Introduction
Development and consequent licensing of new drugs and devices are highly regulated processes. As greater insight into biologic mechanisms has been gained and multiple therapeutic targets identified, the complexity of both clinical trial protocols and the regulations and guidelines required to manage clinical trial activity have increased [1]. To meet this challenge, clinical research personnel must be adequately trained to execute clinical trials. The most recent version of the Declaration of Helsinki acknowledged this by stating that “[m]edical research … must be conducted only by individuals with the appropriate ethics and scientific education, training and qualifications” [2]. This emphasis on training aligns with two of the primary objectives of the Clinical and Translational Science Award (CTSA) Consortium as follows: to provide a high caliber, national platform for executing large-scale, high-quality clinical trials and to ensure the workforce has the skills and knowledge necessary to advance translation of discoveries via clinical trial execution.
An important asset across the various CTSA hubs is diversity in many dimensions; however, diversity is not desired in either the knowledge base or the scientific quality of clinical trial execution. Consistent requirements for providing training to ensure an appropriate level of qualification do not exist. We hypothesized that many aspects of clinical trial implementation will be significantly improved by articulating standard practices and by ensuring uniform approaches to training and qualification for clinical research professionals who are the fundamental human asset of clinical trial execution. Achieving this goal would systematically harmonize both training and, consequently, performance outcomes for professionals actively engaged in the clinical trial enterprise. Once established and validated, we believe a training and qualification strategy could be efficiently implemented across all CTSA Consortium sites. Such an established structure and process would serve as the foundation upon which to establish and maintain best training practices, and provide a culture for natural experimentation as to how the members can successfully develop and validate training approaches that enhance the CTSA Consortium’s function and effectiveness for conducting clinical trials.
Given the complexity of the consortium and diversity of regulatory training requirements across the 62 sites, an imperative was to determine what key regulatory principles might provide an optimal starting place in the effort to enhance and possibly standardize the training expectations of the clinical trial workforce. In determining this, the project leadership team recognized two foundational, mandatory training requirements implemented at every CTSA hub: institutionally based human subjects research training (uniquely provided by each hub) and Good Clinical Practice (GCP) training for industry-sponsored clinical trials. GCP is the accepted, international ethical, and scientific quality standard for the design, comprehensive conduct, and reporting of clinical trials. It also serves to protect the rights, integrity, and confidentiality of clinical trial subjects. Although it was recognized that industry sponsors of trials had a standard requirement for all study personnel engaged in their clinical trial to be trained in GCP, there was no such expectation for either federally sponsored, or other funded, investigator-initiated clinical trials. Therefore, the project aimed to address this gap in Phase I of this National Center for Advancing Translational Science (NCATS)-sponsored Enhancing Clinical Research Professionals’ Training and Qualifications (ECRPTQ) Project. In addition to establishing a foundation of GCP training expectations for all clinical trials work, the project also aimed to substantially reduce the administrative burden of this expectation created by multiple sponsors requesting completion of their independent GCP training programs before initiating a trial. TransCelerate BioPharma, a nonprofit collaboration established in 2012 comprised of now more than 20 leading biopharmaceutical companies, had already initiated an agreement by which any TransCelerate member’s GCP training completion would be reciprocally recognized by all sponsor members. Similarly, although not laying out precise content, other global sites such as the United Kingdom and India have mandated GCP certification for clinical researchers. The project leadership team embraced the notion that NCATS, and ultimately all other partner National Institutes of Health (NIH) institutes and centers, should accept no lower expectation for GCP training of study personnel conducting federally sponsored clinical trials. To that end, we embarked on a process to establish a consensus expectation across the CTSA Consortium that personnel involved in NIH-funded clinical trial activity be trained in GCP.
Materials and Methods
To achieve the goal of establishing standard expectations for GCP training across the CTSA Consortium, NCATS provided supplemental grant funding to support a consortium-wide project entitled “Enhancing Clinical Research Professionals’ Training and Qualifications” (3UL1TR000433-08S1; and individual hub supplement awards). The explicit goal of the project was to strengthen the quality and impact of the science of the clinical trial portfolio across the CTSA Consortium by enhancing the training and consequent qualifications of all study personnel. The first phase of this project was to develop consortium-wide consensus on recommendations for GCP training for clinical research professionals actively engaged in a clinical trial at every CTSA hub. Of note, the aim of a second phase was to identify the minimal competencies necessary for investigators and study coordinators to possess in order to design and execute safe, high quality, and efficient clinical trials and to identify existing training resources that propose to teach and assess those competencies. A paper describing the second phase is published in this journal by Calvin-Naylor and colleagues [Reference Calvin-Naylor3].
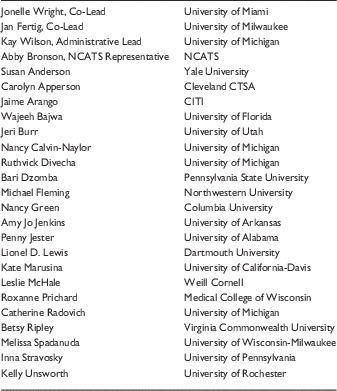
Dr Shanley and Dr Barohn served as Co-Principal Investigators for the project and led a team comprised of faculty and staff from CTSA hub sites at the University of Michigan, University of Kansas, University of Rochester, University of Miami, Boston University and Tufts University (Table 1). To complete the goal of the project’s first phase, a face-to-face meeting of representatives from every CTSA Consortium hub, along with several external stakeholders engaged in GCP training expectations and/or delivery, was held in Chicago, IL. The Northwestern University Clinical and Translational Sciences Institute hosted the meeting on their medical school facilities on November 3–4, 2014. The 2-day meeting provided an opportunity to take initial steps toward a transformative effort to optimize the ability of clinical researchers across the CTSA Consortium to conduct safe, efficient, and high-quality clinical trials. One hundred twenty participants attended the meeting with teleconference access provided to all CTSA hubs. Attendees also represented the pharmaceutical industry, the Clinical Trial Transformation Initiative, and the US Food and Drug Administration (FDA); as well as stakeholder organizations involved in GCP training platforms including the Association of Clinical Research Professionals, the Collaborative Institutional Training Initiative, and Western Institutional Review Board-Copernicus.
Table 1 Project Leadership Team
NCATS, National Center for Advancing Translational Science.
Results
As a first step, project participants agreed in principle that all personnel engaged in the execution of a clinical trial according to the NIH definition should understand the fundamentals of GCP (as listed in Appendix). The subsequent discussions focused on addressing four important questions necessary to this training implementation: Who should receive GCP training? What training should they receive? How should they receive the training? At what interval should retraining occur?
To frame these discussions, Margaret Koziel (University of Massachusetts) reviewed the principles of GCP and differentiated GCP training from other human subject research training that is typically covered by institution-specific human subjects research modules. Dr Koziel emphasized that GCP standards and training were developed to protect the rights and safety of study participants and optimize the quality of study results. She also highlighted that GCP is an international ethical and scientific quality standard for designing, conducting, recording, and reporting trials involving human subjects. Compliance with this standard provides public assurance that the rights, safety, and well-being of trial subjects are protected, consistent with the principles that have their origin in the Declaration of Helsinki. The standards set forth also aim to ensure that clinical trial data are credible. In order to provide such training, a number of organizations have developed approaches for training clinical trial workforces.
To provide examples of GCP training, several stakeholder organization representatives shared their approaches with attendees. Pamela Tenaerts from Clinical Trial Transformation Initiative reviewed their program’s comprehensive assessment of current practices in GCP training and potential strategies for reducing the burden of redundant GCP training (see http://www.ctti-clinicaltrials.org/what-we-do/study-start/gcp-training). It was emphasized that each clinical trial sponsor has historically required all study team personnel to complete sponsor-specific GCP training. This fragmented approach results in wide-ranging inefficiencies and counters efforts to standardize the approach for GCP training and significantly increases the burden of multiple redundant training requirements. Sheri Jacobsen, Associate Director of Global Clinical Training, Compliance and Initiatives for AbbVie (an industry member of TransCelerate), provided GCP training expectations from an industry-sponsored perspective and emphasized how reciprocal GCP training acceptance across TransCelerate members aimed to reduce redundant training requests.
At the conclusion of these presentations, participants constructed a consensus approach that would enable every CTSA program to fulfill an agreed-upon requirement for minimal, baseline GCP training across the consortium. To do so required addressing the questions posed above: Who should receive GCP training? What training should they receive? How should they receive the training? At what interval should retraining occur? Importantly, in an effort to ascertain the value to the proposed training approach, participants discussed what metrics should be tracked and reported to NCATS. In making the recommendations for attaining these project goals, participants attempted to strike a balance between ideals and practicalities which is reflected in the final recommendations.
Discussion
The following are recommended expectations for GCP training at all CTSA hubs.
Who Should Receive GCP Training?
It was unanimously agreed that GCP training should be required of all study personnel engaged in a drug, device, biologic, and/or behavioral intervention study that meets the new NIH definitionFootnote 1 of a clinical trial:
A research study [4] in which one or more human subjects [5] are prospectively assigned* to one or more interventions** (which may include placebo or other control) to evaluate the effects of those interventions on health-related biomedical or behavioral outcomes.***
(http://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-015.html)
*The term “prospectively assigned” refers to a pre-defined process (eg, randomization) specified in an approved protocol that stipulates the assignment of research subjects (individually or in clusters) to one or more arms (eg, intervention, placebo, or other control) of a clinical trial. See more at: http://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-015.html#sthash.pi2imZds.dpuf
**An intervention is defined as a manipulation of the subject or subject’s environment for the purpose of modifying one or more health-related biomedical or behavioral processes and/or endpoints. Examples include: drugs/small molecules/compounds; biologics; devices; procedures (eg, surgical techniques); delivery systems (eg, telemedicine, face-to-face interviews); strategies to change health-related behavior (eg, diet, cognitive therapy, exercise, development of new habits); treatment strategies; prevention strategies; and, diagnostic strategies. See more at: http://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-015.html#sthash.pi2imZds.dpuf
***Health-related biomedical or behavioral outcome is defined as the pre-specified goal(s) or condition(s) that reflect the effect of one or more interventions on human subjects’ biomedical or behavioral status or quality of life. Examples include: positive or negative changes to physiological or biological parameters (eg, improvement of lung capacity, gene expression); positive or negative changes to psychological or neurodevelopmental parameters (eg, mood management intervention for smokers; reading comprehension and/or information retention); positive or negative changes to disease processes; positive or negative changes to health-related behaviors; and, positive or negative changes to quality of life. See more at: http://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-015.html#sthash.pi2imZds.dpuf
At the meeting, although there was acknowledgment that much of GCP training principles apply to any clinical research activity, there was strong consensus that this training expectation should initially be limited to personnel engaged in execution of a clinical trial. Although there was agreement to use the NIH definition of a clinical trial, there was a lack of clarity with regards to the terms “engaged in.” A proposed working definition of “engaged in” for the purposes of this requirement was any clinical research professional involved in the design, conduct, performance, monitoring, auditing, recording, analysis, or reporting of a clinical trial. In terms of identifying who specifically should be expected to undergo GCP training, there was strong consensus that all research personnel formally listed as members of the study team (perhaps on the basis of the Institutional Review Board [IRB] application) should receive GCP training. The strongest argument in support of this broad inclusion was the emphasis on fostering team science whereby all members of a clinical trial team share common language and foundational training in the principles of GCP. However, given the perceived burden of execution, ultimately, representatives from all 62 hubs agreed to limit the expectation to investigators (principal and co-principal) and study coordinators at this initial stage. The inclusion of behavioral interventions implied in the NIH definition created a unique challenge. Although there is some content emphasized in current GCP training platforms that is relevant to behavioral trialists, some of the content is irrelevant as it pertains to specific regulatory processes for drug or device development. There was strong consensus that clinical trial teams testing a behavioral intervention should be familiar with the GCP principles, but that currently identified training modules lacked relevance in this domain. Therefore, the project leadership composed a separate task force charged with the directive of working with partner stakeholders to develop GCP training designed specifically for behavioral scientists and study team members involved in clinical trials. The work of this task force is described in a paper by Murphy and colleagues in this journal.
Another implication of this recommendation is that CTSA hubs must work within their institutional systems to determine strategies for tracking all clinical trials that meet the NIH definition (regardless of the use of or connection to CTSA resources). Furthermore, CTSA institutions must be able to ensure that all investigators and study coordinators on any given clinical trial have met the GCP training expectation. From a practical standpoint, most meeting participants who were regulatory research administrators and IRB members, believed that utilizing institutional regulatory bodies, such as the IRB, would most accurately facilitate this process, as all clinical trials must secure IRB approval. Discussants did identify an increasingly common circumstance that complicates this proposed approach: situations where an investigator cedes IRB reliance for a clinical trial to a central IRB and is not required to provide the names of study team members with his/her own institution. In these situations, it would become incumbent on that central IRB to identify these study team members and determine if they have had/or need GCP training. As the most common practice remains reporting study team members internally, the project leadership felt it was important to track these issues in order to identify exemplar solutions that address this unique complexity and to share best practice solutions across the CTSA Consortium. The project leadership wanted to ensure that the recommendations from the ECRPTQ Project do not adversely impact the use of central IRB mechanisms to facilitate/speed reviews.
What Training Should They Receive?
After identifying who would be required to have GCP training, the next step was to identify what the minimum requirements should be and how best to meet the training goal. To provide attendees with a variety of potential approaches, a series of presentations describing currently available teaching platforms were given. Representatives from the Association of Clinical Research Professionals (ACRP), the Collaborative Institutional Training Initiative (CITI), Western Institutional Review Board (WIRB), QD-Quality and Training Solutions Inc., Northwestern University, University of Cincinnati, and the University of Southern California all provided overviews of their existing approaches. The consensus achieved following these presentations was that there is a baseline level of GCP content that should be taught by the methodology selected by a CTSA site, but that there should continue to be hub-based flexibility to select a specific GCP training platform, provided it met minimal requirements. Admittedly, there was important recognition that simply understanding GCP principles, while an important first step, is insufficient for creating a more comprehensive, competency-based training approach for research professionals engaged in clinical trials. However, there was acknowledgment that this was the goal of Phase II of the project, the results of which are discussed in a paper by Calvin-Naylor and colleagues in this journal [Reference Calvin-Naylor3].
How Should They Receive the Training?
Although acknowledging that there should continue to be hub-based flexibility in selecting a specific GCP training platform, there was agreement that each approved platform must meet certain minimal requirements. Though there was debate as to the “optimal” standard, there was consensus that any platform should fulfill the agreed upon minimum criteria for International Conference on Harmonisation (ICH) training in GCP including:
-
(1) GCP overview
-
(2) Principles of ICH GCP
-
(3) Investigator and/or study coordinator responsibilities.
The project leadership agreed that approval should be given to any GCP training approach that incorporated an overview of GCP and the 13 ICH GCP principles outlined in the 1996 document: Harmonized Tripartite Guideline for Good Clinical Practice E6(R1): http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf (Appendix).1 It was also emphasized that any approved platform which included these fundamental components, should consequently be accepted as “common currency” by federal, foundation, and industry sponsors so as to eliminate redundant training requests. From the perspective of FDA expectations, it was recognized that GCP training was necessary but not sufficient to meet FDA expectations of full training and competencies of investigators and study coordinators involved with any clinical trial team.
The project leadership noted that there was insufficient knowledge about comparative effectiveness of various GCP training platforms to strongly recommend any single platform. At the face-to-face meeting it was also clear that there was no consensus support for adopting any single training tool or platform by all CTSA Consortium members. These observations led us to recommend maintaining flexibility for each hub’s GCP training selection. It was recognized, though beyond the scope of the current project, that this flexibility should allow comparative studies of the efficacy and impact of various options selected. As was demonstrated by the various presenters, GCP training approaches ranged from 45 to 60 minutes online module completion to multiple session-based training over a period of 12–24 hours. In the context of the meeting and brief presentations of content, it was unclear how much of the latter training approaches delved into training of competencies predicated on GCP principles (the explicit goal of Phase II of the project), or remained focused on imparting those minimal requirements of GCP training.
The project leadership agreed with the suggestion that a “peer-review” process be implemented to critically review the platforms chosen by each hub to ensure these requirements are met by the selected training platform(s). Furthermore, the approach chosen by each hub must comply with reporting of the defined outcome metrics that will be identified. Therefore, regardless of the structure, CTSA hubs will be expected to avail local information technology specialists to link training completion and tracking between the partner/platform generating the reports and their own hub in a manner that allows them to provide this report to NCATS in whatever manner each institute defines.
At What Interval Should Retraining Occur?
There was consensus that investigators and study coordinators should complete refresher training every 3 years. It was also acknowledged that there was little data supporting this recommendation, however, it is in line with industry expectations. Based upon the discussion at the meeting, the project leadership believes that CTSA Consortium members have an opportunity to develop survey and knowledge retention assessments that can more precisely ascertain the retention time of research professionals completing the various GCP training methodologies. This opportunity should strongly be encouraged by NCATS.
What Metrics Should be Tracked?
In order to ascertain the impact of a GCP training expectation on the clinical trial enterprise workforce across the CTSA Consortium hubs, a GCP training Metrics Work Group (Table 2) was formed.
Table 2 Good Clinical Practice Training Metrics Work Group
NCATS, National Center for Advancing Translational Science; CTSA, Clinical and Translational Science Award; CITI, Collaborative Institutional Training Initiative.
The Work Group was charged with developing metrics to evaluate the process and the impact of implementing the GCP training expectation across CTSA hubs. Twenty-four volunteers from the cohort of expert CTSA representatives who attended the first national meeting of the ECRPTQ Project comprised work group. The Work Group’s action plan involved:
-
(1) Defining characteristics of outcome measure and evaluation metrics: The metrics were informed by NCATS’ suggestions on what could be tracked and in considering the possible metrics proposed in the original ECRPTQ Project application to NCATS as well as in the context of how NIH handles similar training-related tracking and reporting responsibilities (ie, NIH-mandated human subjects protections training requirements). In doing so, the Work Group determined that outcome metrics identified must be:
-
(a) Simple to understand and easy to obtain from all sites.
-
(b) Consistent with FDA expectations.
-
(c) Confined to data that CTSA managers and NIH would be likely to use.
-
(d) Broad enough to apply to different types of GCP training (agnostic regarding the particular training platform selected).
-
(e) Multi-method in approach: qualitative (eg, local Principal Investigators evaluating implementation of the program) and quantitative (eg, evaluating program adherence, process, and success).
-
(f) Geared toward the needs of relevant audiences (ie, CTSA PIs, hub institutions, CTSA Consortium/Steering Committee, NCATS).
During its deliberations, the Work Group remained cognizant that the roll-out of the GCP training expectation would take place in a time frame following completion of the ECRPTQ Project. Thus, NCATS/NIH will communicate the expected data collection and analysis of program outcome metrics based upon these recommendations.
-
-
(2) Constructing the assessment model: To begin constructing the model, the Work Group supplemented principles of program evaluation with input from experts in adult education, web-based training, and IT platform user friendliness and used a reiterative process of priority mapping. The Work Group ultimately decided to characterize and evaluate the roll-out/implementation of this CTSA-wide GCP training expectation in 4 areas:
-
(a) Program Success: Measured by numbers of individuals completing the training and CTSA hub adherence-to-expectation rates.
-
(b) Program Impact: Reduction in redundant training.
-
(c) Program Process: Training platform used at each CTSA hub; institutional office managing the required tracking and reporting procedures for each hub.
-
(d) Comparative Effectiveness: Learner and PI satisfaction.
-
-
(3) Defining outcome metrics: In identifying multiple potential short and long-term outcome measures and training evaluation metrics, the Work Group ultimately narrowed its focus to two levels of assessment: the learner and the institution. Feasibility with respect to the cost and effort involved in conducting program evaluation across the entire CTSA Consortium was a main consideration. There was clear consensus among members of the Work Group that:
-
(a) Measures of program success and program impact were absolutely essential for program evaluation.
-
(b) Recommended assessments of program process (ie, program implementation) and comparative effectiveness were excellent, albeit optional, measures. These optional measures, however, would provide institutional authorities, program officers, and the CTSA Steering Committee valuable program implementation information.
-
Work Group Recommendation
At their conclusion, the Work Group recommended specific measures to evaluate and characterize the CTSA-wide implementation of the GCP training expectation at each hub. Table 3 outlines the Work Group recommendations. The evaluation consists of two essential and two optimal metrics. It is essential to measure the program’s impact and success. The Work Group suggested that CTSA hubs would submit data for these measures as part of their Research Performance Progress Report to NCATS. Optional data measures may provide helpful insights regarding the implementation and comparative effectiveness of the GCP training expectation.
Table 3 Work Group Recommendations to Evaluate Implementation of Good Clinical Practice (GCP) Training Expectations Across the Clinical and Translational Science Award (CTSA) Consortium

Conclusion
This report summarizes recommendations for foundational mandatory training for research personnel involved in conduct of clinical trials across the CTSA Consortium. The goal of this project is to ensure all study personnel are equipped with the necessary and fundamental competencies to execute clinical trials. Additional phases of this project, such as GCP training targeted at personnel involved in behavioral trials, are reported in separate papers in this journal. The efforts undertaken in this project were designed to strengthen the translational science workforce and ultimately advance translation of discoveries.
Declaration of Interest
None.
Acknowledgments
The authors thank Christopher P. Austin (MD), Petra Kaufmann (MD, MSc), Todd Wilson, DO, and Michelle A. Culp, MPH for their support and insightful comments with this supplement. The authors thank all of the work of the Michigan Institute for Clinical and Health Research at the University of Michigan, especially Vic Divecha, for all of his project management expertise and organizational skills, Christina Loar, Brenda Eakin, and Vicki Ellingrod for all of their assistance with this project. This paper was supported by an administrative supplement award to Michigan Institute for Clinical and Health Research at the University of Michigan (3UL1TR000433-08S1; and individual hub supplement awards to all 62 CTSAs). The leadership team consisted of representatives from the following CTSAs: Heartland Institute Clinical and Translational Research (UL1TR000001), Miami Clinical and Translational Science Institute (1UL1TR000460), Tufts Clinical and Translational Science Institute (UL1TR001064), and the University of Rochester Clinical and Translational Science Institute (UL1TR000042).
Appendix
The agreed upon minimum criteria for ICH training in GCP should include the following:
-
(I) GCP overview
-
(II) Principles of ICH GCP
-
(III) Consequent investigator and/or study coordinator responsibilities.
GCP training must include an overview of GCP and the 13 ICH GCP principles outlined in the 1996 document: Harmonized Tripartite Guideline for Good Clinical Practice E6(R1) (see footnote1):
-
(1) Clinical trials should be conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki, and that are consistent with GCP and the applicable regulatory requirements.
-
(2) Before a trial is initiated, foreseeable risks and inconveniences should be weighed against the anticipated benefit for the individual trial subject and society. A trial should be initiated and continued only if the anticipated benefits justify the risks.
-
(3) The rights, safety, and well-being of the trial subjects are the most important considerations and should prevail over interests of science and society.
-
(4) The available nonclinical and clinical information on an investigational product (IP) should be adequate to support the proposed clinical trial.
-
(5) Clinical trials should be scientifically sound, and described in a clear, detailed protocol.
-
(6) A trial should be conducted in compliance with the protocol that has received prior IRB/independent ethics committee (IEC) approval/favorable opinion.
-
(7) The medical care given to, and medical decisions made on behalf of, subjects should always be the responsibility of a qualified physician or, when appropriate, of a qualified dentist.
-
(8) Each individual involved in conducting a trial should be qualified by education, training, and experience to perform his or her respective tasks.
-
(9) Freely given informed consent should be obtained from every subject before clinical trial participation.
-
(10) All clinical trial information should be recorded, handled, and stored in a way that allows its accurate reporting, interpretation, and verification.
-
(11) The confidentiality of records that could identify subjects should be protected, respecting the privacy and confidentiality rules in accordance with the applicable regulatory requirements.
-
(12) IPs should be manufactured, handled, and stored in accordance with applicable good manufacturing practice. They should be used in accordance with the approved protocol.
-
(13) Systems with procedures that assure the quality of every aspect of the trial should be implemented.
In addition, the training should emphasize the following investigator responsibilities:
-
(1) Investigator qualifications and agreements
-
∙ Investigator qualification (education, training, experience).
-
∙ Demonstrate evidence of adequate training (provide up-to-date CV).
-
∙ Awareness of and compliance with GCP and regulatory requirements.
-
∙ IP familiarity.
-
∙ Allow for monitoring/auditing/inspection to enable sponsor/regulatory oversight.
-
∙ Introduce definitions of monitoring (1.38), audit (1.6), and inspection (1.29).
-
∙ Use of qualified support staff.
-
∙ Document delegation of duties to appropriately qualified persons.
-
-
(2) Adequate resources
-
∙ Potential to recruit suitable subjects.
-
∙ Sufficient time to conduct trial.
-
∙ Sufficient qualified staff and adequate facilities to conduct trial.
-
∙ Staff are adequately informed about protocol, IP, and tasks related to the protocol.
-
-
(3) Medical care of trial subjects
-
∙ Qualified physician or dentist who is an investigator or sub-investigator should be responsible for all trial-related medical decisions.
-
∙ During and following the trial, the investigator/institution should ensure appropriate medical care for adverse events (AEs) and clinically significant lab deviations related to trial and inform subjects if medical care is needed for intercurrent illness.
-
∙ Inform primary (family) physician of subject’s participation in trial (after obtaining permission from the subject).
-
∙ Physician to make a reasonable effort to ascertain the reasons for subject’s premature withdrawal from the trial.
-
-
(4) Communication with IRB/IEC
-
∙ Definition of IRB (1.31) and IEC (1.27).
-
∙ Before trial begins, obtain written, dated approval/favorable opinion for protocol and all documents provided to subjects (eg, informed consent form [ICF], advertisements).
-
∙ Provide a copy of Investigator’s Brochure (IB)/updated IB.
-
∙ Before and during the trial, provide all documents required by IRB/IEC for review and appropriate approval/favorable opinion.
-
-
(5) Compliance with protocol
-
∙ Conduct trial according to approved protocol, GCP, and applicable regulatory requirements, for example, sufficient documentation to support subject meeting inclusion/exclusion criteria.
-
∙ Document the acceptance to follow protocol in a protocol signature page or contract.
-
∙ Protocol deviation process: no deviations or changes before sponsor and IRB/IEC approval. Exception: deviation necessary to eliminate immediate hazard to trial subject. Deviations need to be documented and rationale submitted to sponsor, IRB/IEC, and regulatory authorities.
-
-
(6) IPs
-
∙ Responsibility for IP (refer to 1.33) accountability and delegation of activities and supervision of an appropriately qualified person.
-
∙ Documentation of delivery, inventory, dispensation, usage, disposal or return, and reconciliation of all IP and other study medication.
-
∙ Stored per requirements.
-
∙ IP usage per protocol.
-
∙ Explanation of correct use of IP to subjects and periodic check for understanding/compliance.
-
-
(7) Randomization procedures and unblinding
-
∙ Follow the trial’s randomization procedures.
-
∙ Blinded trials: promptly document and report to sponsor any premature unblinding.
-
-
(8) Informed consent of trial subjects
-
∙ Definition of informed consent.
-
∙ Explain the informed consent process and informed consent form (ICF):
-
– IRB/IEC written approval in advance of use for written consent and other written information to be provided to subjects.
-
– Subject to be fully informed of all pertinent aspects of the trial before participation.
-
– The informed consent discussion and form needs to include all relevant explanations. Refer or link to ICH 4.8.10.
-
– Language used in oral and written information (ICF) should be understandable to subject or legal representative and impartial witness (where applicable).
-
– Subject should have ample time to review the ICF and to ask any questions and receive answers before decision is made.
-
– Subject should not be unduly influenced to participate.
-
– ICF should be obtained/signed before a subject’s participation in a trial (before any study procedures are performed).
-
– Subject should be aware that withdrawal is possible at any time.
-
– Subject should not be asked to waive legal rights or release investigator or sponsor from liability for negligence.
-
– Written ICF must be updated/approved when new information is available that may be relevant to subject’s consent.
-
-
-
∙ Informed consent documentation: the ICF should be signed and personally dated by the subject and/or the legal representative and by the person who conducted the consent.
-
∙ Informed consent of special population:
-
∙ Refer to or add definition of Vulnerable Subjects: when a subject (eg, minor, incapacitated) can only be enrolled with the consent of the legal representative, the subject must be informed to the level of their understanding, provide assent (where this is feasible), and personally sign and date the consent form.
-
– In emergency situations where the subject and legal representative are unable to consent, enrollment requires protective measures to be described in protocol or other IRB/IEC-approved documents. Subject or legal representative should be informed as soon as possible and consent to continue and other consent as appropriate.
-
– If the subject/legal representative is unable to read, an impartial witness must be present during the consent discussion and sign and date the consent form.
-
– A signed and dated copy of the ICF should be given to the subject or the legal representative (including any other written information provided to the subject).
-
– The informed consent process should be documented in the medical record/source file (as well as documentation regarding communication of new information).
-
-
-
-
(9) Records and reports
-
∙ Definition of source documents: the actual documents (originals) GCP glossary (brief).
-
∙ Refer to or add definition of source data.
-
∙ Definition of essential documents.
-
∙ The need to maintain and retain essential documents.
-
∙ CRFs and all required reports (written or electronic).
-
– Accuracy, legibility, completeness of data.
-
– Data to be consistent with source data.
-
-
∙ Corrections are dated and initialed, do not obscure original entry and explained if necessary (applies to written and electronic changes/updates). Retain records of changes and corrections.
-
∙ Financial aspects documented in an agreement between sponsor and investigator/institution
-
∙ Direct access to all trial-related documents by the monitor, the auditor, the IRB/IEC, or regulatory authority.
-
-
(10) Progress reporting/final reports
-
∙ Investigator submits written summaries of progress to IRB/IEC at least annually or as required.
-
∙ Provide written reports to sponsor and IRB/IEC (and institution where required) of any significant changes affecting the study or increased risk to subjects.
-
∙ Upon completion of trial, provide sponsor with all required reports.
-
∙ Final report with a summary of trials and outcomes submitted to IRB/IEC and regulatory authorities as required.
-
-
(11) Safety reporting
-
∙ AE definition.
-
∙ Refer to or add definition of ADR (1.1) and unexpected ADR (1.60).
-
∙ AE reporting: all AEs and/or laboratory abnormalities should be reported to the sponsor within the time period defined in protocol.
-
-
∙ Definition of a serious adverse event (SAE).
-
∙ All SAEs should be reported immediately to the sponsor except for those SAEs that the protocol or other document (eg, Investigator’s Brochure) identifies as not needing immediate reporting.
-
– Prompt follow-up by detailed written reports.
-
– Subjects should be identified by unique code numbers.
-
– Report unexpected serious drug reactions according to regulatory and IRB/IEC requirements.
-
– Sponsor and IRB/IEC may need additional information for reported deaths (eg, autopsy report).
-
-
-
(12) Premature termination or suspension of trial
-
∙ Responsibility to promptly inform the trial subjects and ensure appropriate therapy and follow-up. Inform regulatory authorities when required.
-
∙ Responsibility for communication of study termination or suspension of study to sponsor, IRB/IEC, and institution as applicable, including a detailed written explanation.
-
Finally, in the event an investigator is also serving as Sponsor of the clinical trial, additional responsibilities are expected as outlined in Section 5 (pages 20–30) of the Harmonized Tripartite Guideline for Good Clinical Practice E6(R1) (see footnote1).





