Introduction
Agitation is a common clinical manifestation of many neuropsychiatric disorders. It is a frequent manifestation of Alzheimer's disease (AD), frontotemporal dementia (FTD), dementia with Lewy bodies (DLB), and other dementia syndromes (Ballard and Corbett, Reference Ballard and Corbett2010; Manoochehri and Huey, Reference Manoochehri and Huey2012; Bruns and Josephs, Reference Bruns and Josephs2013). It occurs in schizophrenia, bipolar illness, and depression (Gonzalez et al., Reference Gonzalez2013; Swann, Reference Swann2013). While agitation may include aggressive behaviors, it is not identical to aggression, and agitation can occur without aggression (e.g. pacing, rocking, repetitious mannerisms). Agitation can precipitate institutionalization (Okura et al., Reference Okura, Plassman, Steffens, Llewellyn, Potter and Langa2011), diminishes the quality of life of patients and caregivers (Khoo et al., Reference Khoo, Chen, Ang and Yap2013), and, when severe, may require treatment with medications (Herrmann and Lanctôt, Reference Herrmann and Lanctôt2007). There is an emerging biology of agitation, and frontal lobe dysfunction is implicated in both clinical and neuroimaging studies (Senanarong et al. Reference Senanarong2004; Bruen et al., Reference Bruen, McGeown, Shanks and Venneri2008). Treatment of agitation – both pharmacologic and non-pharmacologic – is an unmet need in the care of patients with cognitive impairment (Herrmann and Lanctôt, Reference Herrmann and Lanctôt2007; Gitlin et al., Reference Gitlin, Kales and Lyketsos2012).
In spite of the framework of studies that have begun to increase understanding of agitation, there is no commonly accepted consensus description of this common clinical phenomenon (Laughren, Reference Laughren2001). Lay definitions of agitation are non-specific and include states of excitement, disturbance, or worry. A consensus definition of agitation applicable in the setting of cognitive impairment would facilitate a wide spectrum of research, including pharmacologic and non-pharmacologic intervention studies, epidemiologic investigations of agitation, clinical studies, and research on the neurobiology of this behavior. A definition would also provide a common framework for diagnostic nomenclatures such as the International Classification of Diseases and Related Health Problems (ICD; (World Health Organization, 2014) and the Diagnostic and Statistical Manual of Mental Disorders (DSM; (American Psychiatric Association, 2013). In addition, clinically relevant definitions have important regulatory applications; when agents possibly appropriate for the treatment of agitation are presented to the Food and Drug Administration (FDA), European Medicines Agency (EMA), or other licensing authorities, the treatment indication must be defined using language useful to clinicians caring for patients with the condition. Without a consensus definition, it is difficult to compare studies or to know what range of behaviors were included in a study of “agitation.”
Rating scales such as the Cohen-Mansfield Agitation Inventory (Cohen-Mansfield et al., Reference Cohen-Mansfield, Marx and Rosenthal1989), Neuropsychiatric Inventory (NPI; Cummings et al., Reference Cummings, Mega, Gray, Rosenberg-Thompson, Carusi and Gornbein1994), or Behavioral Pathology in Alzheimer's Disease (BEHAVE-AD; Reisberg et al., Reference Reisberg, Borenstein, Salob, Ferris, Franssen and Georgotas1987; De Deyn and Wirshing, Reference De Deyn and Wirshing2001) are often used to identify patients for clinical trials of anti-agitation agents and to measure the clinical symptoms in other descriptive and intervention studies. Rating scales, however, are not definitions; rather, they are means of measuring the frequency or severity of symptoms. Most clinicians do not use rating scales for routine care of patients. To assist in defining populations for clinical care and research, a definition that is not dependent on a particular rating scale is needed.
The International Psychogeriatric Association (IPA) has an established leadership role in the field of geriatric behavioral health, including agitation, and has led initiatives involved with this topic (Finkel et al., Reference Finkel, Costa e Silva, Cohen, Miller and Sartorius1996; Reisberg et al., Reference Reisberg, Auer, Monteiro, Boksay and Sclan1997; Draper, Reference Draper1999; Finkel, Reference Finkel2000). To advance the study of agitation by establishing a consensus definition, the IPA formed an Agitation Definition Working Group (ADWG) to produce a provisional consensus definition of agitation. The ADWG conducted a broadly inclusive process, involving the IPA and its affiliate members, employing electronic means of participant engagement, holding a face-to-face meeting with international representation, and using survey-based methods. The ADWG was made up of the IPA leadership and other stakeholders interested in the neuropsychiatric aspects of AD and other disorders. The ADWG implemented a transparent process that included nearly 1,000 survey respondents and engaged the memberships of the IPA, IPA affiliates, and other organizations involved in the care and research of neuropsychiatric disorders in patients with cognitive impairment. Here the process is described, the definition is presented, and the elements of the definition are discussed.
Methods
Consensus-building process
Initial formulation
The literature was reviewed (by Jeffrey Cummings), past definitions of agitation identified, and common elements of the definitions reviewed. A preliminary survey of these definitions and elements to be considered for inclusion was developed and presented to the IPA leadership.
Survey 1
The ADWG was formed to guide this project. The ADWG reviewed the proposed survey, adding or deleting elements to enhance the focus and clarity of the questions. The revised survey was sent electronically to the IPA membership and affiliate members (organizations that share the mission of advancing clinical practice, research, and education to improve the mental health of the elderly). The survey collected demographic information on the respondents, determined the preferences among five definitions of agitation used in the literature (Kong, Reference Kong2005), asked if the definition should be limited to cognitive impairment syndromes, established key behavioral elements to be included in a definition, and interrogated whether the respondents considered agitation and anxiety to be the same and whether agitation and aggression are the same.
International expert consensus meeting
Following completion and analysis of the first survey, an international expert consensus meeting was held to develop a draft definition based on a review of the literature and information derived from the survey. The members of the ADWG present at the meeting include the authors of this paper. In this meeting a draft definition was developed that represented a consensus of those present. Following the expert meeting, a preliminary draft of the definition was developed and circulated to all members of the ADWG. Through multiple electronic exchanges a final consensus was reached (Table 1). Not all aspects of the consensus definition were unanimously endorsed by all participants but a majority of stakeholders agreed on the elements.
Table 1. Consensus provisional definition of agitation in cognitive disorders

To develop further consensus beyond the ADWG, other key stakeholder groups received the provisional definition for comments, including the members of the Neuropsychiatric Syndrome Professional Interest Area of ISTAART (Geda et al., Reference Geda2013) comprising thought leaders in the area of neuropsychiatric aspects of AD.
Survey 2
Once an expert consensus from the ADWG was achieved, the IPA and affiliate members were re-contacted to provide additional input into the definition and its acceptability for clinical and research studies, including prospective validation investigations. Six thousand emails were sent; there were 350 respondents (7%) in this phase of the consensus development process.
Report preparation
Once the second survey was complete, this report containing a description of the consensus process, the definition, and the elements of the definition was prepared (Jeffrey Cummings) and circulated among the ADWG members. Agreement was reached on the text describing the provisional definition and the manuscript was submitted to International Psychogeriatrics for review.
Results
Survey 1
Six thousand emails were sent; 557 individuals responded. The response rate from IPA members was 30.1%. Many members of the IPA and affiliate organizations are involved predominantly with mood disorders, psychosis, or other non-dementia aspects of geriatric psychiatry. Of the 557 respondents, 382 were physicians, including 292 psychiatrists. Other professional disciplines providing responses included nurses (57), psychologists (50), occupational therapists (13), social workers (14), and others/no responses (41). Three hundred eighty-eight (70%) of the respondents had been in practice for more than ten years.
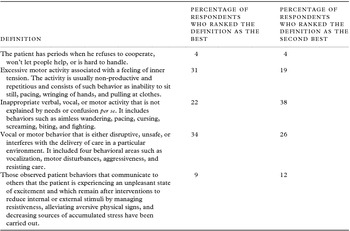
This initial survey provided valuable insights from those involved in the care of agitated patients, and key elements of the definition were identified. Table 2 shows the responses to five existing definitions of agitation (Kong, Reference Kong2005). Three of the definitions had relatively high acceptability (22–34% rating as the “best definition”).
Table 2. Five proposed definitions of agitation in dementia and the number of respondents who ranked each of them as the best or the second-best definition
The ADWG surveyed essential elements of the definition of agitation. The percentage of respondents identifying specific adjectives as key behavioral elements of the definition included: excessive (71%), inappropriate (54%), repetitive (46%), observable (64%), dangerous (24%), and disruptive (56%) (Table 3).
Table 3. Proposed elements of a definition of agitation and the percentage of respondents endorsing that item as an essential element of a definition of agitation
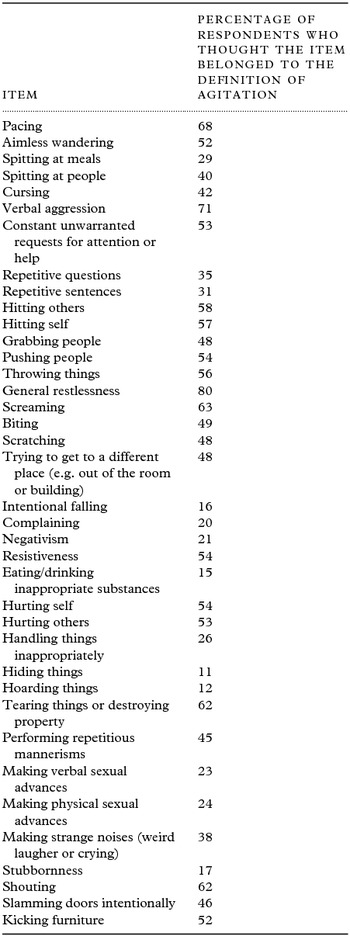
Of the items listed as possible behaviors to be included in a definition of agitation, the following were endorsed by at least 50% of the respondents: pacing, aimless wandering, verbal aggression, constant unwarranted requests for attention or help, hitting others, hitting self, pushing people, throwing things, general restlessness, screaming, resistiveness, hurting self, hurting others, tearing things or destroying property, shouting, and kicking furniture (Table 4). This information guided the elements included in the definition by the ADWG.
Table 4. Behaviors that survey respondents indicated should be included in a definition of agitation
When queried as to whether agitation and anxiety were the same, overlapping, or distinct concepts, most of the respondents found them to be overlapping (0.3%, 61%, and 37% respectively). When asked whether agitation and aggression are the same, overlapping, or distinct, 0.8%, 66%, and 32% endorsed each option.
Survey 2
Table 5 lists the questions of the survey regarding the definition developed by the ADWG and the responses of the participants. All elements of the definition surveyed were rated as “strongly agree” or “somewhat agree” by a majority of the respondents (ranging from 68.2% for “the exclusion criterion is clear” to 88.8% for “the physical aggression components are captured appropriately in the definition”). A majority agreed (strongly or somewhat) that the definition is appropriate for research application. For non-interventional descriptive clinical research, 44% strongly agreed and 33.7% somewhat agreed with the appropriateness of the definition (77.7% agreed); for pharmacologic interventional clinical research, 43.7% strongly agreed and 31.7% somewhat agreed (75.4% agreed); and for clinical trials 39.2% and 36% agreed strongly and somewhat respectively (75.2% agreed).
Table 5. Questions of survey 2 exploring the acceptability of the draft definition and the percentage of participants who responded as strongly agree or somewhat agree

When queried whether the definition should be limited to cognitive impairment syndromes – the approach taken by the ADWG – 67.4% said “yes.”
Discussion
Elements of the consensus definition
The provisional consensus definition uses the DSM style for defining a disorder as one that produces disability (American Psychiatric Association, 2013). The definition is limited to patients with cognitive impairment, requires evidence of emotional distress, requires one of the three observable types of behavior (excessive motor activity, verbal aggression, or physical aggression), specifies that the behavior causes excess disability, and notes that the behaviors cannot be solely attributable to a suboptimal care environment or another disorder such as psychiatric illness, medical illness, or effects of a substance.
Provisional consensus definition
The definition is labeled as “provisional” because it may evolve as it is subjected to prospective validation. It represents an important starting point in a dynamic dialogue that will evolve with clinical application, research, and review. Validation studies are expected to show that some elements are better suited to clinical and research applications than others.
The definition was labeled as a “consensus” because a majority of stakeholders involved in the process concurred with the current definition. Not all elements were unanimously endorsed; a consensus was achieved on all aspects of the definition.
Limitation to syndromes with cognitive impairment
Agitation occurs in many disorders and is not limited to conditions with cognitive impairment (Ballard and Corbett, Reference Ballard and Corbett2010; Manoochehri and Huey, Reference Manoochehri and Huey2012; Bruns and Josephs, Reference Bruns and Josephs2013; Gonzalez et al., Reference Gonzalez2013; Swann, Reference Swann2013). The ADWG and the participating members of the surveys favored limiting the definition to disorders with cognitive impairment. Sixty-seven percent of Survey 2 respondents agreed with this approach.
There are currently separate definitions for psychosis of AD and psychosis in schizophrenia even though they have shared elements such as delusions and hallucinations (Jeste and Finkel, Reference Jeste and Finkel2000); similarly there are definitions of major depression and depression in AD that are overlapping but not identical (Olin et al., Reference Olin2003). Similar considerations may apply to agitation, and we chose to develop a definition explicitly for patients with cognitive impairment. Further research may lead to modifications of this approach.
The FDA has expressed concern about “pseudo-specificity” of syndromes that are artificially assigned to one disorder when they represent general syndromes for which drugs are already approved (Cummings and Jeste, Reference Cummings and Jeste2007), and the ADWG wished to avoid constructing a definition that might raise this issue. Our definition applies specifically to the type of agitation observed in patients with cognitive impairment based on the unique relationships of agitation with aspects of cognition (Senanarong et al., Reference Senanarong2004); a distinct pathophysiology (Bruen et al., Reference Bruen, McGeown, Shanks and Venneri2008; Trzepacz et al., Reference Trzepacz2013); and possibly a differential response to treatment compared with syndromes such as psychosis of AD (Schneider et al., Reference Schneider, Dagerman and Insel2006).
Subjective aspect
The definition requires that there be observed or inferred evidence of emotional distress. Examples of behaviors indicative of emotional distress are provided, including rapid changes in mood, irritability, or emotional outbursts. The ADWG required this subjective element because agitation as conceived by the panel includes the concept that the patient is upset or distressed, and the agitated behavior is an expression of this emotional state. A person could exhibit purposeful aggression with behaviors overlapping with the definition but would not be classified as “agitated” if there was no associated distress. It is also important that patients not be treated when their behavior is upsetting to someone else (a family member or caregiver) but not to the patient. Requiring the subjective element of the definition makes this less likely. It is not possible to directly observe emotional states, and they must be inferred from observable behaviors. In all, 78.2% of the Survey 2 respondents strongly (42.8%) or somewhat (35.4%) agreed that this aspect of agitation was captured appropriately by the proposed definition.
Sustained
A single episode or short-lived period of behavioral change would not meet the definition for agitation developed by the ADWG. The definition applies to a chronic or at least long-lasting state that has been sustained, persisted, or been frequently recurrent for at least two weeks. This aspect of the definition will assist with intervention studies (pharmacologic and non-pharmacologic) where interventional groups are compared and sustained behavioral changes are required to see a difference in the study outcomes.
Change from previous behavior
The ADWG limited the definition of agitation to patients with cognitive impairment. Behaviors that preceded the onset of the associated cognitive disorder would not be included in this definition. This aspect of the consensus definition is similar to the precedent adapted in the definition of psychosis of AD (Jeste and Finkel, Reference Jeste and Finkel2000).
Observable behaviors
The patient must have at least one type of observable agitated behavior. The behaviors can include excessive motor activity (such as pacing, rocking, gesturing, pointing fingers, restlessness, performing repetitious mannerisms), verbal aggression (e.g. yelling, speaking in an excessively loud voice, using profanity, screaming, shouting), or physical aggression (e.g. grabbing, shoving, pushing, resisting, hitting others, kicking objects or people, scratching, biting, throwing objects, hitting self, slamming doors, tearing things, and destroying property). These behaviors are the core aspects of the agitation syndrome; they reflect the behaviors endorsed in Survey 1 as comprising agitation. The ADWG recognized that agitated patients exhibit different repertoires of behaviors and that, in the presence of emotional distress, any of the behaviors described would fulfill this criterion of the definition. Clinician judgment is not prohibited by the definition and behaviors other than those listed may be present in agitated patients. In all, 88.8% of the Survey 2 respondents strongly (65.7%) or somewhat (23.1%) agreed that the proposed definition appropriately captured the physical aggression aspects of agitation, and 87.9% strongly (59.7%) or somewhat (28.2%) agreed regarding the verbal aspects of agitation.
Excess disability
A disorder is defined as producing disability (American Psychiatric Association, 2013), and the ADWG incorporated this aspect of the definition as a measure of the clinical meaningfulness of the behavior. If the behavior produces no disability for the individual in terms of interpersonal relationships, social function, or impact on daily living activities, then it would not meet this criterion of the definition. The disability must be more than can be attributed solely to the cognitive impairment syndrome. Clinician judgment will be required to make this determination.
Necessary exclusions
Agitation has many possible causes and is seen across a broad range of neuropsychiatric illnesses (Ballard and Corbett, Reference Ballard and Corbett2010; Manoochehri and Huey, Reference Manoochehri and Huey2012; Bruns and Josephs, Reference Bruns and Josephs2013; Gonzalez et al., Reference Gonzalez2013; Swann, Reference Swann2013). The definition proffered by the ADWG requires the presence of an underlying cognitive impairment syndrome such as AD, FTD, DLB, or a prodromal dementia state. In some cases, patients with these disorders may have other psychiatric illness, medical illness, use substances, or be in suboptimal care environments that can cause agitated behaviors. The ADWG definition requires that the agitation not be attributable solely to one of these co-existing conditions. Clinician judgment may be required to make this determination. The exclusion aspects of the definition had some of the lowest endorsements on Survey 2 as 38.5% strongly agreed and 36.8% somewhat agreed that the exclusions were adequate for clinical application; 26% strongly agreed and 42.2% somewhat agreed that the exclusions were adequate for research application.
Comment on the definition
The ADWG definition of agitation with cognitive impairment is broad and assumes that agitation is a syndrome and not a response to another disorder. An alternative approach is to define an “agitation with psychosis,” “agitation with depression,” etc. An extensive literature establishes that agitation can be seen in the absence of concomitant psychopathology; neuroimaging studies suggest unique regional dysfunction that is distinct from other disorders (Bruen et al., Reference Bruen, McGeown, Shanks and Venneri2008; Trzepacz et al., Reference Trzepacz2013); and clinical trials demonstrate that the pharmacologic response of agitation may differ from that of other types of behavioral disturbances (Schneider et al., Reference Schneider, Dagerman and Insel2006). Therapies have been approved for agitation in multiple psychiatric settings (e.g. aripiprazole for acute treatment of agitation with schizophrenia or bipolar I disorder), setting a precedent for viewing agitation as a distinct syndrome. While no drug has been approved for agitation per se (i.e. without aggression, depression, or psychosis), several psychosocial interventions have shown benefit in reducing agitated behavior (Low et al., Reference Low2013). The ADWG favored defining agitation as a distinct clinically identifiable syndrome.
Using a syndromal definition of clinical phenomena within neurologic disorders has a precedent in the identification of pseudo-bulbar affect (PBA) and the approval of dextromethorphan/quinidine for PBA across neurologic disorders after having demonstrated efficacy in amyotrophic lateral sclerosis and multiple sclerosis. A similar strategy of showing efficacy for anti-agitation agents across several disorders could be adopted in anti-agitation drug development programs.
The relationship of agitation to aggression sparked discussion. These are overlapping but not identical concepts (Cohen-Mansfield and Mintzer, Reference Cohen-Mansfield and Mintzer2005). Agitation can occur in the absence of aggression, and predatory aggression can occur without agitation; it is unlikely that aggression occurs without agitation in the cognitive impairment syndromes described by the ADWG. Sixty-six percent of the survey respondents consider agitation and aggression as overlapping concepts; 32% consider them to be distinct. Aggression may be a more severe form of agitation or it may occur in differing biological or psychological circumstances. The comparative response profiles to pharmacologic or non-pharmacologic interventions of agitation with and without aggression have not been comprehensively explicated. There is currently insufficient evidence to conclude that agents or interventions used for aggressive agitation would necessarily work or be warranted in non-aggressive agitation. The ADWG definition criterion B allows both agitation without aggression (excessive motor activity) and with aggression (verbal aggression and physical aggression). Investigators using this definition of agitation should note which elements of criterion B were met (e.g. excessive motor activity, verbal aggression, or physical aggression). Longitudinal comparison of studies will help define the relationship between agitation and aggression, and the ADWG definition will advance understanding of this aspect of agitation.
This definition will be useful in the study of psychosocial interventions and in clinical trials of anti-agitation agents. The absence of a consensus definition may have contributed to the lack of activity in developing new therapies for agitation with cognitive impairment; no agent has been approved for treatment of this syndrome in spite of extensive documentation of the disability associated with agitation. Study entry would require that the participants have agitation as defined by the ADWG. A minimum baseline severity level on an agitation scale would typically be required. An outcome measure – usually an agitation measure different from the one used to define entry severity – would be used to compare baseline with end-of-study scores for the active treatment and the placebo (or active comparator) control group. It may be useful to control for other behavioral features such as mood changes or psychosis. The ADWG definition could play a critical role in defining the patient population for such trials.
The development of a provisional definition of agitation is the first step in advancing a research agenda for the definition. Validity studies using other agitation assessments, reliability of the application of the definition, usefulness in clinical trials, usefulness in non-pharmacologic research, and real-world application in clinical and healthcare settings will lead to refinements and adjustments that will enhance the definition and advance the study of neuropsychiatric syndromes in cognitive impairment disorders.
Conflict of interest declaration
The sponsors, Otsuka and Avanir Pharmaceutricals, gave unrestricted education grants to help support the international meeting that was part of the definition-building process.
Dr. Jeffrey Cummings has provided consultation to Acadia, ADAMAS, Anavex, Avanir, Boehinger-Ingelheim, Eisai, EnVivo, GE Healthcare, Genentech, Lilly, Lundbeck, Medavante, Merck, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Resverlogix, Roche, Sonexa, Suven, Takeda, and Toyoma companies. Dr. Cummings owns the copyright of the Neuropsychiatric Inventory.
Professor Sube Banerjee has received consultancy fees, honoraria for speaking, and support in attending conferences from the makers of anti-dementia medication and other psychotropics, including Abbvie, Eisai, Pfizer, Novartis, Lilly, and Shire.
Professor Henry Brodaty has served as investigator for Janssen, Lilly, Medivation, Merck, Sanofi, Servier, and Tau Therapeutics, and has been on the advisory boards of Pfizer, Novartis, Janssen, Lundbeck, and Nutricia. Dr. Brodaty has provided consultation to Baxter, Lilly, Merck, and Nutricia.
D.P. Devanand has received research support from Eli Lilly, and has provided consultation to AbbVie.
Dr. Serge Gauthier has been on the scientific advisory board or investigator with Abbvie, Affiris, Eisai, Lilly, Navidea, Novartis, Pfizer, Sanofi-Synthelabo, Servier, and TauRx.
Professor Robert Howard reports that he has no relevant disclosures to make.
Dr. Krista Lanctôt has had research support and/or speaker's honoraria from Abbvie Canada, Lundbeck Canada Inc., Pfizer Canada Inc., Janssen Ortho, and Rocheand Wyeth.
Dr. Constantine Lyketsos has received grant support (research or CME) from Associated Jewish Federation of Baltimore, Weinberg Foundation, Forest, GlaxoSmithKline, Eisai, Pfizer, Astra-Zeneca, Lilly, Ortho-McNeil, Bristol-Myers, Novartis, National Football League, Elan, and Functional Neuromodulation. Dr. Lyketsos has been a consultant or advisor to Astra-Zeneca, GlaxoSmithKline, Eisai, Novartis, Forest, Supernus, Adlyfe, Takeda, Wyeth, Lundbeck, Merz, Lilly, Pfizer, Genentech, Elan, NFL Players Association, NFL Benefits Office, Avanir, Zinfandel, BMS, Abvie, Janssen, and Orion. Honorarium or travel support has been received from Pfizer, Forest, GlaxoSmithKline, and Health Monitor.
Dr. Jacobo Mintzer reports receipt of grants to his institution from Takeda Global Research and Development Center, Pfizer, Genentech, Merck, Accera, Elan, Avanir, F. Hoffmann-La Roche, Novartis, Baxter, Eli Lilly, Wyeth, and Janssen Alzheimer Initiative; and employment with NeuroQuest, and BioPharma Connex.
Dr. Elaine Peskind has been on the speakers’ bureau for Forest Pharmaceuticals and on the Advisory Committee for Avanir. Dr. Peskind served on the Adjudication Committee for Takeda Pharmaceuticals.
Dr. Anton Porsteinsson has received a grant for his institution from Avanir, Eisai, Elan, Genentech/Roche, Janssen Alzheimer Initiative, Merck, Pfizer, and Toyama. He has provided consultation for Elan, Janssen Alzheimer Initiative, and TransTech Pharma. Dr. Porsteinsson has membership on data safety and monitoring boards for Quintiles.
Dr. Edgardo Reich has participated as investigator in different pharmaceutical-sponsored trials for Ely Lilly, Glaxo, Forest, Mertz. Astra Zeneca, Novartis, Roche, and Janssen. He has received travel grants from Bayer, MerckSerono, Novartis, Mertz, and Teva.
Dr. Cristina Sampaio has been a consultant for Abbvie, Alkermes, AstraZeneca, Avanir, Biogen, BMS, Chelsea, Genzyme, Lilly, Lundbeck, Otsuka, Pfizer, Roche, Sanofi, Servier, Takeda, and Teva.
Dr. Mary Sano has been on the Scientific Advisory Board for Medication and as a consultant for Bayer Schering Pharma, Bristol-Meyers Squibb, Elan, Genentech, Medivation, Medpace, Pfizer, Janssen, Takeda, and United Biosource.
Dr. David Steffens is supported through grants from the National Institute of Mental Health, and he receives textbook royalties from the American Psychiatric Press.
Dr. Marc Wortmann reports no other salaries than from Alzheimer's Disease International.
Dr. Kate Zhong has provided consultation to Avanir, Pfizer, Janssen, and Wyeth Pharmaceuticals.
Description of authors’ roles
J. Cummings, J. Mintzer, H. Brodaty, and M. Sano formulated the research questions, designed the study, carried out the study, analyzed the data, and wrote the paper.
S. Banerjee, D. Devanand, S. Gauthier, R. Howard, K. Lanctôt, C. Lyketsos, E. Peskind, A. Porsteinsson, E. Reich, C. Sampaio, D. Steffens, M. Wortmann, and K. Zhong carried out the study, analyzed the data, and wrote the article.
Acknowledgments
Two industry stakeholders provided unrestricted educational grants to help support the consensus development process. They did not influence the work plan, study implementation, data collection, data interpretation, or drafting of the manuscript.