The National Action Plan for Combating Antibiotic-Resistant Bacteria aimed to reduce inappropriate outpatient antibiotic use by 50% by 2020, which emphasized in the updated plan for 2020. 1 Studies have identified respiratory infections and sinusitis as specific improvement targets by reducing inappropriate antibiotic starts and optimizing antibiotic selection and duration. Reference Martinez, Rood, Jhangiani, Kou, Boissy and Rothberg2,Reference Hersh, Fleming-Dutra, Shapiro, Hyun and Hicks3 For example, macrolides and fluoroquinolones are often inappropriately prescribed for sinusitis when either no antibiotic is indicated or a narrow-spectrum antibiotic is preferred. Reference Hersh, Fleming-Dutra, Shapiro, Hyun and Hicks3,Reference Chow, Benninger and Brook4
E-visits, defined as a mode of asynchronous care delivery through a secure patient portal for minor acute illnesses, have recently increased in use. E-visits have the ability to improve access to care, to decrease healthcare costs, and to improve patient satisfaction. Reference Penza, Murray, Pecina, Myers and Furst5 E-visits do not allow for 2-way communication between patient and provider, in comparison to “video visits” where patient and provider are able to interact in real-time through secure audiovisual conferencing platforms. In addition to the increasing interest driven by patient preferences and technological advances, the coronavirus disease 2019 (COVID-19) pandemic has created a need for more virtual care to decrease exposure. Currently, data on the effectiveness of implementing an antibiotic stewardship intervention to improve antibiotic prescribing within E-visits are limited. Due to high rates of inappropriate antibiotic use for upper respiratory tract infections (URTIs), we aimed to implement a multifaceted intervention to improve guideline-concordant antibiotic use associated with E-visits for sinus, cough, or flu symptoms.
Materials and methods
All adult patients who completed an E-visit for “cough,” “flu,” or “sinus symptoms” at Michigan Medicine between January 1, 2018, and September 30, 2020, were included. The E-visit is a patient-initiated request for care based on a primary symptom, in which the patient electronically completes and submits a questionnaire related to the symptom of concern from a prepopulated list. These responses are then reviewed by an advanced practice provider (APP) who responds with a written treatment plan within 24 hours. Patients with high-risk characteristics (eg, immunocompromised hosts, symptoms concerning for more complex or emergent condition) are referred for a visit with their primary care physician instead. Based on the primary symptom, patients filled out a questionnaire for “cough,” “flu,” or “sinus symptoms.”
Our intervention included the modification of the existing questionnaire to support gathering pertinent information to assess guideline-concordant diagnoses and the creation of computer support tools that generate therapy plans which provide nudges for guideline-concordant prescribing (ie, a phrase template with preselected options for antibiotic selection and duration in order of preference) (Supplement 1 online). In addition, in the months prior to roll out of the intervention, the antimicrobial stewardship committee developed evidence-based sinusitis guidelines and presented them along with the upcoming changes to the electronic medical record (EMR) to the APPs in December 2018. In January 2019, these new EMR tools were launched and were integrated into the electronic record (Supplementary Appendices 1 and 2 online). An additional intervention, implemented in March 2019 and ending in May 2019, involved 2 primary-care physician champions who reviewed antibiotic prescribing rates associated with E-visits in real time and provided audit and feedback to the APPs regarding their selection and duration of antibiotics, the percentage of visits for which they prescribed antibiotics, and guideline concordance. The physician champions were the authorizing providers for the APP team and had regular contact with the APPs during the intervention. The preimplementation period was defined as January 1, 2018, through December 31, 2018. The postimplementation period started June 1, 2019.
Data collected from the EMR included E-visit encounter type (reflected by patient symptom), age, comorbidities, medications, allergies, International Classification of Disease, Tenth Revision (ICD-10) diagnosis code(s), type of antibiotic prescribed and antibiotic duration. Ethics approval was obtained by the Institutional Review Board of the University of Michigan (no. HUM00194065).
An antibiotic prescribed for a visit with an ICD-10 diagnosis code that did not require antibiotics was considered inappropriate (eg, bronchitis) (Supplementary Appendix 3 online). Guideline-concordant antibiotic prescribing for sinusitis included amoxicillin-clavulanate or doxycycline prescribed for 5–7 days. Reference Chow, Benninger and Brook4
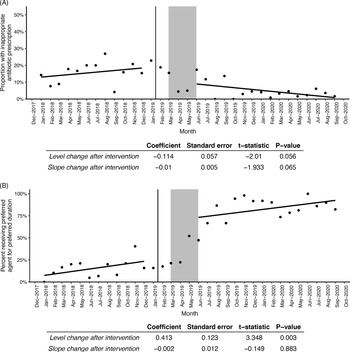
We performed segmented linear regression to estimate the effect of the intervention on the level and trend of (1) the proportion of patients with an ICD-10 diagnosis code that did not require antibiotics who received an inappropriate antibiotic over time, and (2) the proportion of patients who received guideline-concordant antibiotic selection and duration for sinusitis. Regression lines were fit to data before the intervention period (prior to January 2019 and after the intervention period (after May 2019).
Results
Between January 1, 2018, and September 30, 2020, we identified 5,151 E-visits for “cough,” “flu,” or “sinusitis” for inclusion in our study (Table 1). The average age preintervention was 49 years, and the average age postintervention, which includes data from the COVID-19 pandemic, was 44 years. Before the intervention, 26.7% of E-visits were for male patients and after the intervention 30.2% of E-visits were for male patients. Prior to the intervention, 43.2% of visits resulted in antibiotic prescriptions compared to 28.9% of postintervention visits, which was a significant decrease (P < .001). The number of antibiotic prescriptions for guideline-concordant antibiotic selection increased from 37.9% (amoxicillin-clavulanate) and 13.8% (doxycycline) to 66.1% (amoxicillin-clavulanate, P < .001) and 22.7% (doxycycline, P < .001). The median duration of antibiotics decreased from 10 days to 5 days (P < .001). Importantly, follow-up visits with a primary care provider or the emergency department where the antibiotics were prescribed within 14 days of the E-visit decreased after the intervention from 4.5% to 2.9% (P = .02).
Table 1. Demographics and Results

Note. PCP, primary care provider; ER, emergency room. Bold indicates statistical significance.
a 1978 E visits in March and April 2020 alone.
c Phased out March 1, 2018.
d T test.
e Wilcoxon rank-sum test.
The interrupted time series demonstrated the proportion of inappropriate antibiotic prescriptions (Fig. 1A) as a function of time, as well as the proportion of patients receiving guideline-concordant antibiotics for sinusitis (Fig. 1B). The rate of inappropriate prescriptions dropped and began to decrease over time following the intervention; however, neither change in level nor trend reached statistical significance. Prescribing guideline-concordant antibiotics increased significantly after the intervention (P = .003) and continued along a similar upward trend compared to the trend prior to the intervention.

Fig. 1. (A) Interrupted time series model predicting proportion of patients with an antibiotic prescription for an ICD-10 diagnosis code that did not require antibiotics (“inappropriate prescriptions”) by time before and after the bundled intervention. (B) Interrupted time series model predicting proportion receiving preferred agent for the preferred duration for sinusitis from “sinusitis” E visits by time before and after the bundled intervention. Solid vertical line at January 16, 2019, represents the launch of new questionnaires and templates in the electronic medical record, and the gray box between March 1, 2019, and May 31, 2019, represents the physician-champion intervention.
Discussion
A multifaceted stewardship intervention for E-visits was associated with improved guideline-concordant prescribing for sinusitis and decreased inappropriate antibiotic prescriptions for URTIs. Given the bundled approach over a single period, it was difficult to discern most impactful contributions, which was a limitation of the study. Based on the significance and rapidity of change following the physician-champion feedback, we suspect that this element of the bundle was high-yield in influencing the change in prescribing demonstrated by our study. Prior studies have also demonstrated the value of direct feedback to prescribers from antimicrobial stewardship teams. Reference Huang, Newton and Kunapuli11,Reference Camins, King and Wells12
Baseline prescribing rates in this study are similar to those of other studies, including an antibiotic prescribing rate of ∼70% for sinusitis Reference Fairlie, Shapiro, Hersh and Hicks6 and an antibiotic prescribing rate of ∼15% for “antibiotic never appropriate” indications. Reference Fleming-Dutra, Hersh and Shapiro7,Reference Liu, Kaye and Mercuro8 Other studies have demonstrated that E-visits have higher rates of guideline-concordant antibiotic prescribing than office visits, because the current guidelines were included for review at the time of the E-visit. Reference Johnson, Dumkow, Burns, Yee and Egwuatu9,Reference Johnson, Dumkow, Salvati, Johnson, Yee and Egwuatu10 Previously, E-visits for sinusitis have been associated with guideline-concordant antibiotic use 65% of the time Reference Johnson, Dumkow, Burns, Yee and Egwuatu9 compared to 50% in office visits. Reference Hersh, Fleming-Dutra, Shapiro, Hyun and Hicks3 Our study demonstrates significant improvement in guideline-concordant antibiotic prescribing in E-visits following a multifaceted stewardship intervention to 93%, better than office visits or E-visits previously described.
This study had several limitations. It included an increase in the number of E-visits in the postintervention period due to the COVID-19 pandemic, which included new providers who had not received the interventions. Specifically in March and April 2020, our health system as well as the state of Michigan strongly encouraged virtual care as first-line treatment for all complaints, with drastically reduced in-person clinic visits. There were 3,562 E-visits in the entire postintervention period, and 1,978 of those E-visits occurred in March and April 2020. Ultimately, we would have expected this factor to decrease the impact of the intervention. The fact that it did not emphasizes the sustainability of the interventions. Although our study was not designed to specifically address changes wrought by the COVID-19 pandemic, the months with the largest influx of E-visits into our system (March and April 2020) did not show appreciably higher rates of inappropriate antibiotic prescribing (Fig. 1A) or decreases in guideline concordance (Fig. 1B). In addition, ICD-10 codes themselves represent a limitation. The accuracy of diagnoses was not assessed, so antibiotic use, though guideline concordant, may still represent overuse for sinusitis.
Our study also had several strengths. First, it included a large cohort, which allowed us to assess the impact of the intervention. Second, we linked the antibiotic prescription to a diagnosis code for the E-visit, which increased the validity of the data. Third, the use of an interrupted time series analysis allowed us to assess the sustainability of improved antibiotic prescribing for sinusitis after cessation of the physician audit and feedback intervention.
In conclusion, a multifaceted stewardship bundle for E-visits including questionnaire modification, creation of prepopulated EMR nudges and shortcuts, and direct audit and feedback, improved guideline-concordant antibiotic prescribing for URTIs. Changes implemented in the EMR are likely most beneficial after a period of audit and feedback. This approach can aid stewardship efforts in the ambulatory care setting with increases in telemedicine.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2022.19
Acknowledgments
The content of this publication does not necessarily reflect the official views or policies of the Department of Health and Human Services nor does the mention of trade names, commercial products, or organizations imply endorsement by the US government.
Financial support
This work was funded in part with federal funds by the National Institute of Allergy and Infectious Diseases (grant no. K01 AI141579 to J.G.P.).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.