,\%$ when compared with results from 3-D numerical simulations.
$9.0\,\%$ when compared with results from 3-D numerical simulations.