No CrossRef data available.
Published online by Cambridge University Press: 02 February 2024
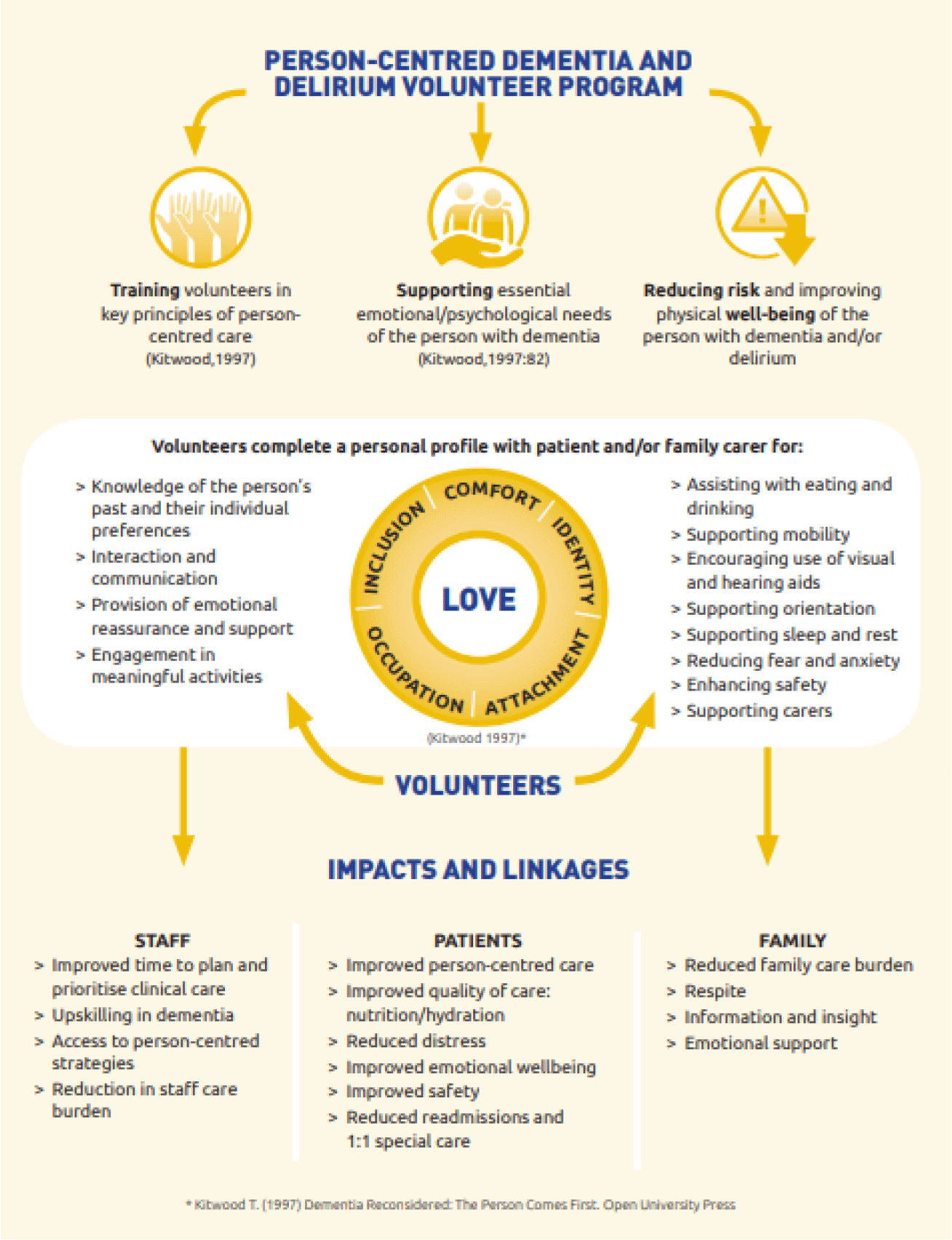
evaluate the clinical outcomes for acute hospital patients with dementia, delirium or at risk for delirium supported by the person-centred volunteer program in australian rural hospitals.
a non-randomised, mixed methods, controlled trial.
older adults admitted to 7 rural acute hospitals. Intervention (n=270) patients were >65 years with a diagnosis of dementia and/or delirium or had risk factors for delirium and received volunteer services. Family carers (n=83) of intervention patients were interviewed. Staff survey and focus groups. Control (n=188) patients were randomly drawn from patients admitted to the same hospital 12 months prior to the volunteer program who would have met program eligibility criteria.
trained volunteers provided 1:1 person centred care with a focus on nutrition and hydration support, hearing and visual aids, activities, and orientation.
medical record audits provided data on volunteer visits, diagnoses, length of stay (los), behavioural incidents, readmission, specialling, mortality, admission to residential care, falls, pressure ulcers and medication use.
across all sites there was a significant reduction in rates of 1:1 specialling (p=.011) and 28 day readmission (p=.006) for patients receiving the volunteer intervention. Los was significantly shorter for the control group (p=.001). All other patient outcomes were equivalent for the intervention and control group (p>.05). Volunteers integrated themselves into the care team providing person-centred care, increased safety and quality of care and were an “extra pair of hands”, reducing care burden for staff and importantly for families: “for me, knowing someone was there … i can't even tell you what a benefit that was”. 98% of staff rated the program as supportive of them in their care
Enablers were clear processes for screening, training and supporting volunteers. Key challenges included initial role delineation, staff/volunteer trust and sustainability.
appropriately trained and supported volunteers are cost effective and can improve the safety and quality of care for hospitalised patients with cognitive impairment in rural hospitals.