Introduction
Borderline personality disorder (BPD) is a mental health diagnosis characterised by a pervasive pattern of instability of interpersonal relationships, self-image, affect, and marked impulsivity (American Psychiatric Association, 2005). BPD is typically characterised by patterns of cognitive, emotional and behavioural dysregulation that often manifests in self-harm and suicidal behaviours (Kuo et al. Reference Kuo, Korslund and Linehan2006). BPD can be a life-threatening mental health condition estimated to be present in 0.7–1% of the general population (Torgersen et al. Reference Torgersen, Kringlen and Cramer2001; Jackson & Burgess, Reference Jackson and Burgess2004; Coid et al. Reference Cronin and Bourke2006). Individuals with a BPD diagnosis typically exhibit self-harming behaviours, with lifetime rates of ~70% for acts of self-injury, 80% for suicide attempts and 10% for suicide reported. As a result, quality of life is found to be severely impaired in this population (Giesen-Bloo et al. Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz2006; Palmer et al. Reference Palmer, Davidson, Tyrer, Gumley, Tata, Norrie, Murray and Seivewright2006).
Due to the chronic nature of BPD, this client group tend to use health care resources more extensively than individuals with other personality disorders or with major depression (Zanarini et al. Reference Zanarini, Frankenburg, Khera and Bleichmar2001; Bender et al. Reference Bender, Skodol, Pagano, Dyck, Grilo, Shea, Sanislow, Zanarini, Yen, McGlashan and Gunderson2006). More frequent and continued use of outpatient and inpatient treatment and high use of prescribed psychotropic medication is reported for persons with BPD (Zanarini et al. Reference Zanarini, Frankenburg, Khera and Bleichmar2001; Bender et al. Reference Bender, Skodol, Pagano, Dyck, Grilo, Shea, Sanislow, Zanarini, Yen, McGlashan and Gunderson2006). In addition, there is a strong relationship between BPD and poor occupational functioning (Skodol et al. Reference Skodol, Gunderson, McGlashan, Dyck, Stout, Bender, Grilo, Shea, Zanarini, Morey, Sanislow and Oldham2002; Jackson & Burgess, Reference Jackson and Burgess2004). Therefore, this client group is characterised by recurring crises, hospitalisations, self-harm, suicide attempts, addictions, episodes of depression, anxiety and aggression and lost productivity, explaining why BPD is considered one of the most expensive mental health disorders (van Asselt et al. Reference van Asselt, Dirksen, Arntz and Severens2007; Soeteman et al. Reference Soeteman, van Roijen, Verheul and Busschbach2008).
Recent cost-of-illness (COI) studies of BPD in Spain and the Netherlands report that BPD is associated with high COI, as well as indicating that the composition of costs vary considerably (van Asselt et al. Reference van Asselt, Dirksen, Arntz and Severens2007; Soeteman et al. Reference Soeteman, van Roijen, Verheul and Busschbach2008). Although there are variations in the identification of health care and societal costs in these studies, it is apparent that national variations in BPD treatment exist. For example, medications accounted for 2% of total costs in the Netherlands (Soeteman et al. Reference Soeteman, van Roijen, Verheul and Busschbach2008) but 25% in Spain (Salvador-Carulla et al. Reference Salvador-Carulla, Bendeck, Ferrer, Andion, Aragones and Casas2014). This suggests variations in national treatment strategies, although clinical guidelines for BPD (where they exist) advocate behavioural and community support in preference to hospitalisation and medication (e.g. National Institute for Health and Care Excellence, 2009). Given these variations in practice across jurisdictions, examinations of current practice are required on a country-by-country basis.
By the mid-2000s, procedures for recording epidemiological information about self-harm and suicide in Ireland had advanced (e.g. National Self-Harm Registry Ireland) (Flynn et al. 2018Reference Flynn, Kells and Joycea). However, the national government policy framework for mental health services and the national policy framework for suicide prevention activities are both over 10 years old (Health Service Executive, 2005; Government of Ireland, 2006). While the recent succession policy document for suicide prevention is welcome (Health Service Executive, 2015), it is important that decision-making is informed by economic information, ensuring appropriate allocation of scarce health care resources.
In 2006, the overall total economic and social cost of mental health problems in Ireland was estimated to be over three billion euro (O’Shea & Kennelly, Reference O’Shea and Kennelly2008). However, there is a dearth of condition-specific COI studies on mental health disorders in Ireland, a COI of schizophrenia being a notable exception (Behan et al. Reference Behan, Kennelly and O’Callaghen2008). BPD in particular, presents huge challenges for mental health services, and estimates suggest that it features in 11–20% of clinical presentations to mental health outpatient clinics in Ireland (Government of Ireland, 2006). In addition, it is recognised as the most difficult condition for clinicians to treat (Government of Ireland, 2006). This study provides insight on resource use and costs of treating BPD in mental health services in an Irish context, which is of considerable value in budgetary and service planning.
Methods
Design
This is a prevalence-based cost analysis study determining the direct health care costs of treating persons with BPD in Ireland.
Setting
Ireland’s public health service, the Health Service Executive (HSE), has responsibility for delivering all public health services in Ireland. There are four core areas of health service for the Irish population: acute hospitals, social care and disability, mental health and primary care. About 90% of mental health difficulties are addressed through the primary care system in Ireland, whereas the remaining patients require more specialist care which is accessed through mental health services (McDaid, Reference McDaid2013). This secondary level care for more complex mental health difficulties is delivered through multidisciplinary community mental health teams which offers specialised services for adults, children and adolescents, older people and intellectual disability (Government of Ireland, 2006). Multidisciplinary teams typically comprise of psychiatrists, clinical psychologists, social workers, community mental health nurses and occupational therapists. The secondary health care system was the setting for this study as specialist care for BPD is provided at secondary care level in Ireland.
Data collection and sample
At present, Ireland lacks an integrated health information system with unique patient identifiers. Therefore, a dedicated resource-use questionnaire was designed to capture the full range of secondary level care services utilised by individuals with BPD to facilitate the micro-costing analysis. While other resource use questionnaires exist (e.g. client socio-demographic and service receipt inventory) and have previously been used in Irish health service studies (Cronin & Bourke, Reference Coid, Yang, Tyrer, Roberts and Ullrich2017; Raftery et al. Reference Raftery, Burke, Murray, O’Duinn, Murray and Hallahan2017), given that standard BPD care requires such a broad range of services, it was important to capture a full ‘census’ of services so to speak. In designing the dedicated questionnaire, expert opinion from community mental health practitioners were elicited to ensure the full range of services available nationally were captured.
This study examines the cost of BPD, therefore non-BPD resource use is not collected or required. Information about the following resource use in the treatment of BPD was collected: acute hospital stay; emergency department presentation; ambulance use; number and duration of visits with multidisciplinary team members; type and quantity of medications.
Data on resource utilisation in the treatment of BPD was extracted from participants’ clinical files by their lead treating clinician. This minimised recall and reliability issues, which may ensue if relying on self-reported resource utilisation from participants. Extracting data directly from participants’ files allows the researchers to be confident that each participants’ contact with mental health services (e.g. acute inpatient, outpatient and emergency department) is accurately reported. However, it is necessary to acknowledge that in the absence of an integrated health information system, there may be instances where utilisation is not recorded, for example, where participants engage with health services outside their primary health service (e.g. presenting to the Emergency Department in another part of the country).
In total, 196 participants were recruited from nine geographically dispersed adult mental health services (AMHS) in urban and rural settings across the Republic of Ireland. Participants were mental health service users, aged 18–64 years, who had received a diagnosis, or met criteria for a diagnosis of BPD (DSM-IV) or emotionally unstable personality disorder (ICD-10). This paper is part of a larger study examining the effectiveness and cost-effectiveness of dialectical behaviour therapy (DBT) for treating individuals with BPD. The participants in this study include all recruited participants at baseline (see Flynn et al. 2018Reference Flynn, Kells, Joyce, Suarez and Gillespieb for study protocol).Footnote 1 Data collection occurred between February 2014 and March 2016. Participants in this study were recruited from secondary care services at multiple geographically dispersed sites across the Republic of Ireland. This sample is representative of the most complex individuals with a formal diagnosis and availing of specialist services. Therefore, the sample accurately depicts the potential costs to the health service if all individuals with a formal diagnosis were actively engaging with secondary level care.
Of the 196 participants, 81% were female. Ages ranged from 18 to 64, with 30% and 29% of participants in the 35–44 and 25–34 age categories, respectively. In all, 44% of participants were single; 18% married; 23% in a relationship and the remainder were divorced, separated or did not specify marital status. In all, 21% of participants were in full or part-time employment, with the remainder being unemployed, retired or in education (see Table 1).
Table 1 Characteristics of study sample
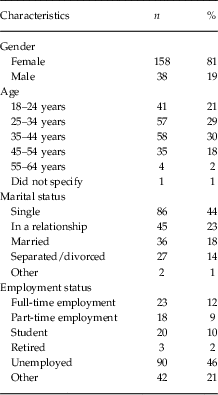
n=196. The study population includes individuals 18–64 years.
Cost analysis
Following Larg & Moss (Reference Larg and Moss2011) and Drummond et al. (Reference Drummond, Sculpher, Claxton, Stoddart and Torrance2015), a micro-costing approach employing standard methods was used to estimate the cost of treating BPD. Owing to the lack of national unit cost data/Ready Reckoner for community mental health services, a micro-costing approach was necessary. In undertaking the analysis, national guidelines for conducting cost analyses were adhered to (Health Information and Quality Authority, 2014). The resources used were identified and measured from the resource use questionnaire discussed above. The primary perspective taken was that of the health service provider and payer – the HSE, and included direct health care costs only. Three categories of direct health care costs were considered: acute care, community care and medication.
To value health resource use, a variety of methods were employed in line with national guidelines (Health Information and Quality Authority, 2014). Diagnostic-related group (DRG) estimates from the National Ready Reckoner were employed to estimate the costs of acute care (emergency department and acute hospitalisation) (Health Service Executive, 2013 a). In order to value the cost of ambulance transfers, an estimate from the literature was employed and adjusted for inflation (Gannon et al. Reference Gannon, O’Shea and Hudson2007).
Data on number and duration of visits to AMHS were provided in the resource use questionnaire. Using the hourly wage for each professional the value of community care services was estimated. Hourly wages were estimated using national guidelines (Health Information and Quality Authority, 2014), whereby the median value from the salary scales is adjusted for relevant costs including overheads. In the absence of evidence on professionals’ administration/ non-patient contact time associated with service delivery, it is assumed these are accounted for in the included overheads (25%).
With regards to valuing medications, the resource use questionnaire provided data on type and quantity of medications, used. To estimate cost of medications national guidelines were employed (National Centre for Pharmacoeconomics, 2016). The price to the wholesaler was extracted from the national medicine database (Primary Care Reimbursement Service, 2017); and the dispensing fee and rebate to the wholesaler were estimated.
The resource use questionnaire provided evidence on resource utilisation for a 6-month period. Assuming this 6 months reflected usual practice, it was directly extrapolated to 12 months to represent annual utilisation.
Sensitivity analysis
In this analysis, resource estimates are from a sample of data, thus the parameters are subject to uncertainty (Briggs et al. Reference Briggs, Sculpher and Claxton2006). To address this parameter uncertainty a probabilistic sensitivity analysis (PSA) was employed. This required characterising uncertainty in input parameters, propagating uncertainty through the model using a Monte Carlo simulation model and presenting the implications of parameter uncertainty on the cost estimates. Thus we can examine if uncertainty in the input parameters results in uncertainty surrounding the cost estimate. The latter is illustrated in the 95 percentile ranges presented.
One-way sensitivity analyses are also employed to estimate the burden of BPD to the Irish health service by varying prevalence rates. Prevalence rates of BPD in the population aged 18–65 [as advocated by Torgersen et al. (Reference Torgersen, Kringlen and Cramer2001)] were varied between 0.7% and 1%, in line with international literature (Torgersen et al. Reference Torgersen, Kringlen and Cramer2001; Jackson & Burgess, Reference Jackson and Burgess2004; Coid et al. Reference Cronin and Bourke2006).
Results
Direct health service costs
Acute health services utilised included emergency department attendance, ambulance transfer and inpatient admission. Analysis of the data revealed 45% of the sample visited the emergency department 2.3 times in a 6 monthly period on average. Applying the relevant costs, the average annual cost of emergency department visits is €717 per person with BPD. Approximately 18% of these visits included transfer by ambulance, at a cost of €81 per person with BPD. The data revealed that 37% of the sample population were admitted as an inpatient. Applying the relevant DRG tariff, this is valued at the annual average cost per person with BPD of €5497 for inpatient care (see Table 2).
Table 2 Average annual cost of borderline personality disorder per person in Ireland

a Results of probability sensitivity analysis. Beta distribution applied to probability of attending or using each services; gamma distribution applied to the frequency and duration of visits and normal distributions applied to costs.
b See Table 3 for further detail on adult mental health services.
All persons in the sample utilised AMHS at an annual average cost of €3282 per person with BPD. These services included psychiatrists, hospital physicians, nursing personnel, clinical psychologists, counsellors, therapists and social workers (see Table 3).
Table 3 Utilisation of adult mental health services by individuals with borderline personality disorder
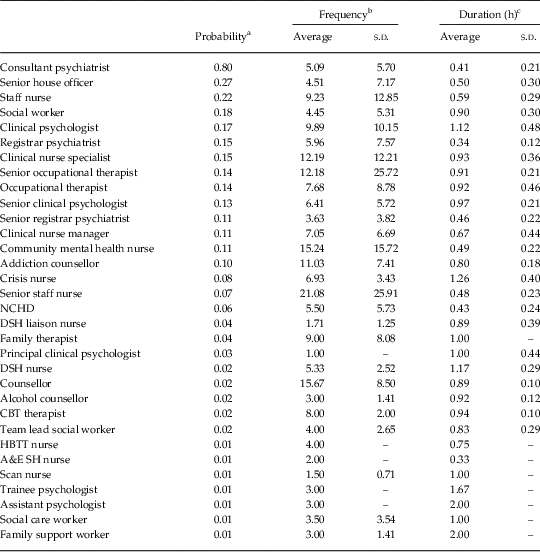
NCHD, non-consultant hospital doctor; DSH, deliberate self-harm; HBTT, home-based treatment team; A&E: accident and emergency; CBT, cognitive behavioural therapy; SH, self-harm.
a The probability of a client attending professional.
b The number of visits to that professional in a 6 monthly period per client
c The duration per visit, measured in hours per client.
The resource use questionnaire also included questions on type and dosage of medications. 82% of the sample population reported taking at least one medication. The annual average cost of medications per person with BPD was €1267. As many persons with BPD may have a means-tested medical card [permitting them access to medication for a €2.50 fee per item dispensed up to maximum of €25 at the time of the analysis (Health Service Executive, 2013b)], reimbursement for these medications would be included in HSE budgets, thus are included in the analysis.
The average total cost to the HSE when utilisation of acute health services, AMHS, other funded mental health services and medications are included is €10 844 per person per year. The breakdown of these costs reveals that admissions account for 51% of the total direct health care costs; mental health services 30% and medications 12%. Emergency department visits and ambulance transfers account for 8% collectively (Table 2).
Sensitivity analysis
Within the PSA, a Monte Carlo simulation was conducted around the total cost estimate to account for uncertainty. The sensitivity analysis results indicate a 95 percentile range for the average total costs of €5228 to €20 609 suggesting uncertainty in the input parameters translates to uncertainty surrounding the cost estimate (see Table 2).
Prevalence
Table 4 presents the estimated costs of providing health care for the BPD population using the previously discussed range of prevalence rates. With a 1% prevalence rate the annual cost of treating BPD in Ireland is €311.50 million in direct health care costs. Lowering the prevalence rate to 0.7% (one-way sensitivity analysis) decreases the estimated annual direct health care costs to €218.05 million. These COI estimates assume that all persons with BPD are utilising the mental health services. It is important to note that given the complexity of BPD, persons with the condition may not yet be diagnosed, while others with a diagnosis may not be engaging with the mental health services.
Table 4 Total costs (€ millions) of borderline personality disorder (BPD) in Ireland

a Irish adult population aged 18–65: 2.87 million.
Discussion
The aim of this study was to estimate the direct health care costs of BPD in Ireland. The results of the analysis reveal that the total direct health care cost to the HSE for providing care to a BPD patient is €10 844 annually. An examination of the breakdown of the total cost of care to the health care provider reveals that hospitalisations account for almost half (51%), and mental health services (AMHS) for almost a third (30%) of direct health care costs. The remainder of costs comprise emergency and ambulatory care (8%) and medication (12%).
It is important to emphasise again that the perspective of this study is quite narrow, in that only direct health care costs for persons with BPD in Ireland are addressed. For instance, other relevant costs such as those outside (mental) health care like productivity costs of the patients and of informal care are not considered in our analysis. Furthermore, it should also be noted that the overall COI estimates are calculated on the assumption that all individuals aged 18–65 with BPD are engaging with the health services. However, given the complexities of this condition it is likely that many individuals have yet to be diagnosed, some do not engage with services, while others may be attending primary care practitioners. This is no doubt a major limitation of this type of research, and suggests that the costs reported in this paper be treated with a degree of caution. In addition, data on resource use where participants engage with mental health services outside their primary service is not captured in this study, potentially underestimating BPD treatment costs. It is also important to acknowledge that it is not only people with a formal diagnosis of BPD that generate costs to the health system. A recent paper on prevalence rates of BPD symptoms reports that patients with subthreshold BPD are intensive users of health resources (ten Have et al. Reference ten Have, Verheul, Kaasenbrood, van Dorsselaer, Tuithof, Kleinjan and de Graaf2016). Furthermore, in extrapolating from 6 to 12 months to estimate annual resource utilisation, we do not account for seasonality or other factors, which may result in over or under estimating costs.
A strength of this study lies in the data collection methods. Rather than relying on self-reported resource utilisation from participants, data were extracted from participants’ clinical files by their lead treating clinician. It is unlikely that study participants would be able to reliably provide information retrospectively about resource utilisation given that individuals with a BPD diagnosis may have multiple service contacts in any 1 week (Zanarini et al. Reference Zanarini, Frankenburg, Khera and Bleichmar2001; Bender et al. Reference Bender, Skodol, Pagano, Dyck, Grilo, Shea, Sanislow, Zanarini, Yen, McGlashan and Gunderson2006), and the study period spans across a 6-month timeframe. Data in the clinical file is factual information based on each individual’s contact with mental health services (acute inpatient, outpatient and emergency department). As this study examines the cost of BPD only (excludes other unrelated resource use), the lead clinicians are best placed to accurately report on mental health services resource use in the absence of a national integrated health information system. This approach increases the reliability and verifiability of the data, which in turn improves the accuracy of the analysis.
In Ireland, there is a dearth of unit cost data. While hospital admissions are covered by case-mix, there is no accurate unit cost data for community mental health services. The absence of this data is a considerable constraint to research and decision-making in the area of community mental health services in Ireland. This paper contributes to the limited literature in Ireland on resource use and costs in community mental health services.
There can be considerable inconsistencies in the way in which COI studies are conducted. In addition, some studies are far from transparent in describing the data employed and reporting the analysis undertaken. These shortcomings limit the usefulness and comparability of COI studies. To overcome these limitations, we follow guidelines from Larg & Moss (Reference Larg and Moss2011) in reporting and evaluating COI studies. These guidelines provide a standardised appraisal tool which encourages greater transparency of reporting.
While there is an absence of COI studies of BPD in Ireland, previous COI studies for BPD across Europe reported average total costs ranging from €11 308 in Spain to €16 852 in the Netherlands (van Asselt et al. Reference van Asselt, Dirksen, Arntz and Severens2007; Soeteman et al. Reference Soeteman, van Roijen, Verheul and Busschbach2008; Salvador-Carulla et al. Reference Salvador-Carulla, Bendeck, Ferrer, Andion, Aragones and Casas2014). These studies also included non-health care costs, such as domestic help, addiction treatment, prison and sheltered employment, and indirect costs such as informal care, sick leave and out-of-pocket expenses. As discussed, our analysis focused on direct health care costs. Therefore, comparisons with these Dutch and Spanish studies in respect of direct health care costs only are more appropriate.
Practices for treating BPD vary across jurisdictions. For example, the analysis in the current study reveals that in an Irish setting, hospitalisations consume the most resources, which is similar to the Netherlands (van Asselt et al. Reference van Asselt, Dirksen, Arntz and Severens2007), whereas in Spain, spend on medications accounts for the majority of direct health care costs (Salvador-Carulla et al. Reference Salvador-Carulla, Bendeck, Ferrer, Andion, Aragones and Casas2014). The current study reveals that hospitalisation (51%) and medication (12%) account for 63% of direct health care spend in Ireland. General clinical recommendations for the treatment of BPD such as those advocated by the National Institute for Health and Care Excellence (2009) and the American Psychiatric Association (2005) advise that the primary treatment for BPD is psychotherapy, preferably in outpatient and day care settings, while hospitalisation and medication have a role in symptom management only (Oldham, Reference Oldham2005; National Institute for Health and Care Excellence, 2009; Departament de Salut Generalitat de Catalunya, 2011). The results of the current study, as well as those in other jurisdictions, indicate a high proportion of costs for hospitalisation and medication use. Country-specific COI studies for BPD are vital to determine how resources are currently being allocated and whether such resource allocations are in line with best practice treatments for BPD.
COI studies such as the current study can be employed to inform economic evaluations of specific treatments by providing nationally representative evidence on treatment as usual. This is of particular importance in the absence of standard randomised control trials, owing to lack of clinical equipoise between treatment-as-usual and evidence-based treatments. It is envisaged that our findings on the costs of treating BPD can be used alongside studies investigating the effectiveness of evidence-based treatments for BPD, such as DBT, schema therapy, mentalisation based therapy or transference focused psychotherapy (Departament de Salut Generalitat de Catalunya, 2011; Stoffers et al. Reference Stoffers, Vollm, Rucker, Timmer, Huband and Lieb2012). DBT is the recommended evidence-based treatment for persons with BPD (Government of Ireland, 2006), and is currently being implemented in Ireland through the National DBT Project (Flynn et al. 2018Reference Flynn, Kells, Joyce, Suarez and Gillespieb). Furthermore, these future studies can then inform the development of national guidelines that promote effective and cost-effective treatments for BPD, and inform budgeting and resource allocation decisions. This can present policy-makers with considerable challenges, particularly when health budgets are allocated between acute hospital services, medications and non-acute services etc., as is the case in Ireland.Footnote 2 This necessitates budget adjustments so as to transfer the savings from acute services and medication budgets to fund the investment required to deliver interventions such as those recommended in mental health services.
Acknowledgements
The authors thank the clinicians who extracted the data at each of the study sites, without whom this research would not have been possible.
Financial Support
This research was supported by the National Office for Suicide Prevention, Health Service Executive, Ireland.
Conflicts of Interest
The authors declare that there are no conflicts of interest to disclose.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. Ethical approval to carry out this research was received from the following research ethics committees: Cork Research Ethics Committee of the Cork University Teaching Hospitals, Galway Clinical Research Ethics Committee, HSE North East Area Research Ethics Committee, HSE South East Area Research Ethics Committee, Naas General Hospital Ethics Committee and Sligo General Hospital Research Ethics Committee. All participants were provided with detailed information about the research study and data confidentiality. Participation in the study was voluntary and could be withdrawn at any time. All participants signed written informed consent forms as outlined in the study protocol.






