Introduction
Birth weight plays a pivotal role not only to the wellbeing of infants but also to their psychosocial development and chances of survival (WHO and UNICEF 2004). Moreover, it provides valuable insights into maternal and foetal health issues, such as maternal nutrition, pregnancy-related complications, and access to comprehensive obstetric care, all of which are predictors of a healthy pregnancy and baby (WHO 2023a). Low birth weight (LBW), which is defined as birth weight below 2 500 g, is an important indicator of public health that strongly correlates with neonatal and under-five mortality risks (Vilanova et al., Reference Vilanova, Hirakata, Buriol, Nunes, Goldani and Silva2019; Watkins et al., Reference Watkins, Kotecha and Kotecha2016; WHO 2023b). It encompasses two categories: preterm births (those born before 37 completed weeks of gestation) and small-for-gestational-age (SGA, which describes an infant whose weight is below the 10th percentile for gestational age based on country and sex standards).
LBW has been linked to numerous health challenges throughout the life course of those affected (WHO and UNICEF 2004). According to the World Health Organization (WHO), LBW affects approximately 15–20% of all births worldwide – approximately 20 million births annually (WHO 2014). The consequences of LBW are far reaching beyond infancy, as many survivors face both immediate and long-term complications. For instance, LBW is associated with neonatal death, prolonged hospital stay after birth, severe infections, cognitive dysfunction, and increased vulnerability to hypertension and type II diabetes later in life (Jornayvaz et al., Reference Jornayvaz, Vollenweider, Bochud, Mooser, Waeber and Marques-Vidal2016; Calkins and Devaskar Reference Calkins and Devaskar2011). In addition to these health issues, other medical complications related to LBW include cerebral palsy, retinopathy of prematurity, and other neurological problems. These complications put further strain on healthcare systems that are overstretched by limited resources (Gu et al., Reference Gu, Wang, Liu, Luo, Wang, Hou, Nkomola, Li, Liu, Meng, Zhang and Song2017; El Adam et al., Reference El Adam, Hutcheon, McLeod and McGrail2022; Canadian Institute for Health Information 2009; Saskatchewan Ministry of Health 2019; UNICEF 2023).
Previous studies have linked LBW to factors contributing to prematurity and/or intrauterine growth restriction (Krasevec et al., Reference Krasevec, Blencowe, Coffey, Okwaraji, Estevez, Stevens, Ohuma, Conkle, Gatica-Domínguez, Bradley, Muthamia, Dalmiya, Lawn, Borghi and Hayashi2022; Zohdi et al., Reference Zohdi, Sutherland, Lim, Gubhaju, Zimanyi and Black2012). These include extremes of maternal age, maternal low body mass index, tobacco and alcohol use during pregnancy, multiple pregnancy, obstetric complications, presence of comorbidities (such as hypertension and renal diseases), placental insufficiency, foetal abnormalities, and environmental pollution (Canadian Institute for Health Information 2009; Hüseyin et al., Reference Hüseyin, Muazzez and Yadigar2020; S. Moore et al., Reference Moore, Daniel and Auger2009; Saskatchewan Ministry of Health 2019; El Adam et al., Reference El Adam, Hutcheon, McLeod and McGrail2022; WHO and UNICEF 2004). Recently, increased use of in vitro fertility treatment and delivery procedures such as induction of labor and caesarean delivery (especially among high-risk pregnancies), have been correlated with LBW (Gunby et al., Reference Gunby, Bissonnette, Librach and Cowan2009; Iams et al., Reference Iams, Romero, Culhane and Goldenberg2008; Chen et al., Reference Chen, Wu, Zhang, Zou, Li and Fan2015; Hüseyin et al., Reference Hüseyin, Muazzez and Yadigar2020; Gorgui et al., Reference Gorgui, Sheehy, Trasler and Bérard2022; L. E. Moore et al., Reference Moore, Haijhosseini, Motan and Kaul2023). Other contributors to LBW are unemployment, poverty, and limited access to prenatal care services (Solomon and Hill Reference Solomon and Hill2020; ‘Infant Health’ 2019; ‘OECD INDICATORS’ 2019; Canadian Institute for Health Information 2009).
LBW has been consistently recognized as a public health priority by the WHO, and its significance has increased since the implementation of the Global Nutrition Targets in 2012 (WHO 2014). During the 65th World Health Assembly (WHA), Canada and other countries approved an action plan to promote maternal, infant, and young child nutrition and reduce global burden of LBW by 30% between 2012 and 2025. The ambitious goal is to reduce the global burden of babies with LBW from 20 million in 2012 to 14 million by 2025, translating to a 3% annual decrease in LBW rates (WHO 2014). This target closely aligns with the Sustainable Development Goal (SDG) 2, which aims to eradicate all forms of malnutrition across all age groups and prevent low birth weight in newborns.
While Canada has historically had one of the lowest LBW rates among the G7 countries (Canada, France, Germany, United Kingdom, Italy, United States, and Japan) (World Health Organization 2023) and significantly below the global average of 14.7% (UNICEF 2023), the rise in LBW rates from 5.6% to 6.6% between 2000 and 2020 warrants attention (World Health Organization 2023; Government of Canada 2016). Moreover, Canada’s position among the 37 Organization for Economic Cooperation and Development (OECD) countries declined from 12th in 2000 to 17th in 2020 (World Health Organization 2023). This slight increase in LBW could indicate underlying issues that might worsen if not proactively addressed.
The recent increase in LBW rate in Canada has been attributed, in part, to recent changes in the population dynamics of women in the reproductive age group. These changes were due to increased immigration (Urquia et al., Reference Urquia, Frank, Glazier and Moineddin2007; Lee et al., Reference Lee, Hinds and Urquia2020; The Conference Board of Canada 2023), heightened risk among Indigenous population (The Conference Board of Canada 2023), and the rise in assisted reproduction among women aged 40 years and above (The Conference Board of Canada 2023; OECD 2019; Gorgui et al., Reference Gorgui, Sheehy, Trasler and Bérard2022; L. E. Moore et al., Reference Moore, Haijhosseini, Motan and Kaul2023).
Apart from the disparities in LBW rates across countries, variations exist within Canada. Of all the births in Canada in 2017, Nunavut had the highest rate of LBW at 7.8%, closely followed by Alberta at 7.2% (Statistics Canada 2018). Conversely, the lowest rates were observed in Newfoundland and Labrador (5.4%), British Columbia (5.8%) and the Northwestern Territories (5.9%) (Statistics Canada 2018). For the same year, the LBW rate in Saskatchewan was 6.2%.
Despite the regional variations appearing modest, the Saskatchewan’s LBW rate reflects inequity in health care for equity-deserving groups such as Indigenous populations, which perennially face higher rates of health disparities including LBW (Halseth and Greenwood Reference Halseth and Greenwood2019).
According to the 2019 Saskatchewan Ministry of Health report (Saskatchewan Ministry of Health 2019), in 2014, LBW varied across the former regional health authorities (RHA) with the highest rate found in northern Saskatchewan’s Mamawetan Churchill River (8.0%), and lowest rate in southern Saskatchewan’s Five Hills (4.3%). The overall LBW share of births in Saskatchewan for that year was 5.8%. The underlying reasons for the disparities between northern and southern Saskatchewan in LBW rates have not been fully elucidated. However, several potential factors have been identified. One possible contributing factor for the disproportionately high LBW rate in northern Saskatchewan is the unequal access to prenatal care, particularly specialized care for high-risk pregnancies in many rural and remote communities (Canadian Institutes for Health Information (CIHI) 2013; Soloducha Reference Soloducha2018). Furthermore, in northern Saskatchewan, where Indigenous communities are predominantly located, Indigenous women are more susceptible to LBW due to higher rates of chronic diseases such as diabetes, hypertension, obesity, as well as socio-economic disadvantages, and the enduring effects of historical marginalization (Indigenous Services Canada, n.d.; Irvine et al., Reference Irvine, Quinn and Stockdale2011; Halseth and Greenwood Reference Halseth and Greenwood2019).
Canada has implemented several policies in recent years to improve perinatal health outcomes. One of such policy is the Canada Prenatal Nutrition Programme (CPNP), a national community-based programme launched in 1995 by the Public Health Agency of Canada (Government of Canada 2023). The CPNP aims to promote the health of vulnerable pregnant women, new parents, and their babies by working with community-based groups, agencies, and coalitions to provide prenatal and postnatal health promotion, referrals to community services, breast feeding education and support, and nutrition counselling and prenatal vitamins. Similarly, the moms and kids health programme (Moms & Kids Health Saskatchewan 2023) in Saskatchewan provides culturally responsive prenatal initiatives such as nutritional support, housing assistance, mental health services, and treatment for substance use for pregnant women and their families. However, there is a need for an assessment of these health programmes, as empirical evidence on their impact, particularly regarding the occurrence of LBW in Saskatchewan, remains scarce.
Given the significance of LBW and its long-term impacts, it is important to monitor and understand the trend. The objective of this study was therefore to examine the trends and geographical variations in LBW rates over a 20-year period from 2002/2003 to 2021/2022 in the province of Saskatchewan. This study also assessed whether there were continuous changes in LBW rates over this period and if these changes were consistent. The result of this study will help develop action plans, establish accountability measures, and monitor progress of LBW in Saskatchewan.
Methods
Study location
Saskatchewan is a landlocked province located in western Canada and shares borders with the United States to the south, Alberta to the west, Manitoba to the east, Nunavut to the northeast, and the Northwest Territories to the north. According to the Statistics Canada, the population of Saskatchewan in 2021 stood at 1.13 million people, accounting for approximately 3.1% of the total Canadian population (Statistics Canada 2023). However, the population distribution within the province is not uniform. Most Saskatchewan residents are concentrated in the southern part of the province, particularly in major cities like Saskatoon and Regina. Contrarily, the northern part of the province is sparsely populated, and its residents are majorly Indigenous populations (over 85%) (Irvine et al., Reference Irvine, Quinn and Stockdale2011). The northern residents are faced with challenges accessing healthcare services, which are primarily concentrated in southern Saskatchewan (Irvine et al., Reference Irvine, Quinn and Stockdale2011). Similar to the rest of the country, Saskatchewan operates a publicly funded healthcare system that offers comprehensive coverage for medical services. The administration of healthcare services throughout the province is overseen by the Saskatchewan Health Authority (SHA), which was established in 2017. The SHA serves as the singular health region, after the amalgamation of the Athabasca and 12 regional health authorities that previously operated in the province (Winiewski Reference Winiewski2017).
Study design
This ecological time-series study examined and quantified changes in LBW rates in the province of Saskatchewan over a period of 20 fiscal years, from 2002/2003 to 2021/2022. A joinpoint regression analysis was used to analyse aggregated LBW rates (operationalized as birth weight <2 500g per 100 live births) for both the Canadian and Saskatchewan populations. These rates were obtained from the online data repository of the Canadian Institute for Health Information (CIHI 2023).
Joinpoint regression analysis is a statistical method that automatically identifies significant points where the linear slope of a trend changes over time. To identify these inflection points and analyze the trends, a log-linear model was used at a significance level of α=0.05. The assumption of normality of the data was verified with Shapiro–Wilk test (p> 0.05), and the sample size is adequate (≥10). Also, the presence of serial autocorrelation was examined, but no evidence of autocorrelation was found.
The rationale for using joinpoint regression analysis was based on the study objective and nature of the dataset. Unlike the traditional regression model, joinpoint regression is particularly well-suited for analyzing data with multiple segments or distinct periods of change, as it allows for the identification of points in time where a significant change in the trends occurs. In order words, it helps to pinpoint locations in the time series where breakpoints occur, allowing further investigation into underlying determinants of population change.
The analyses were conducted at three distinct levels: national (Canada), provincial (Saskatchewan), and regional. The regional-level LBW rates were estimated using aggregated data, obtained from the CIHI at the level of former health regions in Saskatchewan (i.e. Athabasca and previous 12 health regions) (Statistics Canada 2017). The former health regions were grouped into seven categories (informed by the COVID-19 reporting zones) (Hill Reference Hill2020; Solomon and Hill Reference Solomon and Hill2020). The Far North group included Athabasca, Keewatin Yatthé, and Mamawetan Churchill River Health Regions. The North group included Prairie North, Prince Albert Parkland, and Kelsey Trail Health Regions. The Central West group represented Heartland Heath Region, while Central East group comprised the Sunrise Health Region. In addition, there were individual groups for Saskatoon, Regina Qu’Appelle, and the Southern group, which included Cypress, Five Hills, and Sun Country Health Regions. LBW rates for the new broader regional groupings were estimated using average rates reported for the previous health regions. For the analysis at the regional level, data from 2015/2016 to 2021/2022 were used due to limited data availability. It is noteworthy that this time frame represents a shorter period than the broader dataset available at the national and provincial levels (2002/2003–2021/2022).
This study utilized Joinpoint Regression Programme version 5.0.2, a statistical software tool that was developed by the Surveillance Research Programme of the National Cancer Institute (National Cancer Institute 2023). The annual percent change (APC) was estimated for each trend segment. It represents the annual rate of change and indicates the degree of trend intensity within a specific period of time. In addition, the average annual percent change (AAPC) was calculated to succinctly summarize the overall trend throughout the study period. The AAPC was derived by averaging the APC obtained from the joinpoint model, with the weight of each APC corresponding to the duration of the respective interval. The AAPC is a valuable statistic for comparing temporal trends across multiple populations. In the absence of turning points, the APC corresponds to the AAPC.
The selection of the most suitable joinpoint model was guided by the weighted Bayesian information criterion (BIC). The BIC was weighted by the duration of each interval, taking into account the possibility of overfitting. The grid search method was used to determine the optimal number and placement of inflection points. The BIC was then used to compare models with different numbers of inflection points, with a lower BIC indicating a better fit.
To ensure the robustness of the results, a resampling procedure was performed, generating 10 000 resamples of the selected model. This method is particularly useful for minimizing overfitting and providing a more accurate estimate of the uncertainty around the joinpoints. It is important to note that while LBW is commonly defined by the WHO as newborn weighing less than 2 500 g for the purpose of international comparability, in certain settings, LBW is defined as newborn weighing 500 g to 2 500 g. To assess the robustness of including extremely low birth weight infants in this study, a sensitivity analysis was conducted. In the sensitivity analysis, joinpoint regressions were performed with the aggregated LBW rates, which excluded babies weighing less than 500 g.
To visualize rates for the most recent period (2021/2022) and identify spatial patterns, a choropleth map was generated using QGIS software version 3.20.0 (QGIS Development Team 2020). Additionally, regions with notable trends were identified. A 95% confidence interval (CI) was used to assess statistical significance.
Results
Provincial comparison with national trend
Between 2002/2003 and 2021/2022, the province of Saskatchewan experienced a lower incidence of LBW, with an average rate of 5.7%, in contrast to the national average rate of 6.2%. Of note, in 2002/2003, the LBW rate in Saskatchewan was 5.2%, similar to the national rate (Figure 1). However, over time, both rates showed a gradual upward trend. In the most recent period (2021/2022), Saskatchewan saw an increase in its LBW rate, reaching 6.5%, which remained slightly below the national rate of 6.8%. For the 20-year period of 2002/2003 through 2021/2022, the rates increased by 1.0% per year in Saskatchewan (AAPC= 1.0%, 95% CI: 0.6% to 1.3%). For the same period, the national rate had a comparatively higher annual incremental rate (AAPC= 1.4%, 95% CI: 1.2% to 1.6%).

Figure 1. Low Birth Weight Rates in Canada and Saskatchewan, 2002/2003–2021/2022.
AAPC: Average annual percentage of change, CI: Confidence interval
Over the years, there has been a significant increase in the incidence of LBW at both the provincial and national levels. It is worth highlighting specific periods of significant changes that occurred at 2011/2012 and 2004/2005 for Saskatchewan and Canada, respectively (see Figure 2). In Saskatchewan, LBW rates were relatively stable from 2002/2003 to 2011/2012, showing a barely noticeable trend (APC= 0.1%, 95% CI: -3.0% to 0.9%). However, the trend changed drastically after 2011/2012, with a significant increase in LBW rates. The rates increased by 1.8% per year between 2011/2012 and 2021/2022 (APC= 1.8%, 95% CI: 1.1% to 4.6%). Consequently, the Saskatchewan’s rates increased from 5.5% in 2011/2012 to 6.5% in 2021/2022. At the national level, LBW rates in the first period (2002/2003 to 2004/2005), increased significantly by 5.7% per year (APC= 5.7%, 95% CI: 3.2% to 7.8%). In the following period from 2004/2005 to 2021/2022, the rates continued their upward trend, increasing by 0.9% per year (APC= 0.9%, 95% CI: 0.7% to 1.0%), albeit at a comparatively moderate pace.
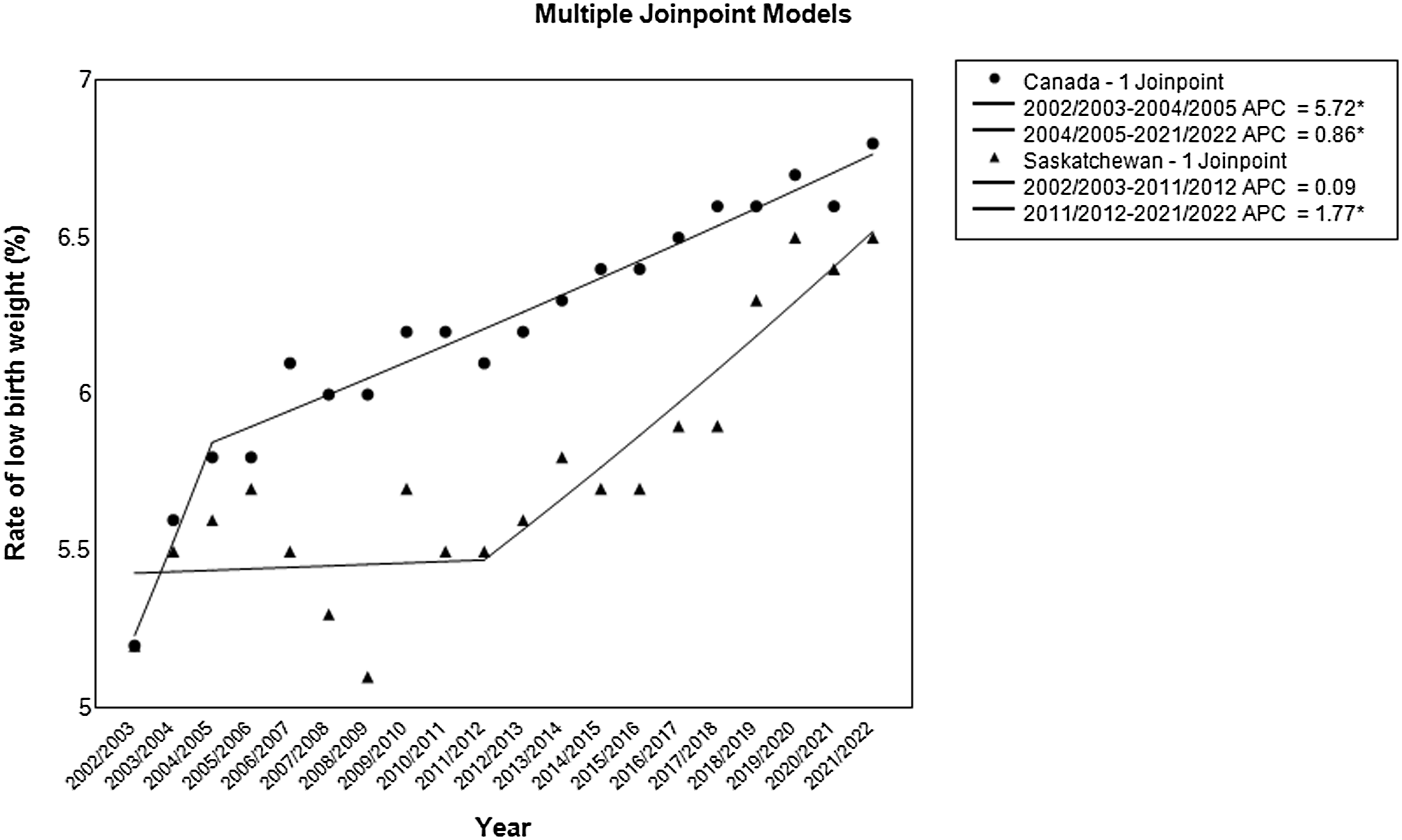
Figure 2. Low Birth Weight Rates in Canada and Saskatchewan with Inflection Points, 2002/2003–2021/2022.
APC: Annual percentage change
For sensitivity analysis, the LBW rate of infants weighing between 500 g and 2 500 g were found to be strikingly similar to those estimated for infants weighing less than 2 500 g. In Saskatchewan and Canada, the average LBW rates were 5.7% and 6.1%, respectively. The overall AAPC produced comparable results to those obtained with the inclusive sets (< 2500g). There was a single joinpoint for Canada and Saskatchewan. Although Saskatchewan exhibited a similar inflection point and APC, Canada experienced a significant jointpoint a little later, around 2006/2007. For the sensitivity analysis, the upward trend in LBW was comparatively less pronounced in Canada between 2002/2003 and 2006/2007, with an APC of 3.29% (95% CI: 2.4% to 4.8%) and an APC of 0.83% (95% CI: 0.7% to 1.0%) thereafter (2006/2007 to 2021/2022).
Regional trend
According to Figures 3 and 4, the Far North region of Saskatchewan experienced the highest incidence of LBW in 2021/2022 at a rate of 9.2%. On the contrary, the Central West region recorded the lowest rate at 4.3% during the same time. During this time, the Far North region and Regina surpassed the provincial average by having higher LBW rates, with relative risk (RR) of 1.4 for Far North and RR of 1.2 for Regina Qu’Appelle. This means that children delivered in the Far North region were 1.4 times more likely to have LBW, and those in Regina Qu’Appelle were 1.2 times more likely to have LBW, compared to the average risk in the province in 2021/2022.

Figure 3. Low Birth Weight Rates in Canada, Saskatchewan, and Region-Specific Trends, 2015/2016–2021/2022.

Figure 4. Spatial Distribution of Low Birth Weight Rates and Trend in Saskatchewan, 2015/2016–2021/2022.
The temporal patterns of LBW incidence varied across the spatial units studied, as shown in Table 1. In general, most regions showed consistent LBW rates over time, apart from the Central East, Southern, and Regina Qu’Appelle regions. Between 2015/2016 and 2021/2022, these three regions experienced a significant upward trend in LBW rates (Figure 4). The Central East region showed the highest trend in the LBW rates, increasing by 5.7% per year from 4.1% in 2015/2016 to 5.8% in 2021/2022 (AAPC= 5.7%, 95% CI: 1.7% to 9.7%). The southern region followed closely behind with an AAPC of 4.3% (95% CI: 0.5% to 8.4%), whereas Regina Qu’Appelle observed the lowest annual incremental rate at 3.5% (95% CI: 0.5% to 6.6%). Table 1 highlights a significant shift in LBW rates in the southern region between 2015/2016 and 2018/2019. An increase from 4.2% to 6.6% was observed during this period (APC: 14.1%, 95% CI: 7.2% to 30.3%). Subsequently, the rates stabilized, denoted by an AAPC of -4.6% (95% CI: -16.3% to 1.6%).
Table 1. The Region-Specific Trends in the Rates of Low Birth Weights, Saskatchewan, 2015/2016–2021/2022

a Aggregated sub-provincial dataset was available from 2015/2016 to 2021/2022.
b Estimates were significantly different from zero (p<0.05).
Discussion
Over the past 20 years (2002/2003 to 2021/2022), LBW rates increased significantly at both the provincial and national levels. An inflection point was observed during this study period: 2004/2005 for Canada and 2011/2012 for Saskatchewan. Also, LBW rates varied across the regions of Saskatchewan, with rates in the Far North and Regina Qu’Appelle exceeding the provincial rate in 2021/2022. The Regina, southern, and central-eastern regions saw significant increasing trends in the entire study period.
The findings on the upward trend in LBW rates in Saskatchewan and Canada are consistent with previous studies in other high-income countries (Huda et al., Reference Huda, Callaway, Jackson, Fatima, Cumming, Biswas, Paz, Boyle, Sly and Mamun2023; Pollock et al., Reference Pollock, Gennuso, Givens and Kindig2021). Notably, LBW rates in Saskatchewan were slightly below the national average. However, Saskatchewan saw an increase in the LBW rate from 5.2% in 2002/2003 to 6.5% in recent years (2021/2022), bringing it closer to the national rate of 6.8%. Initially, Saskatchewan maintained stable LBW rates with an average annual change of 0.1%, whereas the national average annual change was 5.7%. In more recent years, the average annual change for Saskatchewan of 1.8% surpassed the national rate of change of 0.9%. This suggests a convergence towards the national trend, although the reasons for this recent shift remain unclear.
Interestingly, the inflection points in LBW rates occurred earlier at the national level (2004/2005) compared to Saskatchewan (2011/2012) and neither coincided with specific programmatic or policy changes. Further analysis conducted to understand the underlying mechanisms driving these trends shows that Saskatchewan had a higher annual rate of increment in preterm births, SGA babies, and caesarean sections compared to Canada for those periods (Supplementary Table). This disparity might help explain the convergence of LBW rates. The overall caesarean rates in Saskatchewan increased by 2.0% per year from 2002/2003 to 2021/2022, while caesarean rates in Canada increased by 1.5% per year over the same period. Likewise, the annual increase in SGA and preterm births between 2007/2008 and 2021/2022 was higher in Saskatchewan than in Canada (SGA: 1.0% in Saskatchewan vs. 0.8% in Canada, preterm births: 1.4% in Saskatchewan vs. 0.2% in Canada).
There is considerable evidence that LBW is associated with caesarean section (Chen et al., Reference Chen, Wu, Zhang, Zou, Li and Fan2015; Moreira et al., Reference Moreira, de Sousa and Sarno2018; Hüseyin et al., Reference Hüseyin, Muazzez and Yadigar2020; Coutinho et al., Reference Coutinho, Cecatti, Surita, Costa and Morais2011), preterm birth (Krasevec et al., Reference Krasevec, Blencowe, Coffey, Okwaraji, Estevez, Stevens, Ohuma, Conkle, Gatica-Domínguez, Bradley, Muthamia, Dalmiya, Lawn, Borghi and Hayashi2022; Zohdi et al., Reference Zohdi, Sutherland, Lim, Gubhaju, Zimanyi and Black2012), and foetal growth restriction (Krasevec et al., Reference Krasevec, Blencowe, Coffey, Okwaraji, Estevez, Stevens, Ohuma, Conkle, Gatica-Domínguez, Bradley, Muthamia, Dalmiya, Lawn, Borghi and Hayashi2022; Zohdi et al., Reference Zohdi, Sutherland, Lim, Gubhaju, Zimanyi and Black2012). Premature births can occur for various reasons. Approximately 30% of preterm births are medically indicated and may involve the use of caesarean section or induction of labour (Iams et al., Reference Iams, Romero, Culhane and Goldenberg2008). These procedures are performed when there are serious risks to the mother or foetus, such as preeclampsia, eclampsia, maternal bleeding, intrauterine growth restriction, or foetal distress. The remaining 70% of premature births occur spontaneously and can also be caused by foetal distress or poor intrauterine growth (Iams Reference Iams2003). Furthermore, the steady rise in fertility rates and multiple births among older women who conceived through assisted reproductive technology (Gunby et al., Reference Gunby, Bissonnette, Librach and Cowan2009; Statistics Canada 2020; Saskatchewan Ministry of Health 2019; L. E. Moore et al., Reference Moore, Haijhosseini, Motan and Kaul2023; Gorgui et al., Reference Gorgui, Sheehy, Trasler and Bérard2022) and the marked increase in foetal monitoring and surveillance to detect early warning signs of distress might have contributed somewhat to the increase in LBW rates due to preterm birth (Canadian Institute for Health Information 2009).
In addition to health-related factors, social factors such as maternal age, dietary habits, socioeconomic status, and health-seeking behaviours influence maternal and child health outcomes. Although this study did not examine these social factors, previous studies have reported that factors affecting LBW were socio-economic disadvantage, social separation, maternal age under 20 years or over 40 years, and previous stillbirth (Muhajarine and Vu Reference Muhajarine and Vu2009; Government of Canada 2016; Urquia et al., Reference Urquia, Frank, Glazier and Moineddin2007). Other studies have also reported higher rates of LBW among immigrants in Canada and elsewhere (El Adam et al., Reference El Adam, Hutcheon, McLeod and McGrail2022; Catov et al., Reference Catov, Lee, Roberts, Xu and Simhan2016; Canadian Institute for Health Information 2009; S. Moore et al., Reference Moore, Daniel and Auger2009). Due to the recent increase in the immigrant population in Canada, there is a tendency to misclassify infants born to immigrant mothers as SGA, even if they are of appropriate size compared to their ethnic-specific foetal growth standard (El Adam et al., Reference El Adam, Hutcheon, McLeod and McGrail2022; Catov et al., Reference Catov, Lee, Roberts, Xu and Simhan2016; Canadian Institute for Health Information 2009; S. Moore et al., Reference Moore, Daniel and Auger2009).
This study found significant differences in LBW rates across Saskatchewan. In 2021/2022, LBW rates ranged from 4.3% in the Central West region to 9.2% in the Far North region. The prominent LBW rates in the Far North may be partly explained by the significant numbers of Indigenous populations in the region (Irvine et al., Reference Irvine, Quinn and Stockdale2011). Due to historical traumas and effect of colonization, Indigenous women are more prone to adverse perinatal health events. In northern and rural Saskatchewan, where transportation system and accessibility to skilled health workers are still huge challenges, adverse birth outcomes are not uncommon. Addressing structural and social barriers facing pregnant women in these hard-to-reach areas provides opportunities to mitigate the risks of adverse perinatal outcomes.
Although LBW rate was highest in the Far North in 2021/2022, the region, along with other regions like the North, Central West and Saskatoon, showed stable trends in LBW rates over the study period. Also, the Southern region presented a more complex trend with a significant joinpoint identified in 2018/2019. From 2015/2016 to 2018/2019, the Southern region experienced a steep rise in LBW rates. However, from 2018 to 2021/2022, the trend reversed to a stable pattern. These findings highlight the need for continuous monitoring of maternal and child health outcomes in these regions to ensure that the rates remain stable or decrease. Conversely, the Southern, Central East, and Regina Qu’Appelle regions demonstrated significant increasing trend over the entire study period. These findings highlight areas where targeted interventions may be necessary to address factors contributing to the increase in LBW. The increasing trend in those regions is a cause for concern. The different trends observed across the regions may be due to the extent to which maternal and child health policies and programmes were implemented in Saskatchewan prior to December 2017, when the previous health regions were merged into a single health region. Furthermore, these regions are characterized by high levels of urbanization and economic development (Leader et al., Reference Leader, Catherwood and Exner-Pirot2021), which can have positive and negative effects on maternal and child health. Urbanization and economic development can improve access to health services and increase health literacy. On the other hand, urbanization and economic development can also bring environmental pollution, traffic congestion, social isolation, stress, and unhealthy lifestyles, which have detrimental effects on maternal and child health. Therefore, further research is needed to explore the complex relationships between urbanization, economic development, and LBW in these regions.
This study has several strengths, particularly the use of a population-based dataset on LBW rates that captured all live births in Saskatchewan over a 20-year period. This dataset was representative of the entire population of Saskatchewan and lends itself to a high degree of generalizability across the province. The use of aggregated data accurately captured regional trends, avoiding the limitations imposed by sample size constraints. Also, the sensitivity analysis revealed remarkably similar findings between infants weighing between 500 g and 2 500 g and the inclusive set (<2 500 g), suggesting that variations in LBW definitions did not significantly impact the estimates. However, due to the inherent limitations of secondary data analysis, it is important to interpret study results with caution. One of these limitations is the reliance on administrative data. These sources might have omitted some children, potentially affecting the accuracy of the estimates. In addition, the study used joinpoint regression analysis to identify key change points in LBW trends over time. Although this method is invaluable for detecting trend shifts, paucity of data on the potential confounding factors of LBW such as maternal age, education, anthropometry, and smoking habits during pregnancy have prevented it from providing a causal explanation of the underlying factors and mechanisms that trigger these changes. Therefore, it is appropriate to interpret the observed temporal trends with caution as other unmeasured factors might have contributed to the observed patterns. While this study did not examine the effect of maternal smoking, it is unlikely that it explains the increase in LBW rates observed over time. Recent findings from Saskatchewan show a notable decline in smoking prevalence among women from 1999 to 2020 (University of Waterloo 2020). Typically, an increase in smoking rates would imply a decrease in LBW rates, not the contrary.
The findings from this study have implications for public health policy and practice in Saskatchewan and beyond. The increasing trends in Canada and Saskatchewan, along with the geographical disparities within the province, serve as a critical reminder to local public health authorities and other countries that tailored interventions are essential to addressing the multifaceted challenges associated with LBW. Also, active surveillance of maternal and child health indicators is needed at the sub-national levels to identify potential hotspots and address unique geographical challenges influencing maternal and child health outcomes. Regions with stable trend may benefit from maintaining or scaling up of current health initiatives and ensuring continued access to perinatal care. In contrast, regions that experienced increased trend would require targeted interventions to mitigate risk factors contributing to higher rates of LBW. Furthermore, more research is needed to identify and address the underlying mechanisms that contributed to these changes in order to inform evidence-based interventions and policies that promote healthier pregnancies and births across Saskatchewan.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0021932024000336
Data availability
Publicly available datasets were analysed. The datasets can be found at the CIHI website (CIHI 2023).
Acknowledgements
Not applicable.
Author contributions
Conceptualization and methodology: DAA; formal analysis: DAA; writing – original draft: DAA; interpretation, writing, review, and editing: DAA. The author has read and agreed to the submission of the manuscript. The views expressed in this article are solely that of the author and does not necessarily reflect the views of the author’s institution.
Funding statement
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Competing interests
The authors have no conflicts of interests.
Ethical standard
Ethical approval was not required for this study because all data were publicly available. The rates used in these analyses were aggregated in the public domain to ensure anonymization and confidentiality. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







