Introduction
The World Health Organization (WHO, 2019) calculates that one person dies by suicide approximately every 40 seconds worldwide, with those in older age groups (i.e. over 65 years) being at highest risk. Globally, older men are twice as likely to die by suicide compared to women in the same age groups (Barak et al, Reference Barak, Cheung, Fortune and Glue2020; Canetto, Reference Canetto2017). Suicide ideation (thoughts, desires, or plans surrounding ending one’s own life) is a recognized risk factor in suicidal behavior (Nock et al., Reference Nock2008) and increases the risk of suicide attempts in older adults (Pfaff and Almeida, Reference Pfaff and Almeida2005).
Research suggests that there may be unique factors that contribute to thoughts of suicide in older adults including social isolation, childhood trauma, financial distress, and multiple medical morbidities that are not routinely investigated (Almeida et al., Reference Almeida2012; De Leo et al., Reference De Leo, Draper, Snowden and Kolves2013). Evidence suggests that deaths in older people that result from more “passive” acts (e.g. voluntary stopping of eating and drinking, suspending/refusing medication) are unlikely to be formally investigated as potential suicide deaths and that official statistics therefore under-estimate the prevalence of suicide in those over 65 (Deuter et al., Reference Deuter, Proctor, Evans and Jaworski2016; Hafford-Letchfield et al., Reference Hafford-Letchfield2018; Lachman, Reference Lachman2015). A key feature in preventing suicide among older adults is to accurately and routinely screen for suicide ideation. However, this is not currently the norm in healthcare settings (De Leo et al., Reference De Leo, Draper, Snowden and Kolves2013).
Suicide and older adults
Joiner’s (Reference Joiner2005) interpersonal theory of suicide posits that people consider suicide when they feel that they are a burden to family and/or society, and when they no longer feel they belong to valued relationships or wider groups. Suicide in later life is often considered to be the result of a “rational decision” and can be interpreted as a legitimate exit in the case of dramatic changes in social status and role (Bernier et al., Reference Bernier, Lapierre and Desjardins2020). Structural ageism and internalized stigma can contribute towards the view that depression is a normal feature of the aging process and the antecedent of an anticipated and definitive ending (Gleeson et al, Reference Gleeson, Hafford-Letchfield, Quaife, Collins and Flynn2018; Stanley et al, Reference Stanley, Hom, Rogers, Hagan and Joiner2016). Compared to younger age groups, suicide behavior is also more likely to result in death in older people (Monforte-Royo et al, Reference Monforte-Royo, Villavicencio-Chávez, Tomás-Sábado and Balaguer2011; Wand et al, Reference Wand, Peisah, Draper and Brodaty2017).
Psychological autopsy reports have shown that a high proportion (46–86%) of reported suicides in older people were correlated with symptoms of depression in the weeks prior to death (Conwell et al., Reference Conwell, Van Orden and Caine2011). A clinical diagnosis of depression or anxiety disorder was also found to be associated with a seven-fold increased risk of reporting suicide ideation compared to those without a diagnosis for over 65-year-olds (Almeida et al., Reference Almeida2012). It has been argued, however, that symptoms of depression among older people differ from those of younger adults and that there is a need for more age-specific screening and diagnostic measures (Conejero et al., Reference Conejero, Olie, Courtet and Calati2018; Gleeson et al., Reference Gleeson, Hafford-Letchfield, Quaife, Collins and Flynn2018). Interventions aimed at identifying and reducing depression among older populations appear to have little long-term impact on mental health (Almeida et al., Reference Almeida2012; Gleeson et al., Reference Gleeson, Hafford-Letchfield, Quaife, Collins and Flynn2018). History of suicide behavior is recognized as a key indicator of taking one’s life in older populations (O’Riley et al., Reference O’Riley, Van Orden, He, Richardson, Podgorski and Conwell2014); however, such a history may not be present and their choice of means of suicide are more likely to be lethal in the first instance when compared to younger populations (WHO, 2019).
Cukrowicz et al. (Reference Cukrowicz, Cheavens, van Orden, Ragain and Cook2011) distinguished between suicide ideation and death ideation in older adults, which they described as a passive wish to die. Their study tested theory-based risk models of suicide including death ideation, depressive symptoms, thwarted belongingness, and perceived burdensomeness. Their findings suggest that perceived burdensomeness contributes unique variance to suicide ideation in older adults, comparable to that found in other studies with people with terminal illnesses. Feelings of being a burden to others and subsequent perceptions that death is a viable way to avoid this were also found to be present in other studies with older adults expressing passive suicide ideation and their carers (e.g. Hafford-Letchfield et al., Reference Hafford-Letchfield2018).
Screening for suicide ideation in older adults
Given the established links between depression and suicide across age groups, the most common approach to preventing suicide in older age groups to date has concentrated on measuring signs of depression (Gleeson et al., Reference Gleeson, Hafford-Letchfield, Quaife, Collins and Flynn2018). However, screening for depression in older people is not routine across settings (Gleeson et al., Reference Gleeson, Hafford-Letchfield, Quaife, Collins and Flynn2018) and numerous studies have highlighted a reluctance to speak openly about mental health among this generation (e.g. Hafford-Letchfield et al., Reference Hafford-Letchfield2018). In contrast, other research has suggested there is a preference for talking therapies among older people, but in the UK at least, access to these interventions remains low in this group (Frost et al., Reference Frost, Beattie, Bhanu, Walters and Ben-Schlomo2018). In practice, it has been reported that those over 85 years are up to a third more likely to be prescribed anti-depressants compared to those between 55 and 85 years (Frost et al., Reference Frost, Beattie, Bhanu, Walters and Ben-Schlomo2018).
However, it appears that a majority of older people who die by suicide have visited a GP in the previous 30 days (Neufeld and O’Rourke, Reference Neufeld and O’Rourke2009). The most common ailments discussed at these visits are somatic in nature rather than related to mental health. While it is recognized by GPs that older people may present with somatic symptoms that mask psychological difficulties, they may feel that the time and sensitivity needed to properly uncover and respond to these issues is not available to them (Frost et al., Reference Frost, Beattie, Bhanu, Walters and Ben-Schlomo2018). In addition, the normalization of older people’s poor mental health as a factor of aging can lead to Health Care Professionals (HCPs) believing that therapeutic interventions are likely to be ineffective and therefore were less likely to be offered.
Accurate detection of suicide ideation among older adults is of particular relevance in light of arguments that death by suicide is likely to be under-reported in those over 65 (Deuter et al., Reference Deuter, Proctor, Evans and Jaworski2016). The potential for unique presentation of depression or other mental health difficulties related to suicide ideation, the seeming reluctance to discuss psychological or emotional distress with healthcare professionals, and the possibility that poor mental health is a “normal” part of aging all may contribute to many older people failing to receive the support and preventative measures needed to reduce suicide. Currently, there is little consensus as to how to screen for suicide ideation in older people. It is likely that healthcare professionals either lack training in mental health problems in this population or are unaware of the need to assess the potential for suicide behavior in older people. The literature suggests a need for a common, easy to use, and acceptable means of accurately screening older people for both active and passive suicide ideation that can inform improved mental healthcare provision for this group.
To our knowledge, no comprehensive psychometric review of measurements of suicide ideation designed specifically for older adults has been conducted. Given the strong theoretical arguments that older adults may display unique, nuanced indicators of suicide ideation, it is important to consider the usefulness and efficacy of measures aimed at this population to better understand how to uncover, and respond, to suicide ideation in older adults. We conducted a systematic review of existing measures of suicide ideation designed for use with older adults to address the following aims:
-
1. Identify current measures of suicide ideation in older populations and to explore the extent and effectiveness of their use
-
2. Evaluate the psychometric properties of these measures and identify strengths and weaknesses in current provision to effectively measure suicide ideation in this population
Methods
Search strategy
HG and CR conducted searches in 12 databases (APA PsycTests; CareKnowledge; CINAHL; Cochrane; Emerald; IBSS; Medline; NICE evidence; OVID; PsycInfo; Social Care Online; Web of Science) using a combination of keywords based on the PICO system (searches conducted between June and August 2020).
Population: older; aged; geriatric; care home resident*; elderly; old; old age
Intervention: measure; questionnaire; survey; instrument; scale
Setting: care home; residential care; community; hospital; institutional care
Outcome: depression; suicide; suicidal thoughts; suicide thoughts; suicid* ideation; suicid* behavior; mental health; wish to die; well-being
Inclusion/exclusion criteria
Peer-reviewed journal articles were included if they reported on the development, testing, or validation of a measurement instrument designed to assess suicide ideation in older populations only. We excluded those articles that reported on scales intended to measure broader mental health-related factors but that may have included a single item to assess suicide ideation (e.g. Geriatric Depression Scale). We included articles that had been assessed with non-English speaking populations if the article was published in the English language. Studies were included irrespective of where the sample was drawn from to validate a measure (e.g. psychiatric inpatient, community, residential care, etc.). The term “older people” was defined as those 50 years and over to allow for the broadest range of studies to be included.
Data extraction and quality assessment
The initial database search yielded 123 papers with one duplicate. Titles were screened by two authors (HG and CR) for relevance with a remaining 46 included for second screening. Abstracts were read by at least two authors for a final decision on inclusion, leaving a total of ten articles, reporting on seven different scales, for review. Reference lists of each of these articles were also screened for any additional relevant articles to include, but did not yield any additional papers for inclusion. No disagreements on inclusion/exclusion occurred between the authors of this paper. This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA; Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009). The PRISMA diagram can be found in Figure 1.

Figure 1 PRISMA diagram of screening process
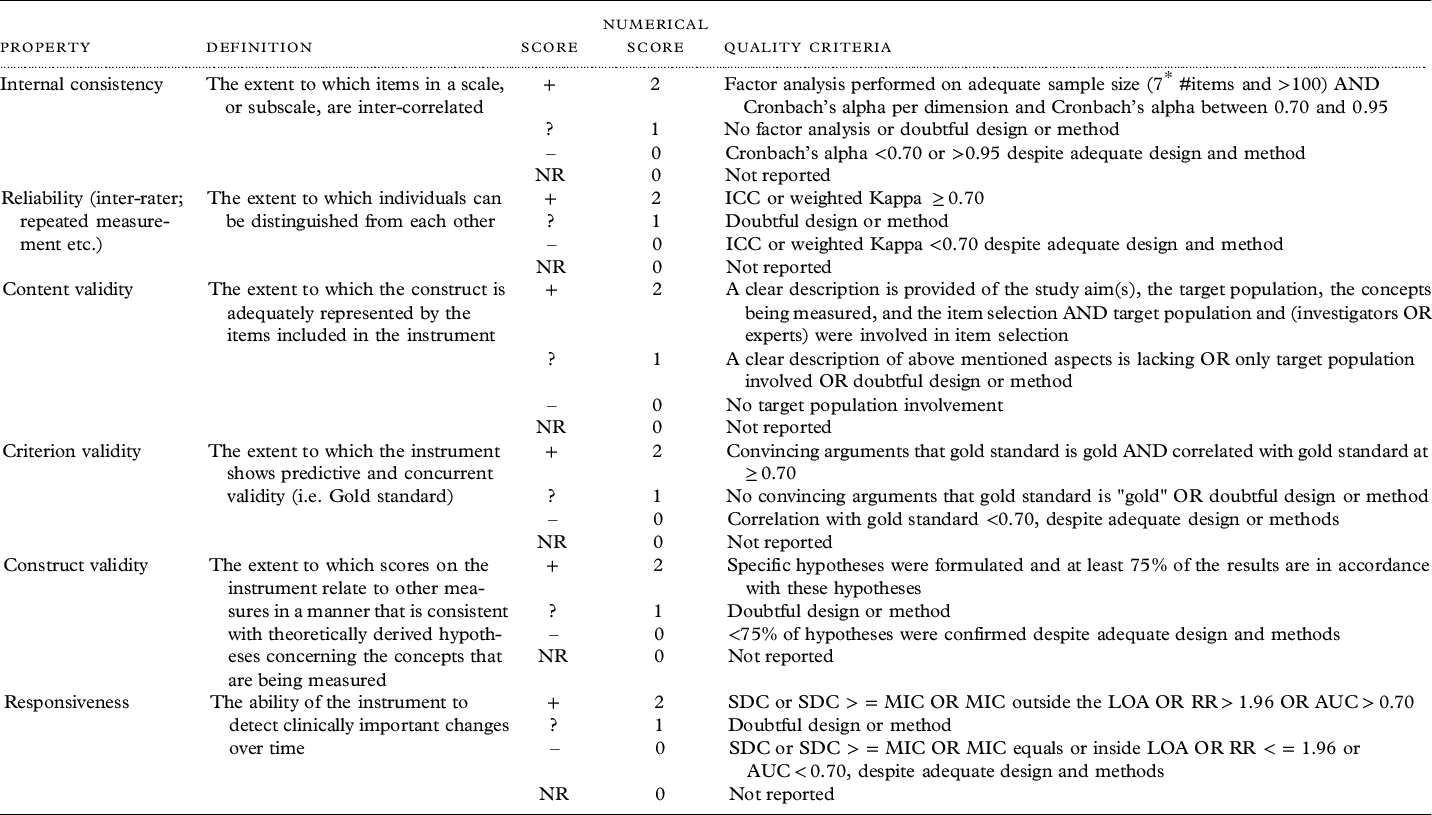
The COSMIN framework was used to evaluate the included studies for quality of psychometric reporting, with scoring included as recommended by Terwee et al. (Reference Terwee, Mokkink, Knol, Ostelo, Bouter and de Vet2012), Table 2 details the quality assessment criteria applied in this study.
Results
General results
The main details of each of the articles reviewed, with abbreviations used throughout the results, are outlined in Table 1.
Table 1. Description of articles included in review

This paper included details of the scale item construction; the table includes only the results from the psychometric analysis part of the study
Table 2. Quality assessment criteria and details
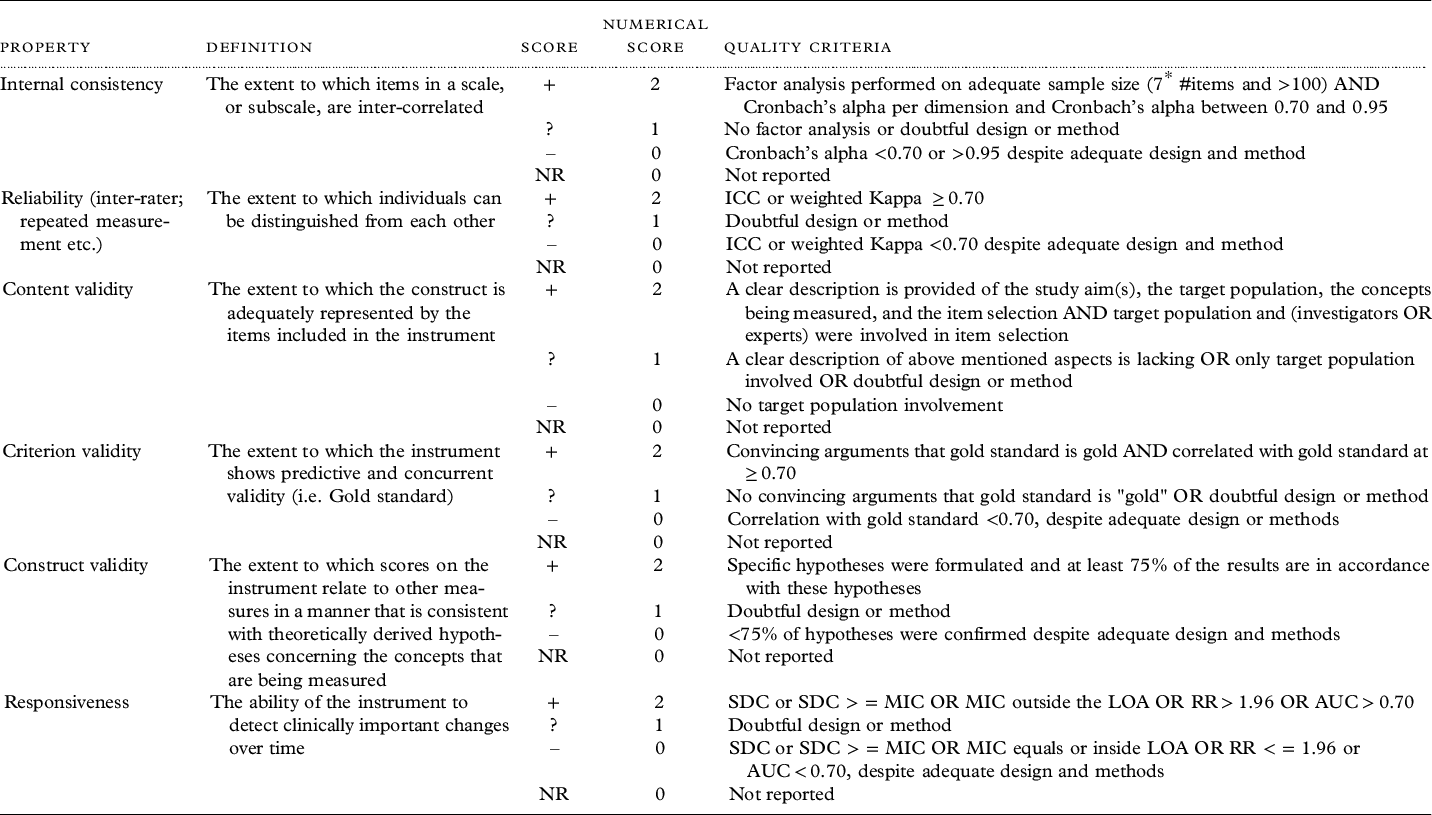
In order to calculate a total score + = 2 positive rating; ? = 1 indeterminate rating; – = 0 negative rating; 0 = no information available
Total score range 0–12
* Item selection criterion only applied to original scale development studies
**Cronbach’s alpha calculated per dimension if the impostor phenomenon is conceptualized as multidimensional in the specific study
AUC, area under the curve; MIC, Minimal important change (this is the smallest difference in score in the domain of interest which patients perceive as beneficial and would agree to, in the absence of side effects and excessive cost)s; RR, responsiveness ratio; SDC, Smallest detectable difference (this is the smallest within person change, above measurement error. A positive rating is given when the SDC or the limits of agreement are smaller than the MIC); SEM, standard error of measurement
We identified seven individual scales across the ten articles included for review that were a mixture of those measuring negative (wish/will to die) factors and those focusing on reasons, or wishes, to live. The measures included the Reasons for Living scale-Older Adults (RFL-OA), reported on by three of the articles included for review: an adaption by Edelstein et al. (Reference Edelstein2009) for older adults, a shortened version developed by Lutz et al., (Reference Lutz, Edelstein, Katz and Gallegos2019), and one article examining the resiliency to suicide subscale individually (Wadhwa and Heisel, Reference Wadhwa and Heisel2019). The psychometric properties of Geriatric Suicide Ideation Scale (GSIS) (which was originally developed by Heisel and Flett in 2006) were reported by two articles included in this review (Heisel and Flett, Reference Heisel and Flett2016; O’Rourke et al., Reference O’Rourke2018). One article reported on the use of the 5-item World Health Organization Well-being scale as a measure of suicide ideation in older people (Awata et al., Reference Awata2007), while three articles were single psychometric reports on a novel scale developed by the authors: Will to Live (Carmel, Reference Carmel2017); Triggers of Suicidal Ideation Inventory (TSII; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017); and the Ultra-Short Suicidal Ideation Inventory (USSII; Nugent and Cummings, Reference Nugent and Cummings2014). The final article reported on the combined use of existing scales, adapted for older adults: the Categories of Attitude Toward Death Occurrence (CADO) and the Schedule of Attitudes Toward Hastened Death – Senior (SAHD) scales (Durst et al., Reference Durst2020).
The included articles represent a range of countries with three from the USA (Edelstein et al., Reference Edelstein2009; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019; Nugent and Cummings, Reference Nugent and Cummings2014), two from Canada (Heisel and Flett, Reference Heisel and Flett2016; Wadhwa and Heisel, Reference Wadhwa and Heisel2019), and one each from Japan (Awata et al., Reference Awata2007), Taiwan (Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017), Israel (Carmel, Reference Carmel2017), and Switzerland (Durst et al., Reference Durst2020), with one further article using social media to recruit an international sample (O’Rourke et al., Reference O’Rourke2018). Measurement development and validation across the different scales were conducted with community, out-patient, and clinical samples ranging in age from 50 to 99 years. Most samples were over-represented by female participants (up to three quarters in some), and all studies that included information on the ethnicity of the sample were predominantly White, apart from studies conducted with Japanese (Awata et al., Reference Awata2007) and Taiwanese (Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017) samples. We consider the measures in light of these sampling limitations in the Discussion.
Administration and sampling
Six of the articles reviewed were based on self-reported measures (Durst et al., Reference Durst2020; Edelstein et al., Reference Edelstein2009; Heisel and Flett, Reference Heisel and Flett2016; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019; O’Rourke et al., Reference O’Rourke2018; Wadhwa and Heisel, Reference Wadhwa and Heisel2019), three used clinician interviews and interpretation to administer the measure and score responses (Awata et al., Reference Awata2007; Carmel, Reference Carmel2017; Nugent and Cummings, Reference Nugent and Cummings2014), while administration was not reported for the TSII (Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017).
A number stated the purpose of their measures were to aid clinical detection of suicide ideation or assess risk factors for suicide in older adults, while some were presented as screening tools that could be used in more general assessment of well-being, referral decisions or support needs. However, the rationale for using exclusively community samples (Awata et al., Reference Awata2007; Carmel, Reference Carmel2017; Heisel and Flett, Reference Heisel and Flett2016; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019; O’Rourke et al., 2017), mental health patient (either inpatient or outpatient) clinical samples (Durst et al., Reference Durst2020; Edelstein et al., Reference Edelstein2009; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017; Nugent and Cummings, Reference Nugent and Cummings2014), or a combination of both (Wadhwa and Heisel, Reference Wadhwa and Heisel2019) in order to pilot and psychometrically test their measures was not presented in these articles.
Scale development and design
Item generation varied across articles. The will-to-live scale (Carmel, Reference Carmel2017) developed scale items through a series of earlier interviews with 25 older people and Edelstein et al., (Reference Edelstein2009) generated additional items for the RFL-OA scale using open-ended questions to older people on the things they felt influenced their wish to continue living. Awata et al., (Reference Awata2007) used an established scale, the WHO Well-being Index, to assess its usefulness in measuring suicide ideation among older adults. Durst et al., (Reference Durst2020) adapted two scales (CADO and SAHD) to measure the presence and intensity of suicide ideation in their sample. Meanwhile, Lutz et al., (Reference Lutz, Edelstein, Katz and Gallegos2019) re-examined data from previous research and performed exploratory factor analyses to create a shortened version of the RFL scale before testing it psychometrically with a community sample recruited online. The remaining scales (Heisel and Flett, Reference Heisel and Flett2016; Nugent and Cummings, Reference Nugent and Cummings2014; O’Rourke et al., Reference O’Rourke2018; Wadhwa and Heisel, Reference Wadhwa and Heisel2019) were developed through a combination of reviews of existing literature and theory, clinical experience of the authors and, in the case of the TSII (Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017), the use of a Delphi panel.
Theoretical frameworks
Little information was provided in the papers reviewed on the process of item generation for scales reported. To better understand the approaches taken by the authors with respect to item generation, we assessed the theoretical frameworks adopted/used in each paper.
Three scales (RFL; Will to Live and WHO-5 Well-being) were developed from the perspective of measuring factors that act as protective against suicide ideation or behavior, tending to reflect the concept of resiliency. Theoretically, it was argued that older adults can be less inclined to speak to healthcare professionals about their mental health and may be reluctant to speak about negative emotions or experiences. Focusing on the factors that give them a reason to continue living (and by implication reasons for not attempting suicide) is thought to be a more appropriate means of detecting suicide risk in this population.
The older adult version of the RFL was adapted by Edelstein et al. (Reference Edelstein2009) to be administered to those aged over 60 years.. A community sample of older people who had previously considered suicide was asked to list the reasons that prevented them from attempting to take their own lives. This generated 41 unique items that had not previously been included in the RFL scale (for younger populations) and tended towards more reasons related to family, religion, and moral objections to suicide when compared to earlier versions.
Two further adaptations of the scale have been made, one as a shortened 30-item version (Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019) and another using just items that reflected resiliency to suicide from the scale resulting in a nine-item measure (Wadhwa and Heisel, Reference Wadhwa and Heisel2019). At 69 items, the original scale is argued to be excessively lengthy to be used with any frequency in most clinical settings (Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019) and shortened versions that can measure suicide ideation with comparable accuracy should increase the use of screening tools.
The will-to-live scale, developed by Carmel (Reference Carmel2017), is a five-item scale designed to measure subjective well-being among older adults using direct questions. Carmel argues that while subjective well-being scales can indicate positive factors in a person’s life, they do not accurately assess risk of suicide or suicide ideation and that there is a preference among older people to be asked directly about their will to live. There are positive associations, but also unique variance, between subjective well-being measures and the will-to-live scale developed and presented in this article.
The WHO-5 aims to measure the presence of depression, physical health burden, and perceived social support. Awata et al. (Reference Awata2007) argue that these are the main drivers of suicide ideation in older adults and present findings from a Japanese translation of the scale in their paper
The remaining four scales (GSIS; SAHD/CADO; TSII; USSIS) intended to measure suicide ideation more directly by focusing on the extent of thoughts of suicide or wishes to die that included both active and passive ideation (see Table 1 for full titles of all scales abbreviated here).
Developed by Heisel and Flett (2006), the GSIS is a 31-item scale designed to detect the unique factors associated with suicide ideation in older populations. Four subscales are included in the measure: suicide ideation, death ideation, loss of personal and social worth and, perceived meaning in life. The authors note that while past suicidal behavior is usually a significant predictive factor in determining future suicide risk, this is not always relevant in the context of older adults who are more likely to use lethal means on a first suicide attempt compared to younger populations. The purpose of the GSIS therefore is to detect more distal factors that may contribute to suicide ideation in older adults.
O’Rourke and colleagues assessed the GSIS in detecting suicide ideation in older adults with diagnosed bipolar disorder (BPD). This group was chosen because of the known increased risk of suicidal behavior in adults with BPD – particularly in those who have lived with a diagnosis for a longer period of time. Using social media to recruit 220 participants this study found that the four subscales of the GSIS reliably measured suicide ideation among this population.
Durst et al. (Reference Durst2020) adapted two scales (SAHD and CADO) designed to measure passive and active wish to die in older populations. Based on a scale initially developed to measure the wish to die among patients with terminal illness, the authors adapted the SAHD for older adults, who are more likely to endorse passive suicide ideation alongside previously measured factors. The CADO offers a qualitative assessment of the strength of the wish to die in older people who score highly on the SAHD which assists in clinical decision making relating to prevention and intervention services.
The Triggers of Suicide Ideation Inventory (TSII) was developed as part of a large-scale, longitudinal, suicide prevention study for older people in Taiwan (Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017). This ten-item scale contains three subscales: emotional distress; child-related and financial problems; and self-value-related concerns. Developed for use in primary care settings, the TSII was designed as a means of screening early signs of suicide ideation in older people to promote early intervention and/or prevention measures being offered.
The Ultra-Short Suicide Ideation Scale (USSIS) is a four-item scale designed for use by a range of professionals who work with older people to screen for potential suicide ideation (Nugent and Cummings, Reference Nugent and Cummings2014). The intention behind the development of this scale was to create an easy-to-use screening tool that was short enough not to place undue burden on healthcare professionals in order to increase suicide ideation screening in older populations. Development of this scale was consistent with the argument made by Carmel (Reference Carmel2017) in that older people have a preference for direct questions relating to their potential suicide ideation.
Psychometric properties
Full details of the psychometric properties, and where they rank in our quality assessment, are given in Tables 2 (criteria) and 3 (quality assessment scores). Overall, the scales demonstrated good levels of internal consistency through calculation of Cronbach’s alpha. Additional measures of reliability (repeated measures, Kappa, ICC, etc.) were only reported for one scale (TSII; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017) where high indicators of test-retest reliability were reported for follow-up data collection with 30 randomly selected participants.
Most of the scales reviewed scored low on the content validity score in our quality assessment criteria. This was largely due to a lack of involvement of older people in identifying items for the scales or in adaptations of existing scales. While most scales had expert involvement in item development, only the original RFL (Edelstein et al., Reference Edelstein2009) and the Will to Live (Carmel, Reference Carmel2017) tested the appropriateness of scale items with a pilot sample of older people. All other scales were developed through literature review or expert opinion without additional input from older adults.
Criterion validity was assessed as meeting the highest quality assessment score in all but two articles reviewed (WHO-5; Awata et al., Reference Awata2007; TSII; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017). These articles failed to assess validity of their scales against a standardized “gold standard” measure of suicide ideation either for older people or a wider population sample (as per the quality assessment tool, see Table 2). The other scales were compared to a range of additional measures including a series of subjective well-being measures (Will to Live; Carmel, Reference Carmel2017; GSIS; O’Rourke et al., Reference O’Rourke2018), the WHO quality of life index (SAHD/CADO; Durst et al., 2019), measures of previous suicide behavior (RFL; Edelstein et al., Reference Edelstein2009; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019; Wadhwa and Heisel, Reference Wadhwa and Heisel2019; GSIS; Heisel and Flett, Reference Heisel and Flett2016; O’Rourke et al., Reference O’Rourke2018), and clinician-rated suicide ideation after patient interview (USSII; Nugent and Cummings, Reference Nugent and Cummings2014).
Quality assessment scores for construct validity were variable across the seven scales. Both the RFL-OA (Edelstein et al., Reference Edelstein2009) and GSIS (in Bipolar Disorder) (O’Rourke et al., Reference O’Rourke2018) scales were assessed as high on construct validity in terms of both discriminant and convergent validity measurements. Psychometric statistics for construct validity were not reported for either the will-to-live scale (Carmel, Reference Carmel2017) or the TSII (Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017). All other articles reported some results but did not generate specific hypotheses or it was unclear if the hypotheses stated for individual scale development studies were fully met (i.e. >75%).
Suicide ideation was assessed using the Beck SSI (Edelstein et al., Reference Edelstein2009; Heisel and Flett, Reference Heisel and Flett2016; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017; Wadhwa and Heisel, Reference Wadhwa and Heisel2019), or clinician-rated psychological interview (Nugent and Cummings, Reference Nugent and Cummings2014). Lutz et al. (Reference Lutz, Edelstein, Katz and Gallegos2019) also compared scores on the RFL-OA shortened version to the GSIS to assess construct validity for suicide ideation, as did O’Rourke et al. (Reference O’Rourke2018) in their validation of the GSIS for older adults with Bipolar Disorder and Wadhwa and Heisel (Reference Wadhwa and Heisel2019) in validating the resiliency subscale of the RFL-OA. Past history of suicidal behavior was also measured in three of the included studies with single- or two-item scales (Edelstein et al., Reference Edelstein2009; Heisel and Flett, Reference Heisel and Flett2016) or in the case of the USSIS (Nugent and Cummings, Reference Nugent and Cummings2014) through clinician interview.
Depression was measured against the CESD Depression scale (Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019), Beck Depression Inventory (Edelstein et al., Reference Edelstein2009), or the Geriatric Depression Scale (Awata et al., Reference Awata2007; Carmel, Reference Carmel2017; Durst et al., Reference Durst2020; Heisel and Flett, Reference Heisel and Flett2016; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017; Nugent and Cummings, Reference Nugent and Cummings2014; Wadhwa and Heisel, Reference Wadhwa and Heisel2019). While some assessed their scales against psychological well-being (Heisel and Flett, Reference Heisel and Flett2016; Wadwha and Heisel, Reference Wadhwa and Heisel2019) and/or subjective well-being (Carmel, Reference Carmel2017; Durst et al., Reference Durst2020; Heisel and Flett, Reference Heisel and Flett2016; Wadhwa and Heisel, Reference Wadhwa and Heisel2019) or satisfaction with life (O’Rourke et al., Reference O’Rourke2018).
Additional comparative measures included measures of physical functioning (Awata et al., Reference Awata2007; Edelstein et al., Reference Edelstein2009; Heisel and Flett, Reference Heisel and Flett2016; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019), general physical health (Carmel, Reference Carmel2017; Heisel and Flett, Reference Heisel and Flett2016; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019; O’Rourke et al., Reference O’Rourke2018; Wadhwa and Heisel, Reference Wadhwa and Heisel2019), hopelessness (Heisel and Flett, Reference Heisel and Flett2016; Lutz et al., Reference Lutz, Edelstein, Katz and Gallegos2019; Wadhwa and Heisel, Reference Wadhwa and Heisel2019), and loneliness (Carmel, Reference Carmel2017; Heisel and Flett, Reference Heisel and Flett2016; Lee et al., Reference Lee, Tsai, Wang, Chen and Tsai2017).
O’Rourke et al., (Reference O’Rourke2018) also assessed the psychometric properties of the GSIS (in Bipolar Disorder) against theoretically significant related factors for individuals with BPD who have a history of suicide behavior, including measures of medication adherence, sleep problems, and alcohol use.
Discussion
Globally, older people are at increased risk of dying by suicide when compared to other age groups (WHO, 2019). This is largely due to the use of more lethal methods and a tendency to either not seek, or not be offered, therapeutic intervention for mental health difficulties (Frost et al., Reference Frost, Beattie, Bhanu, Walters and Ben-Schlomo2018). A majority of older people who die by suicide have had a recent visit to a healthcare professional before taking their own lives, but only a small proportion had a mental health diagnosis at any time prior to their deaths (De Leo et al., Reference De Leo, Draper, Snowden and Kolves2013). This indicates a need to screen older people for suicide ideation across a range of health and social care settings in order to identify risk and be able to offer prevention services to this age group.
The purpose of this review was to identify existing measures that can be used to screen for, or identify, suicide ideation specifically in older age groups. Our search yielded seven individual scales published across ten articles. The need for older adult-specific measures was clear throughout however, and some scales (e.g. RFL) highlighted the unique factors of relevance to understanding suicide ideation in older populations. Psychometric properties of the measures included were generally high quality and demonstrated good rates of reliability and validity. Both the measures that focused on identifying risk factors associated with suicide and those that measured factors related to resilience showed comparable utility for clinical and healthcare screening. While there were relatively strong theoretical arguments for each of the measures reviewed, few contained any follow-up assessment of their acceptability to clinicians for more frequent use or their likelihood of being employed as part of a more generalized prevention of suicide focus for older people.
While age-appropriate measures appear to be needed, based on findings of different factors affecting wishes to live or to end one’s life with age, there is a danger of perceiving “older people” as a single homogenous group. Prevalence estimates of suicide in older age groups have reported differences across cultural and ethnic groups (Canetto, Reference Canetto2017; Cukrowicz et al., Reference Cukrowicz, Cheavens, van Orden, Ragain and Cook2011) suggesting a need for further nuance within measures of suicide ideation. There are also notable gender differences in rates of suicide in older people with older men being at significantly higher risk of using lethal methods of suicide (Neufeld and O’Rourke, Reference Neufeld and O’Rourke2009). Whether there are different indicators of suicide ideation between older men and women has yet to be examined within the research. One clear limitation in the development of the measures reviewed here is the disproportionality of the samples included in psychometric assessments. Almost all measures included a 90% or larger proportion of White participants, and most were over-represented by women. There was little consideration of broader social and environmental factors, such as financial security, access to healthcare, and living conditions, that could have additional influence on wishes to die or to continue with life alongside aspects of social support and perceived belongingness (Hodge, Reference Hodge2016).
A shift in focus from measuring risk to protective factors in determining suicide ideation in older people has been welcomed by some researchers (e.g. Deuter et al., Reference Deuter, Proctor, Evans and Jaworski2016). This is based on evidence that identifies social connectedness and a feeling of belonging as key factors in older people reporting reasons for not attempting or thinking about suicide (Joiner, Reference Joiner2005). The measures reviewed in this study that focus on positive resiliency factors have shown good levels of reliability and validity in assessing suicide ideation in older people. However, the studies reviewed did not attempt to compare scores on their measures with actual outcomes for participants, and it is not clear if these measures accurately predict suicide ideation or behavior. Edelstein et al. (Reference Edelstein2009) do suggest that such measures should be used alongside measures of suicide risk as a means of better predicting such outcomes.
One concern regarding a focus on positivity and/or resilience in determining suicide risk in older adults is that it could lead to professionals dismissing less obvious signs of mental distress in this group. If there are indications of even minimal functional well-being, would this then unconsciously exclude older people from potentially necessary mental health intervention? Though limited, there is some evidence (Frost et al., Reference Frost, Beattie, Bhanu, Walters and Ben-Schlomo2018) that HCPs focus more on physical health symptoms when treating older patients and while acknowledging that there is a high incidence of mental health difficulties including depression, it tends to be de-prioritized due to normalization and available time – physical health issues are more immediate, likely to be treatable and fit more comfortably within the remit of the skills and qualifications of HCP staff.
Overall, the authors of the articles reviewed here recognized that measuring depression alone is insufficient to track suicide ideation among older adult populations and that there are unique factors that need to be considered in this group that may not have been identified in previous scales developed for use with younger populations. The need to be aware of potential cultural differences in admitting to mental health difficulties was raised by Lee et al. (Reference Lee, Tsai, Wang, Chen and Tsai2017) in their scale development article based in Taiwan, where they note a particular reluctance for older people to endorse scale items indicating depression. However, it is not clear from our review of this literature whether this is a country or culture-specific factor that needs to be considered in the use of such scales as most scales were developed with overwhelmingly White sample groups, despite being conducted in countries with considerable ethnic diversity (e.g. USA, Canada).
The value of short, or ultra-short, scales was put forward by a number of the authors of the scales included (e.g. Awata et al., Reference Awata2007; Nugent and Cummings, Reference Nugent and Cummings2014) arguing for the need to develop measures that can be realistically used within current healthcare settings in addition to normal services. While the logic that a 69-item scale (e.g. RFL-OA) would prohibit wider use in primary, and even clinical, settings, appears reasonable, none of the studies sought the opinions of HCPs for the type of scale they would be likely to use in practice.
Perceived burdensomeness is one factor in Joiner’s theory that may contribute to the understanding of suicide ideation – an idea supported by previous studies (Cukrowicz et al., Reference Cukrowicz, Jahn, Graham, Poindexter and Williams2012). The concept of perceived burdensomeness has also been highlighted as a factor in need of independent consideration with regards to assisted suicide in those with severe mental health difficulties (Stoll et al., Reference Stoll, Ryan and Trachsel2021). While the measures we reviewed frequently included questions on social connectedness and support, none fully engaged with the theoretical issue of burdensomeness.
In addition to the points discussed above in relation to sampling in the development of the reviewed measures, there were a number of common limitations that should also be considered if any of the measures are to be used in healthcare settings. Firstly, none of the articles actively included older people themselves in the development of the measures or items to be included. Some (e.g. Carmel, Reference Carmel2017; Edelstein et al., Reference Edelstein2009) based their item development partly on interviews or surveys with older people to determine relevant factors for inclusion, but there was no further involvement of older people beyond this for any of the measures. Secondly, the variation in settings and populations chosen for initial psychometric testing of the measures means it is not clear if these scales can be applied to community, residential and inpatient groups consistently or if they are only relevant to those used in development of the scales. Finally, the lack of follow-up with healthcare practitioners on their perspectives of the measures, how likely they would be to use them in practice, or what they would need for screening to become more commonplace means that the practical utility of these measures cannot be assessed with any degree of confidence.
This review has demonstrated a need for targeted screening measures to assess suicide ideation in older adults who are likely to display unique difficulties compared to younger populations who report thoughts of suicide. Nonetheless, our review has its own limitations that should be acknowledged. Our inclusion/exclusion criteria were necessarily narrow. We actively excluded papers that reported measures that were not explicitly designed for use in older adults; even if they had been successfully used in this group. It is possible that we missed some useful scales that would further understanding of older adult’s suicide ideation through these inclusion/exclusion criteria. Our searches were also limited to papers published in the English language. Given the range of countries represented in the scales reviewed, it is likely that some potentially useful papers may have been omitted. This also limited our understanding of cultural nuances in discussing and measuring suicide ideation.
A number of recommendations for future research are apparent from this review. Firstly, there is a need for further research to determine whether scales such as those presented here have potential to be used effectively across cultural groups in place of, or alongside, existing measures of depression, anxiety, or other mental health assessment tools. Currently, there is little research on how cultural differences in understandings of mental health, and suicide, affect how people interpret and answer questions on these issues, particularly in older populations. Likewise, it would be useful to determine which scales are used in primary and clinical settings and how they are perceived in terms of their usefulness, ease of use, and relevance to professionals to better understand the impact of the number of items on the take-up of more routine screening for suicide ideation in older populations. None of the studies we reviewed had actively included older people in the development of their measures. Greater attention to incorporating co-production within these studies would benefit both the development and future use of such measures. Finally, previous qualitative studies have indicated perceived financial and caring burdensomeness is a likely factor in explaining older people’s suicide ideation (Hafford-Letchfield et al., Reference Hafford-Letchfield2018). Given reported links between this and severe depression in some (Stoll et al., Reference Stoll, Ryan and Trachsel2021), further research on how it manifests in older people, and how it can be addressed, is warranted.
While a number of measures have been developed over the past few decades to cater to this population, screening for either mental health problems, or for suicide risk is not routine in healthcare practice. The measures reviewed here showed good psychometric properties, although further research is needed to assess how likely they are to be used in practice. Evidence has shown that older people (and especially older men) are more likely to die by suicide on a first attempt compared to younger people and that they are least likely to have received a diagnosis of depression, or other mental health difficulty. It is apparent that appropriate screening measures, that both older adults and healthcare professionals find acceptable and useful, are needed to identify those most at risk so that preventative measures can be instigated where and when they are needed.
Table 3. Quality assessment scores for each article reviewed

Conflict of interest
None.
Description of authors’ roles
HG co-designed the study and wrote the first draft of the full paper.
CR conducted the literature search, data extraction and contributed to the final draft of the paper.
TH-L co-designed the study and contributed to the final draft.
TE contributed to the final draft and assisted in the data extraction.