No CrossRef data available.
Article contents
P122: Differences of the treatment needs of patients with dementia with Lewy bodies and their caregivers with duration after diagnosis
Published online by Cambridge University Press: 02 February 2024
Abstract
We have reported parkinsonism and psychiatric symptoms were the most important treatment needs of patients with dementia with Lewy bodies (DLB) and their caregivers, respectively 1). However, the frequency presenting clinical symptoms and the onset time vary among patients. We investigated the impact of the disease duration on clinical symptoms, prescribed medication and treatment needs of patients and their caregivers.
Disease duration was defined as time after diagnosis with DLB. Patient-caregiver pairs were classified into two groups; one with a disease duration <24 months (S-group) and the other with a disease duration ≥24 months (L-group). Comparisons were made between two groups regarding background characteristics and treatment needs of patients and caregivers. Treatment needs were defined as symptom domains most distressing to patients and caregivers.
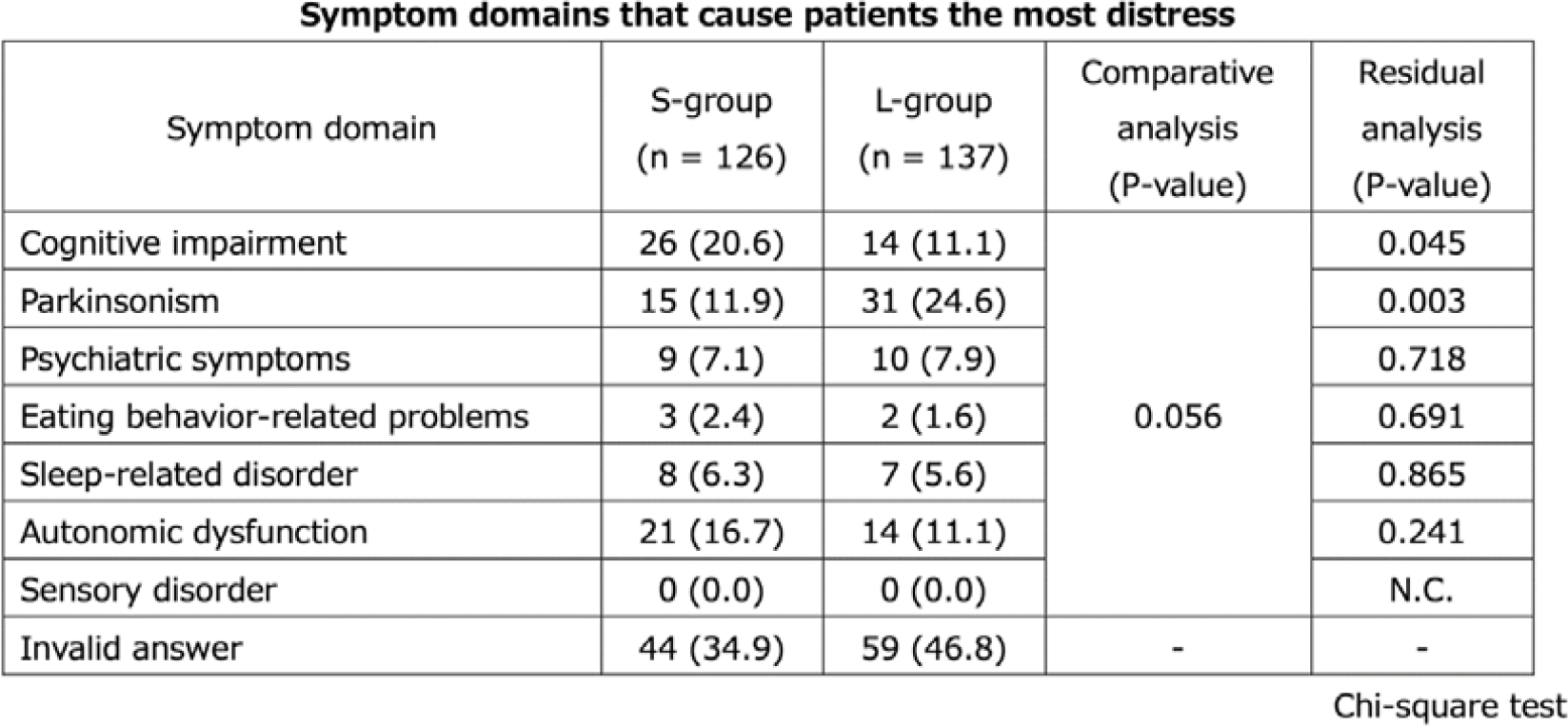
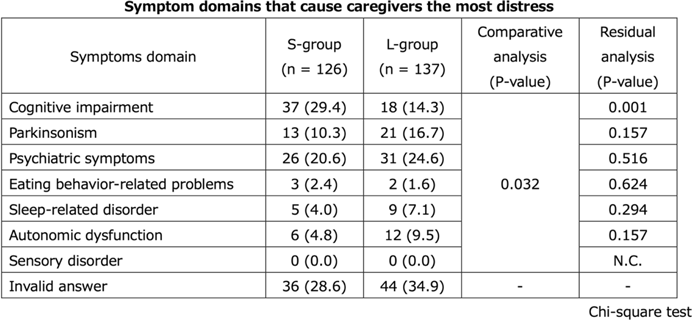
S-group and L-group were consisted of 126 and 137 pairs of patients and their caregivers, respectively. Regarding patientsʼ current symptoms, parkinsonism and autonomic dysfunction were significantly higher in L-group than S-group. MDS-UPDRS Part III total score and the frequency of prescription for memantine and antiparkinsonian were also significantly higher in L-group than in S- group. The treatment needs most frequently selected by patients was cognitive impairment (20.6%) followed by autonomic dysfunction (16.7%) and parkinsonism (11.9%) in S-group, and parkinsonism (24.6%), followed by cognitive impairment and autonomic dysfunction (11.1% each) in L-group, suggesting no significant difference in the tendency of symptom domains to desire treatment between groups (P=0.056). However, residual analysis showed that patients in S-group were more likely to select cognitive impairment than in L-group (P=0.045), and those in L-group were more likely to select parkinsonism than in S-group (P=0.003). The treatment needs most frequently selected by caregivers in S-group was cognitive impairment (29.4%) followed by psychiatric symptoms (20.6%) and parkinsonism (10.3%) in S-group, and psychiatric symptoms (24.6%), followed by parkinsonism (16.7%) and cognitive impairment (14.3%) in L-group, suggesting significant difference in the tendency of patientsʼ symptom domains to desire treatment between groups (P=0.032). Dara from the onset will be added at the poster presentation.
It was suggested that the treatment needs of patients and their caregivers might change with duration after diagnosis.
- Type
- Posters
- Information
- Copyright
- © International Psychogeriatric Association 2024


