To the Editor—Healthcare workers (HCWs) experience various levels of exposure to severe acute respiratory coronavirus virus 2 (SARS-CoV-2); however, evidence is limited on if any subsets of staff are at higher risk of acquiring coronavirus disease 2019 (COVID-19) disease compared to others or the general community. Current knowledge on the significance of “level of exposure” is limited due to (1) data obtained largely during surges, (2) data from major healthcare systems (generalizability), (3) lack of adjustment for exposures outside the health system or for compliance with public health and PPE recommendations, and (4) focusing on only high-risk clinical providers. Reference Jeremias, Nguyen and Levine1-Reference Godbout, Pryor and Harmon5 Accordingly, we performed a cross-sectional analysis evaluating the seroprevalence of SARS-CoV-2 antibodies in HCWs in a community health system in region of moderate disease burden. The study was approved by the Metro-Health University of Michigan Health Institutional Review Board and consent was obtained electronically.
Kent County, Michigan (population 650,000), experienced a “moderate surge” in coronavirus cases during mid-May through June 2020. At the time of the study the county had reported >180 deaths and >8,000 cases, with a prevalence of 1,380 per 100,000 population. The health system is comprised of a 210-bed community-based teaching hospital with multiple outpatient centers, urgent care, and surgery centers. COVID-19 units were established on March 11, 2020, along with policies for extended N95 mask use, eye protection, limited staff entrances, staff screening, and restricted visitor policies. On April 10, all emergency department encounters required staff to wear an N95 mask. Universal mask use for all staff was implemented on May 4. No PPE shortages occurred.
Survey invitations were sent via e-mail. Participants were excluded if they were <18 years of age or reported active COVID-19. An orthogonal testing algorithm was utilized (August 17–September 4, 2020) via the Siemens Atellica Total Antibody instrument (100% sensitivity and 99.8 specificity) followed by a confirmatory high-sensitivity enzyme-linked immunosorbent assay, immunoglobulin G ELISA (Eagle Bioscience, 100% sensitivity and 88.7% specificity).
For the primary outcome, we investigated whether working on a COVID-19 unit, predicted seropositivity to SARS-CoV-2 antibodies after adjusting for risk of exposure outside of work and compliance with PPE use. Secondary outcomes included modeling if a “clinical provider” or if “perceived high risk of COVID-19 exposure” at work predicted seroprevalence. We investigated whether the seroprevalence in HCWs differed from the community using the 95% confidence interval for Michigan during the study period as determined by the Centers for Disease Control and Prevention (CDC, 3%–6%). Reference Bajema, Wiegand and Cuffe6
We used SAS version 9.4 software (SAS Institute, Cary, NC) for statistical analyses. Continuous variables were compared with 2-tailed t tests or the Wilcoxon rank-sum test, as appropriate. Categorical variables were compared using the χ2 or the Fisher exact test. The 95% confidence interval for seroprevalence was calculated using the asymptotic approximation method. Multivariate logistic regression models were used to evaluate odds of seropositivity for SARS-CoV-2 antibodies by risk of exposure at work. P < .05 was considered significant.
Overall, 1,385 HCWs participated (45%). Demographics and bivariate analysis are listed in Table 1. The seroprevalence was 1.88% (95% CI, 1.16%–2.59%); significantly lower than the lower bounds of the community 95% confidence interval (P = .014). For HCWs to have had a significantly higher prevalence, the true community population prevalence would have had to have been <1.35% (1-sided P value = .045). We detected no difference in the seroprevalence of SARS-CoV-2 antibodies when exposure risk was modeled as working in a COVID-19 unit (adjusted OR, 1.7; 95% CI, 0.75–3.86) or working as a clinical provider (adjusted OR, 1.89; 95% CI, 0.83–4.29). However, when risk of exposure was modeled as “perceived high risk of work exposure” a significant increased risk of seropositivity was detected (adjusted OR, 3.4; 95% CI, 1.45–8.01).
Table 1. Demographics and Clinical Characteristics of Study Participants
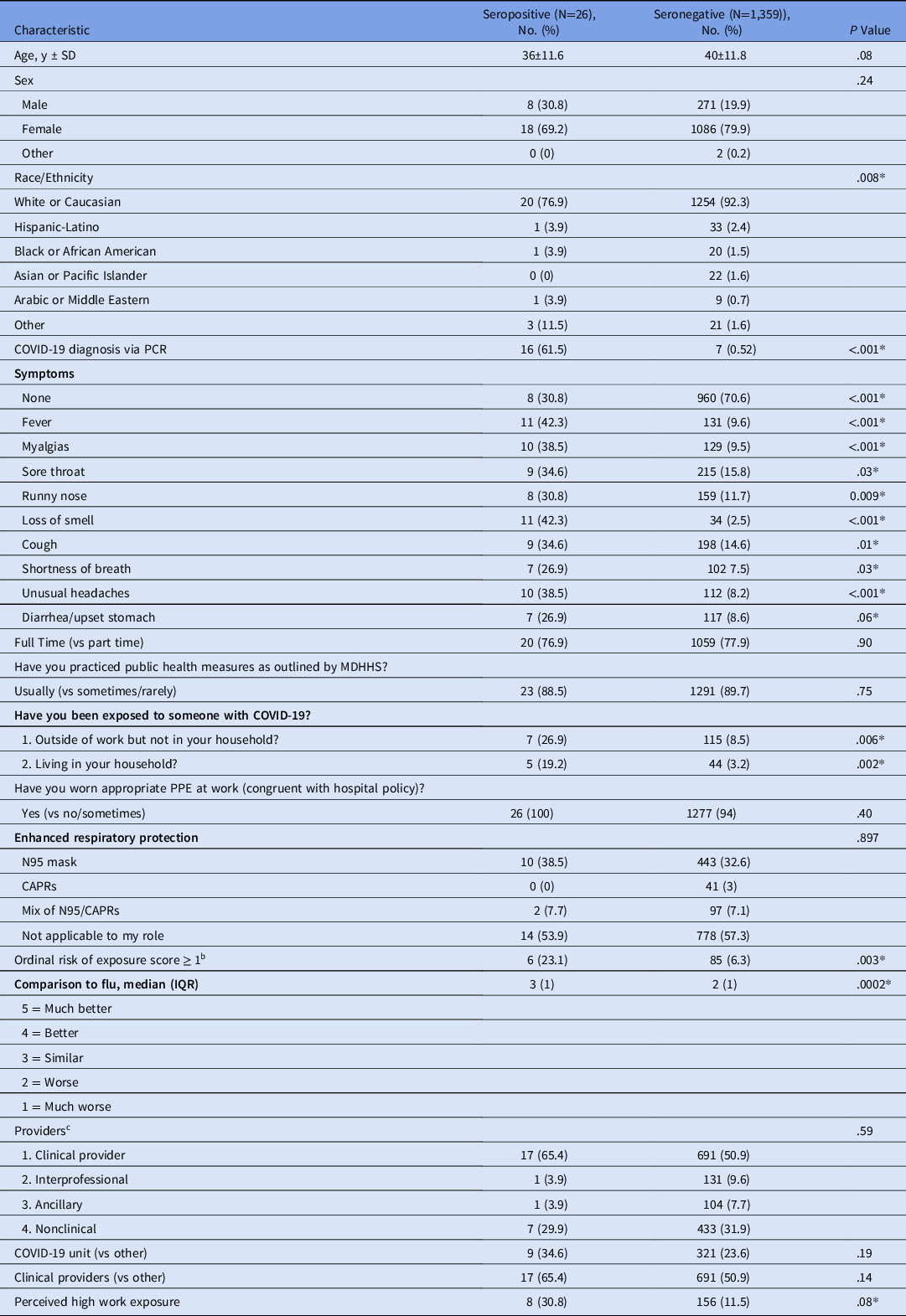
Note. SD, standard deviation; PCR, polymerase chain reaction; MDHHS, Michigan Department of Health and Human Services; PPE, personal protective equipment; CAPR, controlled air purifying respirator; IQR, interquartile range.
a May not add up to 100% as participant may have reported multiple symptoms.
b Scale components (points). Exposure to a known or suspected COVID patient in the community (1). Exposure to known COVID patient in home (2). Sometimes adhering to public health measures (1) or rarely adhering to public health measures (2). Not adhering to PPE policy at work (1).
c Providers (clinical providers with most patient exposure): physicians, residents, APPs, nurses, MA, respiratory therapists. Interprofessional services: nutrition/RD, social work, case management, PT, OT, SLP, pharmacy. Ancillary services: radiology technicians, lab. Nonclinical: clerical, administrative, research, security, food services, maintenance, housekeeping, other.
We failed to demonstrate an increased risk of infection with COVID-19 among staff at the highest risk of exposure within a community health system during a time of moderate community prevalence. Our findings are consistent with other studies that have used various definitions of “high risk” but failed to demonstrate an increased risk of COVID-19 in those at highest risk of exposure within the health system. Reference Jeremias, Nguyen and Levine1-Reference Steensels, Oris and Coninx3,Reference Korth, Wilde and Dolff7 Similar to a study of a large cohort in New York, we did demonstrate that HCWs who perceived a high risk of exposure at work were more likely to develop SARS-CoV-2 antibodies. Reference Moscola, Sembajwe and Jarrett2 Further study on perceived exposure among HCWs exposure seems warranted.
Like others, we found a low seroprevalence of SARS-CoV-2 antibodies in HCWs (1.88%), suggesting that adequate PPE and infection control prevention measures are effective in preventing disease transmission. Reference Moscola, Sembajwe and Jarrett2,Reference Yogo, Greenwood and Thompson4,Reference Godbout, Pryor and Harmon5 However, this finding is contrary to other evidence reporting that frontline HCWs may have an increased risk of acquiring COVID-19 disease compared to the community in general. Reference Celebi, Piskin and Beklevic8-Reference Iversen, Bundgaard and Hasselbalch10 These conflicting results are likely due to differences in infection prevention, preparedness, testing methods, and disease burden in the region tested, all of which have evolved over time.
The strengths of our study include the ability evaluate the independent contribution of work exposure after adjusting for adherence to PPE, public health measures, and exposure in the home or community. Additionally, our results should be generalizable to the broad health system. We acknowledge that selection bias may exist because only 45% of HCWs chose to participate in the study.
In conclusion, no association between level of exposure to COVID-19 and risk of seropositivity to SARS-CoV-2 antibodies was demonstrated in this study. The seroprevalence among HCWs was low and consistent with or below expected community seroprevalence.
Acknowledgments
Financial Support
No financial support was provided relevant to this article.
Conflicts of Interest
All authors report no financial disclosures or conflicts of interest.




