Introduction
Malaria, a vector-borne disease, is a serious public health concern and continues to be a major focus of the Sustainable Development Goals (Dawaki et al., Reference Dawaki, Al-Mekhlafi, Ithoi, Ibrahim, Atroosh and Abdulsalam2016; Okunlola & Oyeyemi, Reference Okunlola and Oyeyemi2019). In 2019, about 229 million cases and 409,000 malaria-associated deaths occurred worldwide, with nearly half of the world’s population being at risk (World Health Organization, 2020). Although about 97 countries and territories in the tropics and sub-tropics are burdened by malaria, fifteen contributed the highest burden with 80% of malaria-associated deaths (Okunlola & Oyeyemi, Reference Okunlola and Oyeyemi2019). Regionally, sub-Saharan Africa (SSA) is accountable for about 92–94% of the global malaria burden (Okunlola & Oyeyemi, Reference Okunlola and Oyeyemi2019; World Health Organization, 2020).
Since 2010, there has been a global reduction in the rate of decrease in malaria incidence. The decrease generally halted in 2014, and reversed in some countries (World Health Organization, 2018). In Nigeria, about 100% of the population is at risk of malaria, and the country contributed the highest proportion of malaria cases (25%) and malaria deaths (24%) globally in 2018 (World Health Organization, 2019b). It was also one of two countries with the highest rates of malaria infection in pregnancy (World Health Organization, 2019b). Nationally, malaria contributes about 60% of all outpatient visits to health facilities and 30% of child mortality (Dawaki et al., Reference Dawaki, Al-Mekhlafi, Ithoi, Ibrahim, Atroosh and Abdulsalam2016; Andrada et al., Reference Andrada, Herrera, Inyang, Mohammed, Uhomoibhi and Yé2019).
In 2019, an estimated US$3 billion was spent on malaria control and elimination globally, with governments of endemic countries contributing about US$900 million (31%) (World Health Organization, 2020). Malaria has been shown to intensify poverty, limit educational opportunities and increase absenteeism in schools and at work in affected populations (Van Damme-Ostapowicz et al., Reference Van Damme-Ostapowicz, Krajewska-Kułak, Rozwadowska, Nahorski and Olszański2012; Ghahremani et al., Reference Ghahremani, Faryabi and Kaveh2014). However, despite a scaling up of efforts, global malaria reduction and long-term elimination programmes have not seen much success due to lack of resources, economic constraints, long distance to health facilities, limited knowledge of malaria, parasitic drug resistance and insecticide-resistant mosquitoes (Pell et al., Reference Pell, Straus, Andrew, Meñaca and Pool2011; Ghahremani et al., Reference Ghahremani, Faryabi and Kaveh2014; Diiro et al., Reference Diiro, Affognon, Muriithi, Wanja, Mbogo and Mutero2016).
Very importantly, the World Health Organization (WHO) devised the Global Technical Strategy for Malaria 2016–2030, which called for the elimination of malaria in at least ten countries that had the greatest burden of the disease in 2015 by the year 2020. In 2016, 21 countries spanning five regions were identified by the WHO as being able to defeat malaria by 2020, based on the likelihood of elimination across key criteria, and these countries formed the E-2020 initiative. Recently, WHO launched the E-2025 initiative, which aims to halt transmission of the disease in 25 more countries by 2025 (World Health Organization, 2019a, 2021). Measures such as controlling mosquito breeding sites and the use of long-lasting insecticide-treated nets (LLINs) play key roles in achieving these targets (World Health Organization, 2020). Sadly, only 40% of the at-risk population worldwide slept under LLINs in 2018 (World Health Organization, 2019b). The Nigerian Government, through the National Malaria Elimination Programme (NMEP) and collaborators, have instituted malaria prevention and treatment interventions towards achieving the 2014–2020 National Malaria Strategic Plan (NMSP) (Federal Ministry of Health, 2014). This strategic plan aimed to reduce the incidence rate of malaria to less than 5000 per 100,000 persons and reduce deaths attributable to malaria to zero by 2020. One of the objectives of this goal was to provide at least 80% of the targeted population with appropriate preventive measures by 2020, including increased LLIN ownership coverage (Federal Ministry of Health, 2014; Andrada et al., Reference Andrada, Herrera, Inyang, Mohammed, Uhomoibhi and Yé2019). A mixed-model approach, including free mass LLIN distribution campaigns (e.g. through immunization and antenatal care services) was devised by the NMEP (Andrada et al., Reference Andrada, Herrera, Inyang, Mohammed, Uhomoibhi and Yé2019). Nigeria’s NMEP resulted in LLIN use increasing from 8% in 2008 to 61% in 2018 (Ameyaw et al., Reference Ameyaw, Adde, Dare and Yaya2020).
In Nigeria, socio-demographic and economic factors play key roles in the uptake of malaria prevention and control measures. These vary by region, place of residence, education and other maternal demographic characteristics (Ameyaw et al., Reference Ameyaw, Adde, Dare and Yaya2020). Malaria is reported to mainly affect vulnerable communities (Gómez et al., Reference Gómez, Caicedo, Gaitán, Herrera-Varela, Arce, Vallejo, Padilla and Chaparro2017). Young children are biologically vulnerable to malaria. Also, less educated people and housewives living in precarious conditions are at high risk of malaria infection (Gómez et al., Reference Gómez, Caicedo, Gaitán, Herrera-Varela, Arce, Vallejo, Padilla and Chaparro2017). Contrasting studies have indicated that formal education is both a positive (Dike et al., Reference Dike, Onwujekwe, Ojukwu, Ikeme, Uzochukwu and Shu2006; Diiro et al., Reference Diiro, Affognon, Muriithi, Wanja, Mbogo and Mutero2016) and negative (Ahmed & Zerihun, Reference Ahmed and Zerihun2010; Auta, Reference Auta2012) predictor of uptake of malaria prevention and treatment strategies. The majority of malaria cases are thought to occur in rural areas worldwide, but with a growing number of urban and peri-urban cases (Padilla et al., Reference Padilla, Chaparro, Molina, Arevalo-Herrera and Herrera2015). Rapid rural–urban migration has resulted in populations living in poor socioeconomic conditions with inadequate housing infrastructure and a lack of public services. These settlements usually have inadequate sanitation and poor surface water drainage, leading to the development of water bodies and vegetation-rich areas, which act as breeding grounds for mosquitoes, especially Plasmodium falciparum and Plasmodium vivax (De Silva & Marshall, Reference De Silva and Marshall2012; Padilla et al., Reference Padilla, Chaparro, Molina, Arevalo-Herrera and Herrera2015). In Nigeria, the human malaria parasites include P. falciparum, P. ovale and P. malariae, among others. Plasmodium falciparum, transmitted through the bites of competent female mosquitoes of the genus Anopheles, is said to account for around 90–95% of malaria infections, while P. malariae and P. ovale are estimated to be responsible for less than 5% of infections (Oduola et al., Reference Oduola, Olojede, Oyewole, Otubanjo and Awolola2013; World Health Organization, 2018).
Oduola et al. (Reference Oduola, Olojede, Oyewole, Otubanjo and Awolola2013) assessed malaria vector abundance and diversity in rural and urban communities in three selected major towns in south-western Nigeria, to determine the impact of urbanization on the diversity and abundance of the Anopheles species associated with malaria transmission in human habitations. Ten Anopheles species were identified in the rural communities, with only four species, namely A. gambiae, A. funestus, A. moucheti and A. nili, occurring in more than 50% of the rural communities. On the other hand, eight Anopheles species were identified in the urban communities, with only one species (A. gambiae) occurring in all urban communities, while three major vectors (A. funestus, A. moucheti and A. nili) occurred in no more than 20% of the urban communities. Additionally, some mosquito species seem to easily adapt to new breeding conditions in urban settings (De Silva & Marshall, Reference De Silva and Marshall2012; Oduola et al., Reference Oduola, Olojede, Oyewole, Otubanjo and Awolola2013). Another study in Malawi reported that Anopheles abundance was greater during rainy seasons, with A. funestus being more abundant than A. arabiensis, although the female of both species significantly increased with distance from the urban centre (Dear et al., Reference Dear, Kadangwe, Mzilahowa, Bauleni, Mathanga and Duster2018).
These socio-demographic and economic factors and ‘social characteristics within which living takes place’ serve as structural mechanisms that affect a wide range of health conditions (World Health Organization, 2010; Committee on Educating Health Professionals to Address the Social Determinants of Health et al., 2016). These factors stratify populations into groups, which results in health inequalities, including in malaria transmission, and invariably shapes specific determinants of health status and reflects individuals’ experiences in exposure and vulnerability to health-compromising conditions (World Health Organization, 2010). Together with contextual factors and the socioeconomic position of individuals from such stratification, these underpin the Social Determinants of Health (SDH) framework (World Health Organization, 2010; Committee on Educating Health Professionals to Address the Social Determinants of Health et al., 2016). Although adherence to, and use of, malaria preventive measures depend on multiple factors such as accessibility of LLINs, the behaviour and perception of people about the risk of malaria severity and effectiveness of preventive measures play key roles. The WHO resolved to ‘continue to invest in changing people’s behaviour’ towards ending the malaria epidemic by 2030 (World Health Organization, 2018).
To date, studies have focused on malaria prevention and the use of LLINs in Nigeria, predominantly focusing on the ownership and use of LLINs (Adebayo et al., Reference Adebayo, Akinyemi and Cadmus2014; Adedokun & Uthman, Reference Adedokun and Uthman2020). However, there is paucity of information on the relationship between perceived severity of malaria and the use of LLINs. In some settings, uncomplicated malaria is becoming a ‘normalized illness’ and affects people’s perception of risk (Jones & Williams, Reference Jones and Williams2004; Giardina et al., Reference Giardina, Kasasa, Sié, Utzinger, Tanner and Vounatsou2014). With seasonality being a source of bias, different surveys conducted during dry and hot months (e.g. because of issues of accessibility of remote areas), when people are less likely to sleep under bed nets, may affect the accuracy of the research results that inform policy decisions (Giardina et al., Reference Giardina, Kasasa, Sié, Utzinger, Tanner and Vounatsou2014). Also, the occurrence of malaria is closely related to naturally existing environmental and climatic conditions and anthropogenic activities (Odongo-Aginya et al., Reference Odongo-Aginya, Ssegwanyi, Kategere and Vuzi2005). Although Nigeria’s current malaria control situation has improved, with the aid of both international and local initiatives, one of the roadblocks, however, to reduction and long-term elimination is the vector harbourage posed by clogged drainage systems (Farid, Reference Farid2016). Nigeria has predominantly two seasons. In the south, the rainy season lasts from March to November, whereas in the north it lasts only from mid-May to September (Britannica, 2021). The rest of the months are dry season. During the rainy seasons, waste accumulated in the dry seasons blocks drainage, making it hard for water to flow easily and causing stagnant water to collect, creating breeding sites for mosquitoes (Amoran et al., Reference Amoran, Onwumbe, Salami and Mautin2014).
Therefore, this study explored the rural–urban dimensions of the perception of malaria severity and practice of malaria preventive measures using the nationally representative 2018 Demographic and Health Survey dataset for Nigeria. The theoretical frameworks of the study were the Health Belief Model (HBM) and the Social Determinants of Health (SDH) framework, which were used to explain the results and how they inform policies towards reducing malaria incidence. The HBM is a psychological model that attempts to explain and predict health behaviours by focusing on the attitudes and beliefs of individuals (Green & Murphy, Reference Green and Murphy2014; Jones et al., Reference Jones, Jensen, Scherr, Brown, Christy and Weaver2015). It proposes six constructs to explain and predict preventive health behaviours: modifying factors, perceived threats (severity and susceptibility), benefits, barriers, self-efficacy and cues to action. It focuses on intra-personal factors, including risk-related beliefs that influence individuals’ health-related decision-making. The HBM can be used to interpret people’s perception of health threats and subsequent compliance with health interventions (Green & Murphy, Reference Green and Murphy2014; Watanabe et al., Reference Watanabe, Kaneko, Yamar, Leodoro, Taleo, Tanihata, Lum and Larson2014; Jones et al., Reference Jones, Jensen, Scherr, Brown, Christy and Weaver2015).
This study explored the association of women’s perceptions of the severity of malaria and the decision-making process in the uptake of preventive measures in Nigeria. The findings will inform policymakers when designing specific interventions to change the perception of the use of LLINs. The aim was to establish a baseline for effective and cost-effective initiatives for the Federal Government of Nigeria towards reducing malaria and its associated complications.
Methods
Data
The study used a female dataset from the 2018 Nigeria Demographic and Health Survey (NDHS). The 2018 NDHS data were cross-sectional and collected from 14th August to 29th December 2018. The survey adopted a two-stage sampling design (National Population Commission & ICF, 2019), details of which can be found in previous reports (National Population Commission & ICF, 2009; National Population Commission & ICF, 2013). A total of 42,121 women of reproductive age (15–49 years) were eligible to be interviewed and 99.288% of them responded to the questionnaire (National Population Commission & ICF, 2019). A total of 1128 (2.7% of 41,821) respondents who indicated that they did not know, or were not sure, that malaria led to death were excluded from the dataset during the data cleaning before analysis. The final analytic sample was 40,693 women.
Measures
Dependent variable
The dependent variable was ‘adoption of a malaria preventive measure’. The survey variable ‘type of mosquito bed net(s) slept under last night’ was used, with the responses ‘0’ for no net, ‘1’ for only a treated net, ‘2’ for both treated and untreated nets and ‘3’ for only an untreated net. Respondents who slept only under a treated net the night before the survey were treated as ‘having adopted a malaria preventive measure’ and all other respondents as otherwise.
Independent variable
The independent variable for the study was ‘perceived severity of malaria’. The survey variable used was whether respondents agreed or disagreed (or responded ‘do not know’) to the statement ‘every case of malaria can potentially lead to death’ (National Population Commission & ICF, 2019). The study hypothesized that respondents who agreed that malaria could potentially lead to death would adopt malaria preventive measures.
Control variables
Control variables were identified and selected from the dataset based on the literature and their availability in the female dataset and included respondent’s age, education level, marital status, whether they had a child under 5 years, employment status, religion, rural–urban place of residence, household wealth and region of residence.
Analysis
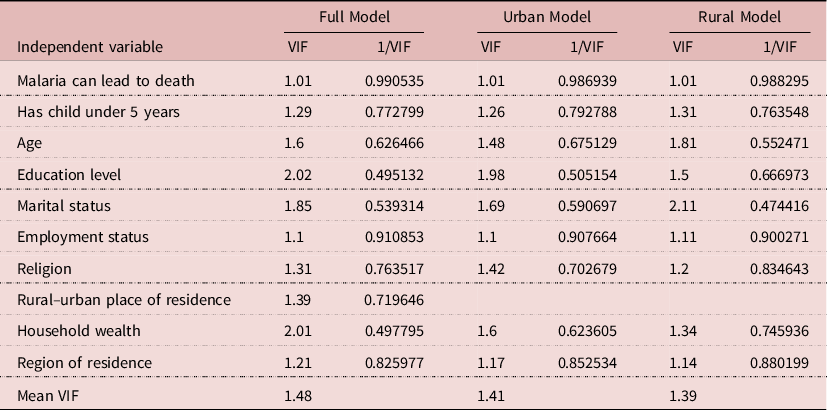
Analyses were conducted using STATA version 14. The variables were first cleaned and re-coded to create the final respondent sample of 40,693 women. Assumptions of multicollinearity were tested for, and no violations were observed; all independent variables in the models had variance inflation factors (VIFs) values of less than 3, which is far less than the cut-off value of 10 (see Table 1).
Table 1. Multicollinearity statistics of the variables in the study models
The svyset command was used to set the analytical environment to account for the two-stage sampling methodology (sampling weight, stratification and the primary sample units) of the NDHS. Frequency and percentages were used to describe the sample. Poisson regression was used to test the study hypothesis using bivariable and multivariable analyses. Poisson regression was used to estimate prevalence ratios because the proportion of the outcome of interest exceeded 12% (Barros & Hirakata, Reference Barros and Hirakata2003; Zou, Reference Zou2004; Santos et al., Reference Santos, Fiaccone, Oliveira, Cunha, Barreto and do Carmo2008; Zou & Donner, Reference Zou and Donner2013). In such situations, prevalence ratios should be reported instead of the frequently reported odds ratio; it has been proven that the use of odds ratios biased the coefficients showing strength and direction of statistical relationships and the confident intervals and standard errors (Barros & Hirakata, Reference Barros and Hirakata2003; Zou, Reference Zou2004; Santos et al., Reference Santos, Fiaccone, Oliveira, Cunha, Barreto and do Carmo2008; Zou & Donner, Reference Zou and Donner2013).
Results
Characteristics of respondents by their use of treated bed nets
Table 2 presents the demographic and socioeconomic characteristics of the respondents by whether they slept under an LLIN the night before the survey. About 48% of respondents slept under LLINs the night before the survey. About 34% disagreed that malaria could lead to death. About 49% of the women who agreed that malaria could lead to death slept under LLINs, compared with 45% of those who disagreed. Women in the 20–24 (51.39%) and 25–29 (51.22%) age categories had higher proportions of those sleeping under LLINs the previous night than women in other age groups. Surprisingly, more women with no formal education (63.08%) slept under LLINs the previous night compared with those with some formal education (less than 50%). Women living in rural areas were more likely to have slept under LLINs the previous night (56.18%) than their urban counterparts (37.42%). All the analysed socio-demographic variables were significantly associated with the outcome. Details of the remaining statistics are shown in Table 2.
Table 2. Distribution of characteristics of respondents by whether they reported sleeping under a long-lasting insecticide-treated net (LLIN) the night before the survey
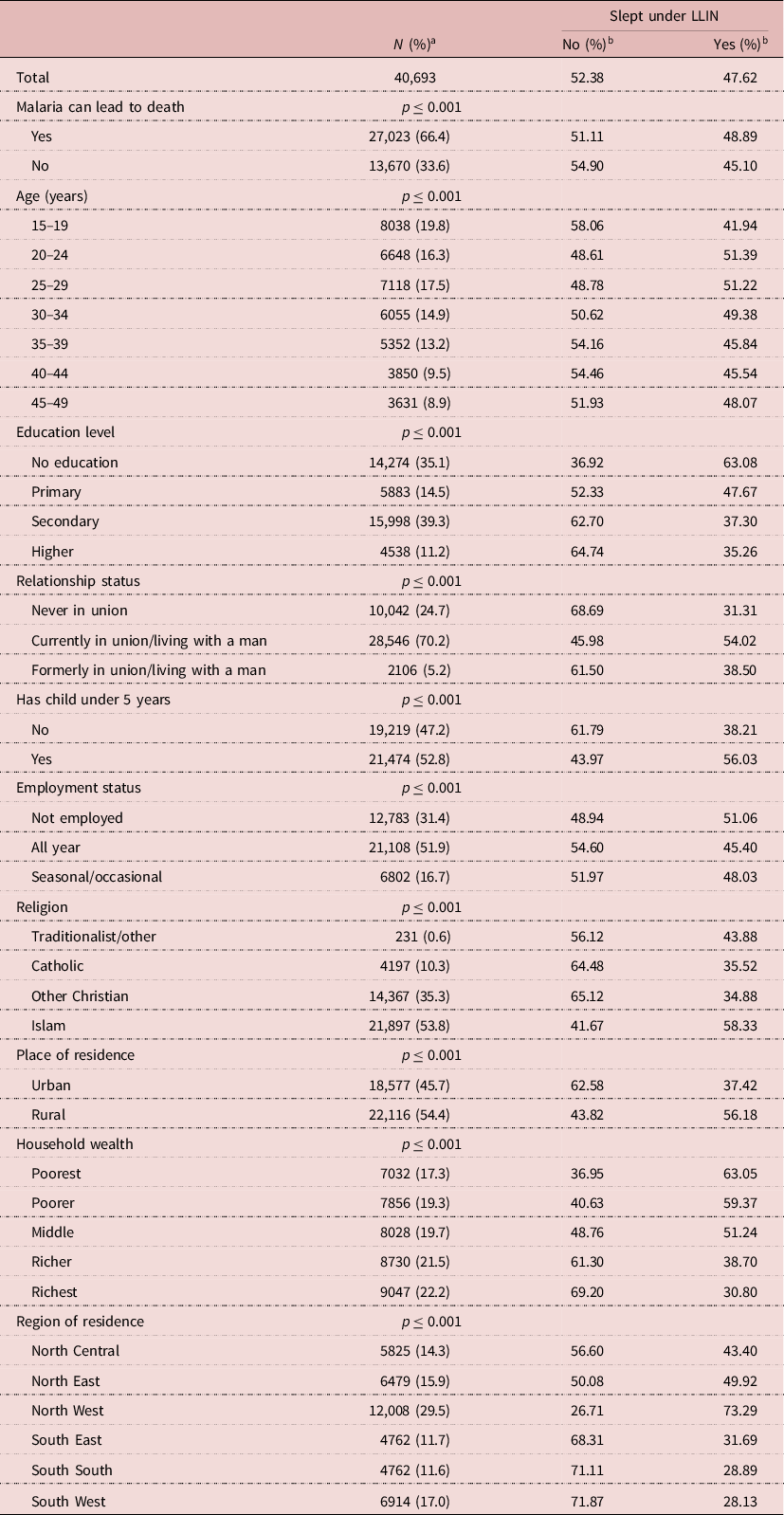
a Column percentage reported.
b Row percentage reported.
Regression analysis of perceived malaria severity by use of treated bed nets
Women who perceived that malaria could lead to death had a higher likelihood of sleeping under LLINs the previous night in the urban, rural and combined samples (Table 3). After adjusting for other socio-demographic variables, the association between perceived malaria severity and use of LLINs was only significant for rural women (APR=0.964, 95% CI: 0.933, 0.996) (Table 3). The results unexpectedly suggest that, holding the effect of all other variables in the model constant, rural Nigerian women who perceived malaria to be severe (and could lead to death) had a lower likelihood of adopting a malaria-preventive measure compared with those who did not perceive malaria to be severe (Table 3).
Table 3. Perceived malaria severity regressed on the use of long-lasting insecticide-treated nets and controlled for socio-demographic variables
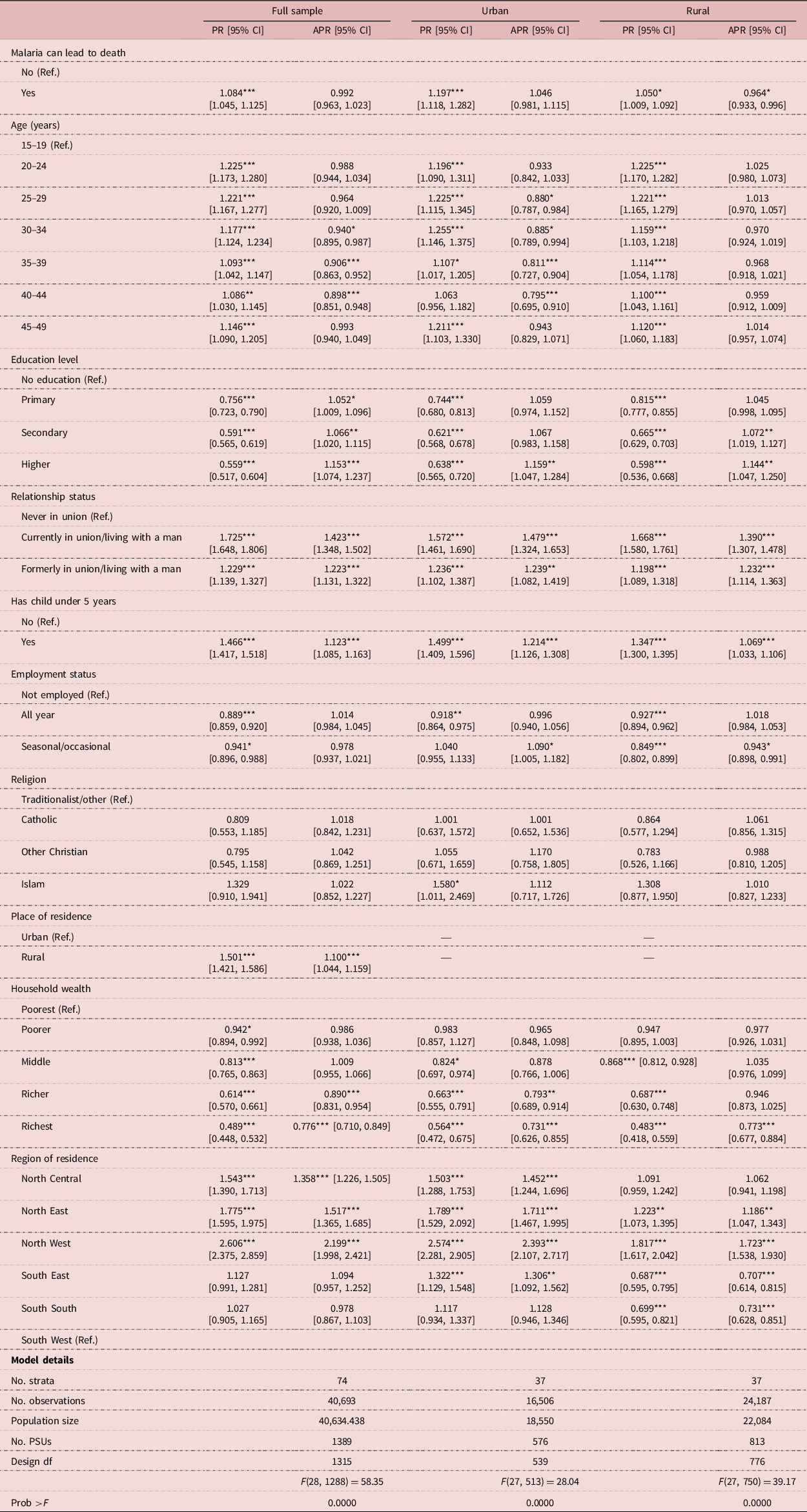
Exponentiated coefficients; 95% confidence intervals in brackets.
*p<0.05; **p<0.01; ***p<0.001.
Rural–urban variations were observed in the relationship between socio-demographic variables and the use of LLINs. Women’s age was significantly associated with sleeping under an LLIN in urban areas but not in rural areas. In the urban sample, compared with 15- to 19-year-old women, women who belonged to an older age group (except 20–24 years and 45–49 years) were significantly less likely to sleep under an LLIN (Table 3). Although formal education was a significant factor in both urban and rural models, some differences existed in their contribution to the model. In the rural model, women who attained a secondary level education or higher were more likely to use an LLIN. In the urban model, however, only the attainment of a post-secondary education status was positively associated with sleeping under an LLIN (Table 3). Also, marital status and having an under-5 child were positively associated with sleeping under an LLIN in both urban and rural models, but with slightly different effects (Table 3). The effect of being currently married or formerly married or having an under-5 child was slightly higher among urban women than rural women. Compared with unemployed women, women who were seasonally or occasionally employed were significantly more likely to sleep under an LLIN in urban areas but less likely to sleep under an LLIN in rural areas (Table 3). Household wealth was negatively associated with sleeping under LLINs in both urban and rural areas, but with some differences. Belonging to the richer or richest households was negatively associated with using an LLIN compared with the poorest households (Table 3). In rural areas, however, belonging to only the richest households was negatively associated with the use of LLINs. Region of residence was also significantly associated with the use of LLINs, but with rural–urban variation. Compared with the South West region of Nigeria, the prevalence of women’s use of LLINs was significantly higher in urban than rural areas of North Central, North East, North West and South East (Table 3). For urban women, residing in the South South region was not significantly associated with the use of LLINs. For rural women, residing in the South East or South South region was significantly associated with a lower likelihood of using the LLINs. Religion was not a significant contributor to either the urban or rural models (Table 3).
Discussion
By applying the Social Determinants of Health (SDH) framework and Health Belief Model (HBM), this study sought to examine the rural–urban dimensions of the perception of malaria severity and practice of malaria preventive measures using the 2018 Nigeria Demographic and Health Survey dataset. Almost half (49%) of the surveyed women who had the perception that malaria could lead to death slept under long-lasting insecticide-treated nets (LLINs) the night before the survey. Multiple reasons for non-use of LLINs, including discomfort due to heat and difficulty in hanging up the nets, have been reported elsewhere (Adebayo et al., Reference Adebayo, Akinyemi and Cadmus2014). Women’s likelihood of sleeping under an LLIN the night before the survey was significantly associated with their age, education level, marital status, having a child under 5 years, employment status, religion, place of residence (urban/rural), household wealth and region of residence. Although the perception of severe malaria leading to death was significantly higher, compared with the perception of severe malaria not leading to death, across both urban and rural residence, adjusting for the above socio-demographic factors resulted in significant rural–urban differences.
The study found that Nigerian women’s perception of the severity of malaria influences their use of LLINs differently in urban compared with rural areas. Specifically, having the perception that malaria could lead to death had no association with the use of LLINs in urban areas. In rural areas, however, agreeing that malaria could lead to death had an association with a lower likelihood of using LLINs. A qualitative exploration is therefore needed to understand why severity did not seem to increase the likelihood of treated bed net use in rural setting. Certain haemoglobinopathies such as sickle cell anaemia variously reduce the risk of developing malaria syndromes (Taylor et al., Reference Taylor, Parobek and Fairhurst2012). These haemoglobinopathies, which are also common among Nigerians, are highly prevalent in some human populations that are/were currently or historically exposed to the malaria parasite P. falciparum. For example, with a sickle haemoglobin (HbS) carrier prevalence of 25% to 40%, Nigeria bears the greatest burden of sickle cell disorder worldwide (Adewoyin et al., Reference Adewoyin, Busari and Aworanti2019). Therefore, these haemoglobinopathies may affect the perceived severity of malaria and use of preventive measures in Nigeria. From the perspective of the HBM alone, perceived severity of malaria is positively associated with the use of LLINs. However, after accounting for other socio-demographic factors in line with the SDH framework, the positive relationship observed in the bivariable model changed into negative, indicating that perceived severity has a negative relationship with the use of LLINs. Due to their unavailability in the dataset, it was not possible to control for variables that mimic the other components of the HBM (perceived susceptibility, perceived benefits, cues to action and self-efficacy). Therefore, it was impossible to conclude that the HBM alone was sufficient to understand the observed phenomenon. Generally, the observed rural–urban dichotomy in the influence of perceived severity of malaria on the use of the LLINs for sleep underscores the need to account for contextual implications in designing policies that influence people’s health beliefs and behaviours. Furthermore, as intimated in the SDH framework, people’s health practices and health literacies are influenced by where they live and work (World Health Organization, 2010; Committee on Educating Health Professionals to Address the Social Determinants of Health et al., 2016). Therefore, this rural–urban difference would have been lost if the study did not account for it, which has been a frequent practice in similar public health publications, in addition to their lack of control for the severity of malaria (Ameyaw et al., Reference Ameyaw, Adde, Dare and Yaya2020). Thus, the results also have lessons for data analysts using nationally representative data. They suggest that observation of a significant association, or lack of it, in studies that fail to account for the rural–urban divide may present an incomplete picture for policymakers.
Women’s age was found to be significantly associated with the use of LLINs, but with a rural–urban effect. Whereas age was a significant factor in the association in urban areas, it was not significant in rural areas. In urban areas, however, women who were older than the 15–24 years group had a lower likelihood of using LLINs. This suggests that adolescent and younger adult women in urban areas were more likely to use LLINs. This finding supports those of similar previous studies on the age–LLIN use association (Ameyaw et al., Reference Ameyaw, Adde, Dare and Yaya2020) but contradicts the findings of others (Singh et al., Reference Singh, Brown and Rogerson2013). Most young women (15–24 years) in urban areas may be in higher education institutions and may require LLINs to protect themselves from mosquito bites in their rented accommodation (Kudom & Mensah, Reference Kudom and Mensah2010). Nevertheless, it is important to note that malaria can have a devastating impact on the health of women as they age. Compared with their older counterparts, younger women are more likely to use LLINs, and this may affect the drive for malaria prevention and elimination in Nigeria. Younger women constitute a large part of the population, are caregivers of under-five children, and in early child-bearing age (Babalola et al., Reference Babalola, Sambo, Idris, Ajayi, Ajumobi and Nguku2019). Malaria preventive measures, in line with universal and continuous mass LLIN distribution campaigns targeting the entire population, should be intensified.
Despite formal education being significant in both urban and rural models, there were some differences in their contributions to the model. In the rural model, women who attained a secondary level education or higher were more likely to use LLINs, while this association was only significant in women with post-secondary education status in the urban setting. Although the rural–urban differences in education may not be explicitly explained, it is well-known that the opportunity for higher education is greater in urban than in rural areas, so post-secondary education may serve as a baseline qualification for most people. The role of education in influencing health behaviours is well-documented (Hahn & Truman, Reference Hahn and Truman2015; Shimaponda-Mataa et al., Reference Shimaponda-Mataa, Tembo-Mwase, Gebreslasie and Mukaratirwa2017; Oladimeji et al., Reference Oladimeji, Tsoka-Gwegweni, Ojewole and Yunga2019), as is its role in increasing the likelihood that households purchase or own LLINs (Deressa & Ali, Reference Deressa and Ali2009), since education and information are important drivers for change (Ezire et al., Reference Ezire, Adebayo, Idogho, Bamgboye and Nwokolo2015). Previous studies have indicated a positive association between education on the life history of mosquitoes and on the mechanism of control strategies with the use of LLINs (Kudom & Mensah, Reference Kudom and Mensah2010). In contrast, other studies have reported a negative association (Adebayo et al., Reference Adebayo, Akinyemi and Cadmus2014). Therefore, policymakers need to invest significantly in educating the general population at least to the secondary level. Tuition-free education such as the Free Secondary Education policy implemented in the neighbouring country of Ghana could be adopted and/or adapted, and it needs the commitment of policymakers since such policy requires more resources.
The study found that women who were currently married or formerly married or who had under-5 children were more likely to sleep under net among urban women than rural women. Generally, being married or having a partner or having under-5 children seems to be associated with positive health behaviours such as the use of LLINs at night. Previous studies have found a protective association between marital status and health-seeking behaviours (Umberson, Reference Umberson1992; Robards et al., Reference Robards, Evandrou, Falkingham and Vlachantoni2012; Hilz & Wagner, Reference Hilz and Wagner2018). Conversely, unmarried women may lack spousal support and be disadvantaged in access to resources compared with their married counterparts (Nkoka et al., Reference Nkoka, Chipeta, Chuang, Fergus and Chuang2019). Under-5 children, especially those being breastfed, have a higher likelihood of sharing a bed with their parents, thereby increasing the chances of both the woman and the child sleeping under an LLIN (Auta, Reference Auta2012). Women who are currently or formerly married are more likely to be pregnant and to have an under-5 child compared with those who had never been in a union. Specifically, urban women have more access to health care facilities and antenatal services providing peri-natal services, including education on LLIN use. The availability of LLIN distribution and/or sales points, and other factors such as marital status, may favour urban women. Policymakers may need to consider implementing couple-friendly interventions to improve LLIN uptake among rural women, as well as never-in-union women.
Compared with unemployed women, women who were seasonally or occasionally employed were significantly more likely to sleep under LLINs in urban areas but less likely to sleep under LLINs in rural areas. Generally, women who are seasonally or occasionally employed are more likely to have the economic power to purchase or own an LLIN than unemployed women. However, it is difficult to explain the rural–urban differences existing among seasonally or occasionally employed women. This calls for further studies, particularly qualitative studies, to explain the differences. More importantly, government and non-governmental organizations in Nigeria must adopt policies and programmes that encourage integrating malaria preventive measures into existing work benefits and structures.
The study found that household wealth was negatively associated with sleeping under an LLIN in both urban and rural areas, but with some differences. Belonging to the richer or richest households among urban women was negatively associated with using an LLIN. In rural areas, however, belonging to only the richest households was negatively associated with the use of the LLINs. In other words, richer people were less likely to use LLINs. Generally, rich households can provide decent houses that are well-fitted with mosquito nets for doors and windows and application of mosquito repellent formulae or insecticides to prevent mosquito bites, thereby reducing their need to use LLINs. Also, women from wealthy households usually reside in environments that hinder mosquito breeding, unlike their poor counterparts (Adedokun & Uthman, Reference Adedokun and Uthman2020). Therefore, urban women who are from richer or richest households may benefit from the protective association between household wealth and well-fitted, mosquito bite-preventive accommodation. However, regardless of the direction of the association, there is a need for the government and/or policymakers to increase efforts towards LLIN distribution mechanisms that accommodate socioeconomic differences in LLIN uptakes and use. The Nigerian government should implement pro-poor policy interventions and/or decent accommodation systems to improve rural–urban equity in ownership of decent housing, with the associated benefit of well-fitted door and window nets, as part of malaria preventive measures.
The study found region of residence to be significantly associated with the use of LLINs, but with a rural–urban difference. Previous studies in Nigeria have indicated that region of residence is the most significant predictor of LLIN use due to the heterogenous transmission of malaria across the country (Andrada et al., Reference Andrada, Herrera, Inyang, Mohammed, Uhomoibhi and Yé2019). Different studies have reported ownership of LLINs to be either low (Eteng et al., Reference Eteng, Mitchell, Garba, Ana, Liman, Cockcroft and Andersson2014; Alawode et al., Reference Alawode, Chima and Awoleye2019) or high (Tobin-West & Alex-Hart, Reference Tobin-West and Alex-Hart2011) in urban areas in Nigeria, and this could explain why this study found women in urban regions to have either high or low prevalences of LLIN use. Compared with the South West region, the North Central, North East, North West and South East regions had significantly higher prevalence estimates of women’s LLIN use in urban than rural areas. Previous studies have indicated that northern Nigeria generally has a significantly higher incidence of malaria, and number of new malaria cases, than southern Nigeria, possibly due to poor health care access and public health services in some areas of the north and the impact of the Rivers Niger and Benue, and even urban agricultural development that involves irrigation (Okunlola & Oyeyemi, Reference Okunlola and Oyeyemi2019). Therefore, people in northern Nigeria are more likely to use LLINs than their southern counterparts. Indeed, Okunlola and Oyeyemi (Reference Okunlola and Oyeyemi2019) reported greater coverage of LLINs in the North East region. Although it appeared to be the rainy season in the south and the dry season in the north of the country during the data collection, this study’s findings suggest that the seasonality of data collection may have little or no impact on LLIN use. It is expected that, during the rainy period, there will be increased breeding of mosquitoes, high exposure to malaria and a resultant, expected increase in the use of LLINs. However, these findings do not suggest an increased use of LLINs in the south, thereby suggesting that other factors may be at play beyond the season of data collection.
Regarding the higher use of LLINs among urban than rural women, poor health service delivery, lack of access and lack of health professionals posted to rural areas widen the gap for LLIN use sensitization and a resultant low use of LLINs in rural areas (Okunlola & Oyeyemi, Reference Okunlola and Oyeyemi2019). This study observed no significant association between religion and rural–urban residence. Therefore, there is no need for policymakers to devise interventions based on religion. However, further studies may consider regional analyses of this association to identify if there is any sub-national masking.
The main strengths of this study were that is was based on a large, nationally representative survey (2018 NDHS) and used standardized, analytic methodology. This means that the findings can be generalized to the entire population. Also, it employed complex sample analyses in accounting for sampling units and weighting. In addition, it unmasked rural–urban variations in the perception of malaria severity and the practice of malaria preventive measures in Nigeria. The main limitations of this study were its use of secondary data and its cross-sectional design. Therefore, causal relationships could not be inferred between the predictors and the outcome variables. It was also restricted to variables available in the NDHS data. Also, the NDHS data were collected in a predominantly rainy period in the south and dry period in the north of Nigeria, and these differences in seasonality could possibly have affected the results.
In conclusion, the study found that about 48% of Nigerian women slept under long-lasting insecticide-treated mosquito nets the night before the 2018 survey. Women who perceived that malaria could lead to death had a higher likelihood of using a treated bed net in the urban, rural and combined samples. However, after adjusting for other socio-demographic variables, the association between respondents’ perceived malaria severity and their use of treated bed nets was significant for rural Nigerian women only. Rural Nigerian women who perceived malaria to be severe had a lower likelihood of using treated bed nets. The study observed rural–urban variations in the relationship between socioeconomic and demographic variables and the use of treated bed nets. The results have implications for health policymaking towards improving the use of insecticide-treated bed nets as a malaria preventive measure, taking into consideration the socioeconomic stratifications of the Nigerian population as explained by the SDH framework, and by modifying factors, perceived threat (severity and susceptibility), benefits, barriers, self-efficacy and cues to action as postulated by the HBM. The Federal Government of Nigeria needs to implement pro-poor policies to improve wealth and educational opportunities across all regions, rural and urban areas as well as devise couple-friendly and employment-oriented strategies for malaria prevention.
Acknowledgment
The authors would like to thank the thank the Demographic and Health Survey (DHS) programme for their support and for permitting free access to the original data used in this study.
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Conflict of Interests
The authors have no conflicts of interest to declare.
Ethical approval
The authors obtained permission from the DHS program to use the dataset after a simple request-access registration at sprogram.com/data/dataset_admin/index.cfm. The DHS indicated that it obtained written and verbal consent from all eligible participants before their data were collected (National Population Commission & ICF, 2019).





