External ventricular drain (EVD) insertion may lead to serious complications including infection, which increases the risk of poor neurosurgical outcomes, increases healthcare costs, and prolongs hospital stays. Reference Fried, Nathan and Rowe1 The incidence of EVD infection ranges from 0% to 45% Reference Lozier, Sciacca, Romagnoli and Connolly2–Reference Sheppard, Ong and Lagman21 ; the largest study reported that ∼4% of EVDs placed resulted in infection. Reference Bischoff, Schröder, Gastmeier and Geffers4 Many interventions for reducing infection risk have been proposed. Factors previously associated with increased risk of EVD infection include prolonged EVD drainage, cerebrospinal fluid (CSF) leak, EVD manipulation including frequency of CSF sampling, tract hemorrhage at placement, and insufficient hair clipping. Reference Fried, Nathan and Rowe1–Reference Flint, Toossi and Chan6,Reference Phan, Schultz and Huang8–Reference Rahman, Whiting and Fauerbach20,Reference Hader and Steinbok22,Reference Hepburn-Smith, Dynkevich and Spektor23 Factors associated with reduced risk include perioperative and immediate postoperative antibiotics, as well as antibiotic-impregnated EVDs. Reference Sheppard, Ong and Lagman21,Reference Moussa and Mohamed24–Reference Wong, Ip and Poon29 Some additional risk factors for which there has been no conclusive association with EVD infection include age, sex, Glasgow coma scale (GCS) score, elevated intracranial pressure (ICP) at time of EVD placement, systemic infection, prolonged use of postprocedural antibiotics, prolonged hospital stay prior to EVD placement, involuntary EVD disconnection, placement by a junior surgeon, or coverage of the insertion site with a dressing. Reference Fried, Nathan and Rowe1–Reference Flint, Toossi and Chan6,Reference Phan, Schultz and Huang8–Reference Rahman, Whiting and Fauerbach20,Reference Hader and Steinbok22–Reference Trick, Kioski and Howard25 Controversy continues over whether specific indications for EVD placement (eg, brain trauma or intracranial hemorrhage), history of previous EVD placement, prior neurosurgery, and EVD irrigation contribute to infection risk. Reference Fried, Nathan and Rowe1–Reference Flint, Toossi and Chan6,Reference Phan, Schultz and Huang8–Reference Rahman, Whiting and Fauerbach20,Reference Hader and Steinbok22–Reference Trick, Kioski and Howard25
Several institutions, including our own, have demonstrated a significant reduction in EVD infections through implementation of protocols for EVD insertion and maintenance. Reference Muralidharan3,Reference Flint, Toossi and Chan6–Reference Phan, Schultz and Huang8,Reference Kubilay, Amini and Fauerbach10,Reference Camacho, Boszczowski and Freire11,Reference Kitchen, Singh and Hulme13–Reference Dasic, Hanna, Bojanic and Kerr15,Reference Korinek, Reina and Boch17,Reference Rahman, Whiting and Fauerbach20,Reference Hepburn-Smith, Dynkevich and Spektor23,Reference Walek, Leary, Sastry, Asaad, Walsh and Mermel30 In 2007, the Department of Epidemiology and Infection Control at our institution identified a high incidence of EVD infections and, in response, formed an EVD Infection Control Committee. This committee has recorded all EVD infections as they have occurred, has periodically recommended changes in practice, and has assessed the impact of these interventions over time. Major elements of this protocol include minimal EVD manipulation after insertion, no routine CSF sampling, and regular cleansing of the insertion site with alcoholic chlorhexidine while the EVD is in situ. Reference Walek, Leary, Sastry, Asaad, Walsh and Mermel30
We undertook a retrospective review of prospectively collected data regarding EVD infections among adult or pediatric patients who received an EVD from March 2015 to May 2019 at our 719-bed, tertiary-care, academic medical center.
Methods
Data collection and outcome measures
With approval from our institutional review board (no. 1396435), clinical data were collected from the electronic medical record by one investigator (KW). EVD placement was identified in medical records utilizing billing codes (ie, Current Procedural Terminology–CPT; International Classification of Disease, Ninth Revision–ICD-9; and International Classification of Disease, Tenth Revision Procedure Coding System–ICD-10-PCS) for procedures associated with ventricular drainage via EVD that occurred during the study period. Individual charts were then reviewed to confirm the placement of an EVD and to exclude patients who had other CSF drainage procedures or miscoded procedures. Inclusion was not limited by age, sex, or indication for EVD placement. We applied the following exclusion criteria: EVD placement as part of treatment for an active CSF infection, EVD dwell time <24 hours, and pregnancy. In total, 479 EVDs placed in 409 patients were included in this study.
Our primary outcome was development of an EVD infection following EVD placement. The Center for Disease Control and Prevention National Healthcare Safety Network (CDC NHSN) has not defined EVD infections. For this study, we used the CDC NHSN definition of meningitis/ventriculitis 31 in patients with an EVD in situ or within 30 days of EVD removal. Secondary outcomes included EVD duration, need for EVD flushing, CSF leak, dehiscence of surgical site, total number of EVDs placed per patient, 30-day functional outcome via modified Rankin Scale (mRS) score, and total length of hospital stay. Other collected variables included age, sex, GCS at insertion, indication for insertion, comorbidities, history of brain surgery including prior EVD placement, and site of EVD placement. For patients who developed an EVD infection, additional data were collected on microbial culture results, initial and final choice of antimicrobial therapy, antimicrobial treatment duration, and number of days after insertion when EVD infection occurred.
Treatment, procedural management, and infection control protocol
Indications for EVD placement in this patient cohort included subarachnoid hemorrhage (SAH), intracerebral hemorrhage (ICH), intraventricular hemorrhage (IVH), epidural hematoma (EDH), subdural hematoma (SDH), severe traumatic brain injury (TBI), obstructive hydrocephalus, space-occupying lesion, arteriovenous malformation, or shunt failure. EVD insertions were performed at the bedside or in the operating room. No antibiotic prophylaxis was given to the patient before the procedure or while the EVD was in place. Indications for sampling CSF from an implanted EVD were clinical or imaging suspicion of CNS infection or persistent fever. Routine sampling of CSF was not performed. The insertion site of an indwelling EVD was cleaned daily with alcoholic chlorhexidine and inspected for signs of dehiscence, CSF leak, or infection.
EVDs placed in our institution were predominantly non–antimicrobial-impregnated devices (Codman EDS3, Integra LifeSciences; Princeton, NJ). Antimicrobial-impregnated EVDs were reserved for patients with high suspicion of active CSF infection at the time of EVD placement and were thus excluded from this study.
Statistical analysis
Data were anonymized and exported to Microsoft Excel (Microsoft, Redmond, WA). Missing variables were assessed, and duplicate entries were removed. Continuous variables with normal and nonnormal distributions were represented as mean (± standard deviation, SD) and median (± interquartile range, IQR) respectively. Categorical data were represented as proportions with percentages. Statistical significance of comparisons between data was determined using the independent sample t test between mean values; using the nonparametric Kruskall-Wallis equality-of-populations rank test between median values; and using the χ2 test or the Fisher exact test, as appropriate, between categorical data. Cox regression analysis was conducted to determine hazard ratios and contribution of independent risk factors to EVD infection risk. P < .05 was considered significant. Data analysis was conducted using Statistical Package for Social Sciences (SPSS) version 24 software (IBM, Armonk, NY) and MedCalc version 19.4 software (MedCalc Software, Belgium).
Results
Overall, 479 EVDs inserted in 409 patients for 3,888 EVD days were included for analysis (Fig. 1). We observed a similar distribution of sex for patients receiving EVDs, with 55% males, 45% females, an age range of 18 days to 94 years, and a median age of 54 years (Table 1). Most EVD insertions involved patients with SAH (n = 145, 30%), ICH or IVH (n = 112, 23%), and severe TBI including EDH/SDH (n = 110, 23%). At the time of EVD insertion, patients had a median GCS of 7 (IQR, 3–13); 81% were intubated. Moreover, 9 EVD infections occurred in 9 patients, for an overall infection rate of 2.2% (2.3 infections per 1,000 EVD days).

Fig. 1. Selection for study Inclusion. Overall, 40 EVD records across 16 patients did not meet the inclusion criteria for analysis due to pre-existing CSF infection (29 EVDs, 9 patients) or EVD duration <24 hours (11 EVDs, 7 patients). Arrows indicate steps in selection process.
Table 1. Patient Demographics

Note. SD, standard deviation; NS, not significant; CSF, cerebrospinal fluid; GCS, Glasgow coma scale; SAH, subarachnoid hemorrhage; ICH, intracranial hemorrhage; IVH, intraventricular hemorrhage; TBI, traumatic brain injury; EDH, epidural hemorrhage; SDH, subdural hemorrhage; HCP, hydrocephalus; VP, ventriculo-peritoneal; MRSA, methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant Enterococcus species; CNS, central nervous system; AVM, arteriovenous malformation.
a History of CNS infection, but no active infection at time of EVD insertion.
*P < .05
Effect of comorbidities on EVD infection risk
In total, 10 EVDs (2.1%) were placed in immunocompromised patients (ie, absolute neutrophil count <500/mm3 and/or the use of 1 or more immunosuppressive medications). Also, 5 EVDs (1.0%) were placed in patients with type I diabetes mellitus, and 35 (7.3%) were placed in patients with type II diabetes mellitus. Although the presence of active CNS infection was an exclusion criterion, 9 EVDs (1.9%) were inserted in patients with a history of resolved CNS infection. None of these patients developed an EVD infection (Table 1).
EVDs placed in patients with a history of prior brain surgery was associated with an increased risk for EVD infection (OR, 7.8; 95% CI, 1.6–37.8; P = .0097), independent of the specific indication for brain surgery (Table 1). When further stratified by prior brain surgeries with and without concurrent or previous shunt or EVD placement, only surgeries with prior EVD or shunt placement were associated with higher EVD infection risk (OR, 5.7; 95% CI, 1.5–21.7; P = .011).
Effect of operative variables on EVD infection risk
Most EVDs were placed in the neurocritical care unit (NCCU; n = 268, 56%) and emergency department (n = 109, 23%) (Table 2). All 9 EVD infections occurred in the NCCU while the EVD was in place (P = .0056). The median EVD day-of-infection diagnosis was 4 days (minimum 2, maximum 11; IQR, 2–7). Most EVDs were placed by neurosurgery residents, most commonly by junior residents (n = 217, 45%). The overwhelming majority of catheters were inserted frontally at the Kocher point (n = 455; 366 right-sided and 89 left-sided). Risk of EVD infection was not influenced by training level of the primary surgeon, anatomic site of EVD insertion, total EVD indwelling time, or number of EVDs per patient.
Table 2. Operative Statistics
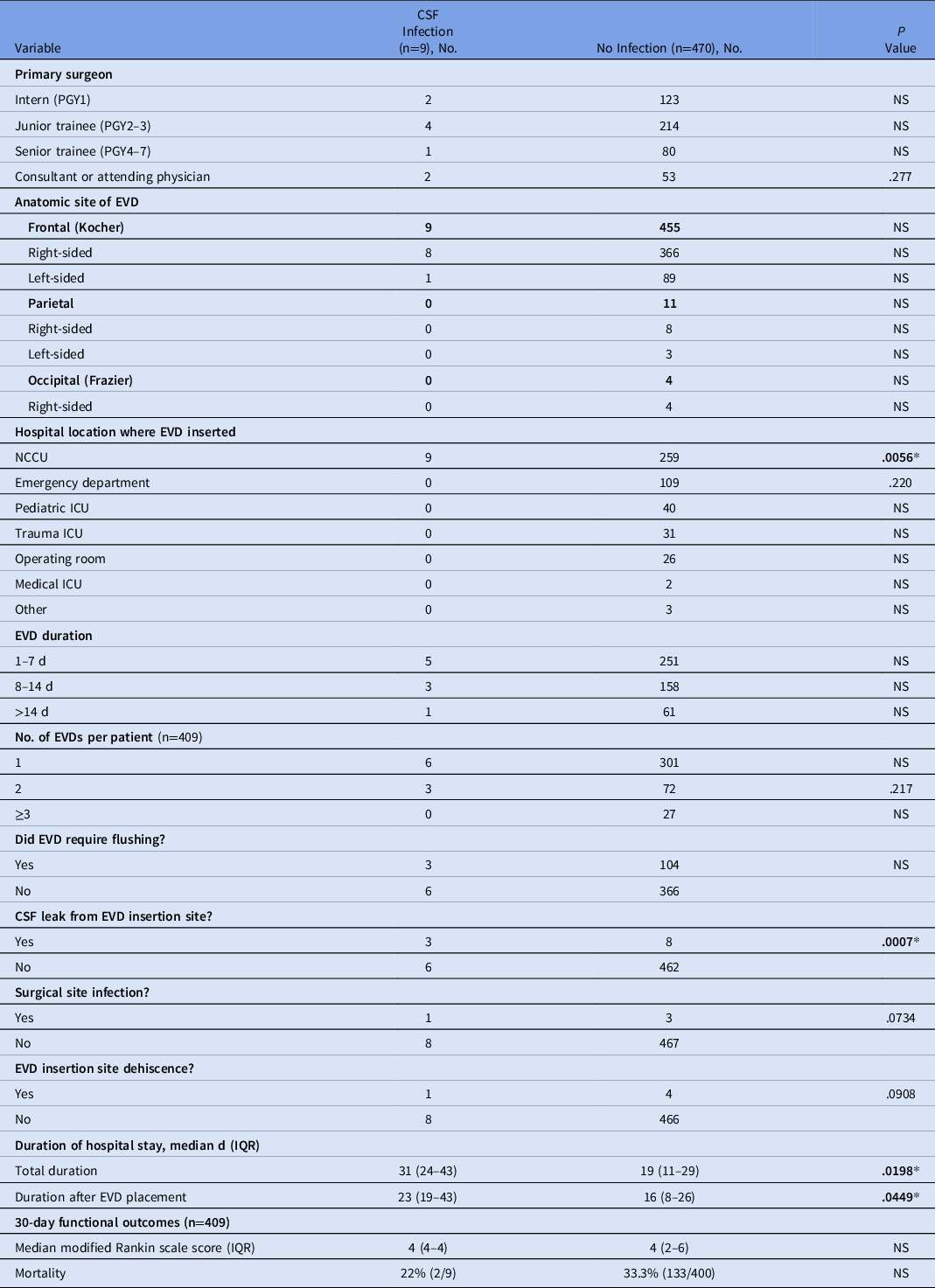
Note. CSF, cerebrospinal fluid; PGY, postgraduate year; EVD, external ventricular drain; NCCU, neurocritical care unit; ICU, intensive care unit; IQR, interquartile range.
P values calculated using χ2 goodness of fit or Fisher exact test.
*P < .05.
EVD infection risk factors
EVD infection was associated with prolonged post–EVD-placement length of stay (23 days vs 16 days; P = .045). Upon development of an EVD infection, the device was weaned and removed promptly. If the patient continued to require CSF diversion, it was replaced with an antibiotic-impregnated catheter. Median length of treatment with antibiotics after diagnosis of EVD infection was 14 days (minimum 10, maximum 42; IQR, 14–28). The most common pathogens associated with these infections were coagulase-negative staphylococci (Table 3). Two cases were polymicrobial: one case involving Micrococcus luteus and Pantoea agglomerans, the other involving coagulase-negative staphylococci and Cutibacterium acnes.
Table 3. Outcomes of EVD Infections
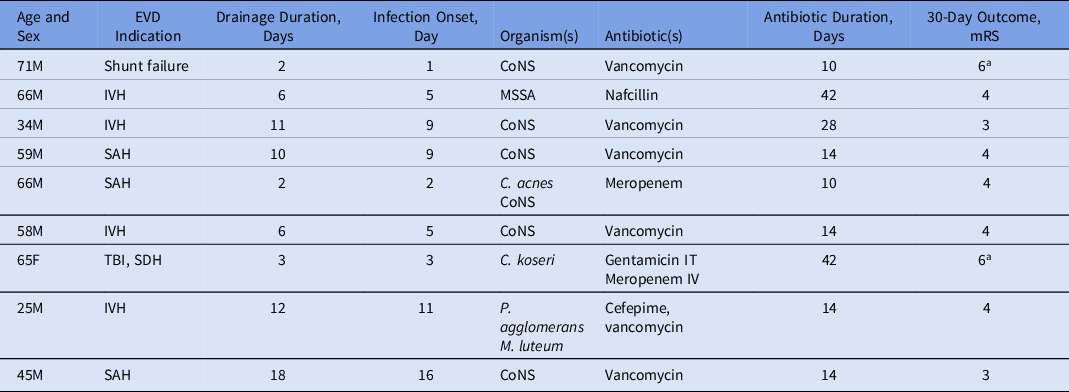
Note. EVD, external ventricular drain; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage; TBI, traumatic brain injury; SDH, subdural hematoma; CoNS, coagulase-negative staphylococci; MSSA, methicillin-sensitive Staphylococcus aureus; C. acnes, Cutibacterium acnes; C. koseri, Citrobacter koseri; P. agglomerans, Pantoea agglomerans; M. luteus, Micrococcus luteum; IT, intrathecal; IV, intravenous; mRS, modified Rankin Scale score (3=moderate disability, 4=severe disability, 6=death).
a Pateint died.
Cox regression analysis adjusted for age, sex, and indication for EVD placement demonstrated increased infection risk associated with prior brain surgery involving EVD or shunt placement (HR, 8.08; 95% CI, 1.7–39.4; P = .010), development of a postoperative CSF leak (HR, 21.0; 95% CI, 7.0–145.1; P = .0007), and dehiscence of surgical site (HR, 7.53; 95% CI, 1.04–37.1; P = .0407). Duration of EVD placement >7 days was not associated with infection risk (HR, 0.62; 95% CI, 0.07–5.45; P = .669).
Mortality and functional outcomes
In total, 135 (33%) deaths were observed within 30 days after EVD insertion. Of the 274 patients surviving at 30 days following EVD insertion, 48 (18%) were lost to follow-up, 134 (49%) had good functional outcomes (mRS, 0–2), and 92 (34%) had poor functional outcomes (mRS, 3–5). We detected no significant difference in mortality or mRS in patients with EVD infection when compared to those without EVD infection. Of the 2 patients with EVD infection who died, one death was due to complications of infection and the other was due to complications of shunt failure (Table 3).
Discussion
Previously identified risk factors for EVD infection include prolonged EVD dwell time, prior surgery, CSF leak, frequency of CSF sampling and EVD manipulation, insufficient tunneling of the EVD catheter, tract hemorrhage at placement, and insufficient hair clipping. Reference Fried, Nathan and Rowe1–Reference Flint, Toossi and Chan6,Reference Phan, Schultz and Huang8–Reference Rahman, Whiting and Fauerbach20,Reference Hader and Steinbok22,Reference Hepburn-Smith, Dynkevich and Spektor23,Reference Trick, Kioski and Howard25,32–Reference Collins, Hartley, Chakraborty and Thompson34 Previous brain surgery has been demonstrated to be an independent risk factor for EVD infection. Reference Lozier, Sciacca, Romagnoli and Connolly2,Reference Muralidharan3,Reference Kim, Lee and Feng5,Reference Flint, Toossi and Chan6,Reference Phan, Schultz and Huang8,Reference Dasic, Hanna, Bojanic and Kerr15,Reference Bota, Lefranc and Vilallobos16,Reference Lyke, Obasanjo and Williams18,Reference Mayhall and Archer19 Our findings support these reports. Stratification by type of surgery revealed that this increased risk was specifically related to cranial surgeries with EVD or shunt placement concurrently with or before the surgery. To our knowledge, this has not been previously noted in the literature.
Prolonged EVD duration is associated with an increased risk of EVD-related infection. Reference Lozier, Sciacca, Romagnoli and Connolly2,Reference Muralidharan3,Reference Kim, Lee and Feng5,Reference dos Santos, Fortes Lima, Lunardi and Stefani9,Reference Kim, Desai and Ricci12–Reference Hoefnagel, Dammers, Ter Laak-Poort and Avezaat14,Reference Bota, Lefranc and Vilallobos16–Reference Mayhall and Archer19,Reference Trick, Kioski and Howard25,32,Reference Zhou, Wu, Chen and Zhao33 Surprisingly, we did not find this to be the case. Most infections we observed occurred within 1–7 days of EVD insertion. Prolonged EVD dwell time was associated with a nonsignificant decrease in incidence of EVD infections (2.0% risk for 1–7 days, 1.9% risk for 8–14 days, 1.6% risk for >14 days). We hypothesize that this unexpected result is due to several longstanding, evidence-based infection control protocols in place at our institution, including minimal catheter manipulation after insertion, no routine CSF sampling, and regular cleansing of the insertion site with alcoholic chlorhexidine. Reference Fried, Nathan and Rowe1–Reference Muralidharan3,Reference Kubilay, Amini and Fauerbach10,Reference Hoefnagel, Dammers, Ter Laak-Poort and Avezaat14–Reference Rahman, Whiting and Fauerbach20,Reference Hader and Steinbok22,Reference Walek, Leary, Sastry, Asaad, Walsh and Mermel30
Other known risk factors associated with EVD infection include CSF leak, frequency of CSF sampling, and EVD manipulation. Reference Fried, Nathan and Rowe1,Reference Muralidharan3,Reference Kim, Lee and Feng5,Reference Camacho, Boszczowski and Freire11,Reference Kitchen, Singh and Hulme13–Reference Dasic, Hanna, Bojanic and Kerr15,Reference Korinek, Reina and Boch17–Reference Mayhall and Archer19 Although our institution has not routinely sampled CSF without suspicion of infection since 2008, analysis of this cohort identified a dramatically increased risk of infection with CSF leak. Indeed, CSF leak was the strongest risk factor identified in our study; although CSF leakage around the insertion site occurred in only 11 EVDs, 3 of these EVDs subsequently became infected. CSF leak has consistently been identified as a major contributor to the risk of EVD infection, and our findings further emphasize the importance of careful surgical technique during EVD catheter placement to ensure watertight wound closure and a tight seal around the catheter to mitigate risk of CSF leak and subsequent EVD infection.
Several prior studies have demonstrated SAH and IVH as independent risk factors for EVD infection. Reference Lozier, Sciacca, Romagnoli and Connolly2,Reference Kim, Lee and Feng5,Reference dos Santos, Fortes Lima, Lunardi and Stefani9,Reference Kim, Desai and Ricci12,Reference Trick, Kioski and Howard25 Of 9 EVD infections we identified, 3 occurred in patients with SAH and 4 in patients with ICH or IVH. However, these 2 indications for EVD placement comprised most cases requiring EVD insertion in our study, and the incidende of infection was not significantly higher in either group.
As demonstrated in previous studies, the most common pathogens associated with EVD infections are coagulase-negative staphylococci. Reference Kim, Lee and Feng5–Reference Phan, Schultz and Huang8,Reference Kubilay, Amini and Fauerbach10–Reference Kim, Desai and Ricci12,Reference Hoefnagel, Dammers, Ter Laak-Poort and Avezaat14–Reference Korinek, Reina and Boch17,Reference Mayhall and Archer19,Reference Hader and Steinbok22,32,Reference Zhou, Wu, Chen and Zhao33 Other common pathogens include Staphylococcus aureus, Cutibacterium acnes, and Citrobacter koseri, Reference Kim, Lee and Feng5,Reference Talibi, Tarnaris and Shaw7,Reference Phan, Schultz and Huang8,Reference Kubilay, Amini and Fauerbach10–Reference Kim, Desai and Ricci12,Reference Hoefnagel, Dammers, Ter Laak-Poort and Avezaat14–Reference Mayhall and Archer19,Reference Hader and Steinbok22,32,Reference Zhou, Wu, Chen and Zhao33 and infections with these pathogens were identified in our study patients.
Comparison to incidence and mortality in other reported studies
Our overall infection rate was 2.2% and the incidence density was 2.3 infections per 1,000 EVD days which compares favorably with prior studies, Reference Fried, Nathan and Rowe1,Reference Lozier, Sciacca, Romagnoli and Connolly2,Reference Kim, Lee and Feng5–Reference Mayhall and Archer19,Reference Hader and Steinbok22,Reference Moussa and Mohamed24,Reference Zhou, Wu, Chen and Zhao33 including those that also used the CDC NHSN surveillance definition of meningitis/ventriculitis (Table 4). Reference Kim, Lee and Feng5–Reference Mayhall and Archer19 Additionally, our infection rate is comparable to, and in some cases lower than, institutions using post-EVD antibiotic prophylaxis and antimicrobial-impregnated EVDs. Reference Sheppard, Ong and Lagman21,Reference Moussa and Mohamed24,Reference Wang, Dong and Qi26–Reference Wong, Ip and Poon29,Reference Sorinola, Buki, Sandor and Czeiter35–Reference Hong, Apedjinou and Heissler39 Based on a previous analysis of the effects of protocol changes at our institution, Reference Walek, Leary, Sastry, Asaad, Walsh and Mermel30 we believe major factors that have contributed to this low infection rate include cutaneous antisepsis with alcoholic chlorhexidine, elimination of routine CSF sampling, and use of a modified tunneling technique with coiling of the catheter under the skin. We have demonstrated that EVD catheters can remain in place without contributing to EVD infection risk as long as meticulously sterile technique is used with minimal device manipulation.
Table 4. Incidence and Risk Factors Associated With EVD Infection in Previous Literature
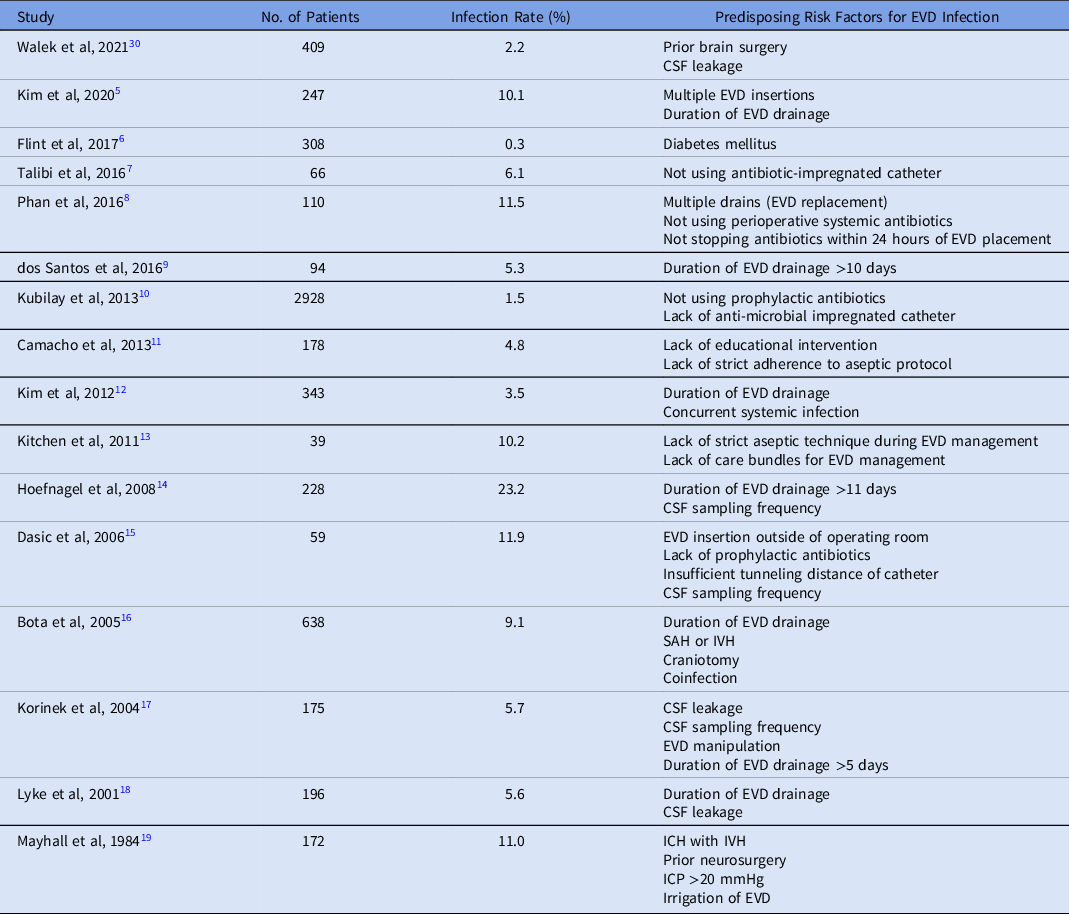
Note. EVD, external ventricular drain; CSF, cerebrospinal fluid; SAH, subarachnoid hemorrhage; IVH, intraventricular hemorrhage; ICH, intracranial hemorrhage; ICP, intracranial pressure.
Of the 9 patients who experienced an EVD infection during our study period, 2 died within 30 days of EVD placement, conferring a 30-day mortality rate of 22%. This finding is consistent with previously reported 30-day mortality rates of 17%–46%. Reference Kim, Lee and Feng5,Reference dos Santos, Fortes Lima, Lunardi and Stefani9,Reference Camacho, Boszczowski and Freire11,Reference Kim, Desai and Ricci12,Reference Bota, Lefranc and Vilallobos16,Reference Mayhall and Archer19
This study had several limitations. The retrospective nature of this study leaves open the possibility of incomplete data in the medical records. However, microbiological reports were always available. Routine CSF cell counts and CSF lactate levels were not obtained throughout the course of the study; therefore, no conclusions can be drawn as to their ability to help predict or aid in the diagnosis of CSF infection associated with EVD placement. We also did not collect data on which provider manipulated the EVD once it was placed, and the number of insertion attempts per EVD was not routinely recorded. Our study may have been underpowered to identify all significant risk factors in this cohort.
In conclusion, risk of EVD infection was associated with prior brain surgery associated with EVD or shunt placement, CSF leak, and insertion site dehiscence. We did not find an association between infection risk and prolonged duration of EVD placement, which might be attributable to our institutional policies of minimal EVD manipulation after insertion, no routine CSF sampling, and regular cleansing of the insertion site with alcoholic chlorhexidine.
Acknowledgments
The authors thank the Rhode Island Hospital infection control staff for their thoughtful assistance in mitigating EVD infection risk and managing data related to this project. The authors declare no conflicts of interest, and this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.








