Since the report of the first US case in Snohomish County, Washington, on January 19, 2020, COVID-19 has spread quickly nationwide. Reference Holshue, DeBolt and Lindquist1 As of January 14, 2022, >64 million cases had been confirmed, and >850,000 related deaths had been reported in the United States. 2 Residents of long-term care facilities account for <1% of the US population, but they contributed 10% of COVID-19 cases and 37% of all deaths. 3
Facility-level characteristics, area-level socioeconomic deprivation, and state social distancing policies are associated with COVID-19 cases and deaths in nursing homes. Reference Grabowski and Mor4–Reference Li, Cheng, Cai, Mao and Temkin-Greener7 Residents of nursing homes are typically older, have multiple chronic conditions, and live in communal settings, making them more vulnerable to the ravages of this pandemic. Reference Grabowski and Mor4,Reference Thompson, Barbu and Beiu5 The risks of COVID-19 and death are higher among nursing home minority residents, Reference Li, Cen, Cai and Temkin-Greener6 suggesting unequal access to resources and greater exposure to infection. Neighborhood socioeconomic status, including racial/composition of a community, Reference Cai, Yan and Intrator8,Reference Elkafrawi, Sisti and Mercado9 per-capita income, Reference Sugg, Spaulding and Lane10 housing conditions, Reference Wong, Upchurch, Steers, Haderlein, Yuan and Washington11,Reference De Jesus, Ramachandra and Jafflin12 and the general neighborhood deprivation Reference Fritz, Ramsey and Taylor13–Reference Das, Ghosh, Das, Basu, Das and Dutta15 are also potential risk factors.
In response to the COVID-19 pandemic, states adopted different policies and imposed measures to control its spread. Examples include social distancing, mask mandates, business closures, and mandatary quarantines. Studies have suggested that these measures were effective in slowing the overall impact of COVID-19 in various settings, including in nursing homes. Reference Li, Cheng, Cai, Mao and Temkin-Greener7,Reference Lyu and Wehby16,Reference Lyu and Wehby17
Assisted living communities (ALCs) account for half of all long-term care beds in the United States, and they serve older and more disabled populations than nursing homes. Reference Caffrey, Sengupta and Melekin18,Reference Silver, Grabowski, Gozalo, Dosa and Thomas19 However, the impact of the COVID-19 pandemic on these communities has received very little attention. Reference Temkin-Greener, Guo, Mao, Cai and Li20 To date, no study has examined how the current pandemic has affected ALCs and their residents, particularly those who live in ALCs with fewer resources (ie, with a higher proportion of minority or dually eligible residents) or in ALCs located in more disadvantaged neighborhoods. Furthermore, the impact of state COVID-19 social-distancing policies and their stringency on COVID-19 case penetration in ALCs has not been examined.
ALCs share many similar characteristics with nursing homes, and possibly they have faced similar problems during the pandemic. Reference Zimmerman, Carder and Schwartz21 Understanding factors that may modify the pandemic’s impact in this residential setting is important in developing effective prevention policies. To fill the gaps in the literature, we examined the association of ALC-level COVID-19 cases with facility, community, and state-level factors.
We hypothesized that ALCs with fewer resources (ie, proxied by higher proportions of racial/ethnic minority and dually eligible Medicare/Medicaid residents), ALCs located in communities with higher area deprivation index, and ALCs in states with less stringent COVID-19 social distancing measures experienced higher numbers of COVID-19 cases than ALCs with higher resource availability, in wealthier communities, and in states with stricter policies.
Methods
Data
We used multiple sources of data. The information on weekly reported COVID-19 cases was obtained from state health department websites. As of June 2020, 12 states were reporting ALC-specific COVID-19 cases online. Due to differences in data quality, we kept only 5 states (Colorado, Connecticut, Georgia, Ohio, and South Carolina) in our final analytical sample. Other states were excluded because they reported ranges of cases rather than actual case counts (Massachusetts and Rhode Island), because they reported only new but not cumulative cases (North Dakota and Florida), because they masked data in ALCs with fewer than 5 cases (Pennsylvania and North Carolina), and becuase they reported only a disproportionately small number of COVID-19 cases (Kentucky).
A national inventory of ALCs that we previously constructed based on data obtained from state licensing agencies was linked to the COVID-19 state reports using facility names and addresses. Reference Temkin-Greener, Mao, Ladwig, Cai, Zimmerman and Li22 Employing a previously developed methodology, Reference Temkin-Greener, Mao, Li and McGarry23 we identified Medicare beneficiaries who resided in ALCs in calendar year 2018 (CY2018). We then used the Master Beneficiary Summary File (MBSF) to characterize ALCs based on the following factors: average resident age, proportion of race and ethnic minorities and the dual-eligible status for Medicare and Medicaid, proportion of males, and residents with chronic conditions. Data regarding the area deprivation index (ADI) at the census-tract level were obtained from Neighborhood Atlas Project of CY2018, which is maintained by the University of Wisconsin. Reference Kind and Buckingham24,25 ADI ranks neighborhoods by socioeconomic disadvantage status based on factors such as income, education, employment, and housing quality. Reference Kind and Buckingham24 Previous research has shown that ADI is a valid measure in identifying socially disadvantaged neighborhoods. Reference Sheehy, Powell and Kaiksow26,Reference Rahman, Meyers and Wright27
Data on state-level COVID-19 policy stringency were obtained from the Wallethub.com website. 28 This website has been publishing COVID-19 policy stringency rankings for all 50 states every 2 weeks since May 2020. The rankings are based on 13 metrics: mask mandates, travel restrictions, restrictions on gatherings, school closure, reopening of restaurants and bars, state guidance on customer health checks at restaurants, reopening of nonessential business, legislation on business immunity from COVID-19 claims, working from home requirements, workplace temperature screening, strictness of the “shelter in place” order, presence of multistate agreements to reopen, and guidance for ALCs related to COVID-19. 28 Each metric was graded by a panel of public health experts on a 100-point scale, with higher scores denoting fewer restrictions. The weighted average score of all domains was then calculated and aggregated to produce policy stringency rankings for all 50 states. We acquired the policy stringency data for 5 consecutive weekly updates: June 9, June 23, July 7, July 21, and August 11. Assuming a 1-week lag of policy effect on cases, we linked the state-level policy stringency data to the ALC-level COVID-19 weekly reports by state. That is, stringency data from June 9 were linked to cases data for the week of June 16, whereas stringency data from August 11 were linked to the cases data for the week of August 18. The rationale for a 1-week policy lag was based on the finding that the estimated median incubation period of COVID-19 was 5.1 days. Reference Lauer, Grantz and Bi29
County-level COVID-19 cases were acquired from The New York Times COVID-19 data set (https://github.com/nytimes/covid-19-data). The information on county-level population density was derived from Area Health Resources Files (AHRF) CY2018 maintained by the Health Resources & Services Administration. 30
Outcome variable
Our outcome of interest was the cumulative number of ALC-level COVID-19 cases each week. In accordance with the dates of state policy stringency data and the assumed 1-week lag, ALC-level COVID-19 cases in the weeks of June 17, June 30, July 14, July 28, and August 18 were included in the final analyses.
Key independent variables
The literature showed that ALCs with fewer resources were more likely to have higher proportion of residents who were dually eligible for Medicare and Medicaid, were smaller, and tended to have a higher proportion of racial and ethnic minority residents. Reference Zimmerman, Guo, Mao, Li and Temkin-Greener31 Therefore, we characterized ALCs based on both the proportion of race and ethnic minorities and dual status as the ALC-level key independent variable of interest. For each ALC, we calculated the proportion of residents who were minority (ie, black and/or Hispanic) and dually eligible. Because of the skewed distribution, we dichotomized this variable as 1 for ALCs with higher proportions of dually eligible minority residents, and 0 otherwise. We chose the third quartile as the cutoff point because almost half of the ALCs reported very low proportion of minority and dually eligible residents (median, 0; third quartile, 0.18).
The ADI was also dichotomized as 1 for ALCs located in more deprived areas and 0 for ALCs located in less deprived areas. The ADI ranged from 1 to 100. Following prior studies, Reference Sheehy, Powell and Kaiksow26,Reference Hu, Bartels, Rovin, Lamb, Kind and Race32 we chose the median value of 55 as the cutoff point. Using 9-digit ZIP codes, Reference Temkin-Greener, Mao, Li and McGarry23 we linked the ALCs to the most proximate ADIs.
State-level COVID-19 social-distancing policy stringency was a continuous variable ranking each of the 50 states, from the least (=1) to the most stringent (=50).
Other covariates
Additional ALC-level characteristics aggregated from the resident-level information of the MBSF included the following: average resident age, proportion of male residents (dichotomized using median value 0.50), bed size, and the proportions of residents with selected chronic conditions (ie, dementia, chronic obstructive pulmonary disease [COPD], asthma, congestive heart failure [CHF], obesity, hypertension, chronic kidney diseases, and diabetes).
Additional area-level covariate included metropolitan versus nonmetropolitan ALC location, which was derived using rural–urban continuum codes and Federal Information Processing Standard Publication codes of the ALCs. Fixed effects accounting for each study week were also included to adjust for the hierarchical nature of the data.
Analytical sample
Our sample included 2,952 ALCs with 1,624 reported COVID-19 cases (as of August 18, 2020). We deleted 98 ALCs, and their associated 110 COVID-19 cases, because we were not able to link these beneficiaries to the CY2018 MBSF. After applying all the exclusion criteria, we included 2,854 ALCs (96.68%) with 1,514 reported COVID-19 cases (93.22%) in the final analytical sample.
Statistical analyses
We first calculated the summary statistics for ALCs included in our sample, stratified by whether the ALC reported at least 1 COVID-19 case. Student t tests and χ2 tests were employed to compare the ALCs.
We then conducted multivariable analyses to examine the associations between the ALC-level proportion of minority and dually eligible residents, neighborhood ADI, state policy stringency, and the reported COVID-19 cases. To account for the large number of ALCs with zero cases, we applied a 2-part Poisson regression with the unit of analysis being each ALC per week. The first part of our model was a logistic regression estimating the likelihood of ALC having 1 or more reported COVID-19 cases in a study week. In the second part of our model, we used a generalized linear model, assuming a Poisson distribution of cumulative cases, conditional on the ALC having reported at least 1 case. In both models, we controlled for the same characteristics, and standard errors were clustered at the state level.
All analysis were performed using SAS version 9.4 software (SAS Institute, Cary, NC). This study was reviewed and approved by the University of Rochester Institutional Review Board.
Results
Descriptive analysis
In the 5 states we examined, 201 ALCs (7.04%) had reported 1 or more COVID-19 cases as of August 18, 2020 (Table 1). ALCs with COVID-19 cases, compared to those without, were more likely (P < .001) to have residents who were older (82.96 vs 74.38 years) or were male (28.29% vs 36.14%), to be larger in bed size (75.07 vs 37.62 beds), and to have a lower proportion of dually eligible minority residents (3.37% vs 12.74%). ALCs with COVID-19 cases also differed from those that reported none regarding the prevalence of chronic conditions, such as dementia (42.40% vs 29.85%; P < .001), COPD (29.70 vs 26.43%; P = .014), chronic heart failure (37.88% vs 27.22%; P < .001), hypertension (73.12% vs 64.80%; P < .001), and chronic kidney disease (12.36% vs 6.14%; P < .001).
Table 1. Assisted Living Communities (ALC), Neighborhood Area, and State Characteristics by Whether COVID-19 Cases Had Been Reported as of August 18, 2020

Note. SD, standard deviation; NA, not available; COPD, chronic obstructive pulmonary disease; CHF, chronic heart failure.
ALCs with COVID-19 cases were more likely to be located in communities with a higher ADI (63.18% vs 46.81%; P < .001) and to be in more metropolitan areas (89.05% vs 82.81%; P = .0223). State stringency ranking did not appear to be significantly different (P = .5138) between the 2 groups.
Multivariate analysis
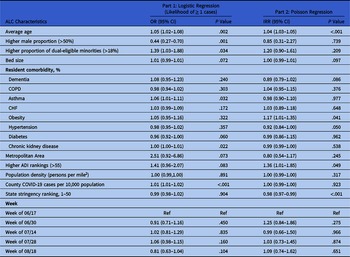
In Table 2 we report the results of the 2-part model controlling for ALC, neighborhood, and state level factors. We detected significant associations between higher proportion of dual-eligible minority residents (P = .034) and the likelihood of ALCs having at least 1 COVID-19 case. ALCs located in more disadvantaged neighborhoods (ie, higher ADI) had greater odds (OR, 1.41; P = .083) of having at least 1 COVID-19 case. State stringency rankings were not significantly associated with the likelihood of ALCs experiencing a COVID-19 outbreak (P = .904).
Table 2. Regression Analysis of the Number of Cases in Assisted Living Communities (ALCs)

Note. OR, odds ratio; CI, confidence interval; ADI, area deprivation index; COPD, chronic obstructive pulmonary disease; CHF, chronic heart failure.
Furthermore, the odds of ALCs having at least 1 COVID-19 case were higher in communities with older residents (OR, 1.05; P = .002), a higher proportion of residents with asthma (OR, 1.06; P = .032) or chronic kidney disease (OR, 1.00; P = .022), and those located in counties with more COVID-19 cases (OR, 1.01; P < .001). ALCs with a higher proportion of male residents were associated with a lower likelihood of COVID-19 outbreak (OR, 0.44; P = .0002).
Conditional on having at least 1 COVID-19 case, ALCs in states with more stringent COVID-19 policies appeared to have had a significantly lowered risk of COVID-19 case count (IRR, 0.98; P ≤ .0001), while those located in more disadvantaged areas (higher ADI) exhibited higher COVID-19 penetration (IRR, 1.36; P = .049) (Table 2, part 2). We detected no statistically significant association between the proportion of dual minority residents (IRR, 1.20; P = .209) and COVID-19 case count in ALCs. Also, we detected no statistically significant differences in the case counts across the sampled weeks.
Discussion
In this study, we examined ALC factors, community-level socioeconomic deprivation, and state-level social-distancing policies, and their associations with COVID-19 cases. ALCs with a higher proportion of the dually eligible minority residents were more likely to have at least one COVID-19 case. State policies regarding social distancing, such as masking, gathering restrictions and business closures, were not associated with the likelihood of a COVID-19 outbreak in an ALC (ie, having at least 1 case). But more stringent state-level restrictions, along with lower neighborhood deprivation, were associated with fewer cases within an ALC that has experienced a COVID-19 outbreak. These findings support our initial hypothesis for the association of ALC, community, and state factors with COVID-19 cases.
Our findings regarding the association of COVID-19 cases with the proportion of minority residents in ALCs are consistent with prior research. Reference Temkin-Greener, Guo, Mao, Cai and Li20 The associations between ADI, state social-distancing policies and COVID-19 cases, which we have demonstrated for the ALCs, were also borne out in prior nursing home studies. Reference Li, Cen, Cai and Temkin-Greener6–Reference Cai, Yan and Intrator8,Reference Sugg, Spaulding and Lane10,Reference Kandula and Shaman33,Reference Ryskina, Yun, Wang, Chen and Jung34
Our findings have several implications. First, the Centers for Disease Control and Prevention (CDC) and state governments issued a number of guidelines and recommendations for preventing the spread of COVID-19 in long-term care facilities. 35,36 These guidelines, however, did not specifically recommend greater vigilance for facilities with higher minority and lower SES residents, or for facilities located in higher ADI areas. No specific information was available on how ALCs responded to these recommendations. ALCs, compared to nursing homes, may have faced significantly different issues in responding to the recommendations due to the population they serve. Reference Zimmerman, Carder and Schwartz21,Reference Zimmerman, Sloane, Katz, Kunze, O’Neil and Resnick37 Such knowledge may be beneficial in addressing future interventions and public policy to better protect the already vulnerable residents of such communities. Second, the Coronavirus Aid, Relief, and Economic Security (CARES) Act, enacted on March 27, 2020, included a specific $15 billion to the Department of Health and Human Services (DHHS) in helping long-term care facilities purchase personal protective equipment (PPE) and increase testing capacities. 38 Although ALCs serving the dually eligible Medicare beneficiaries have been included in this funding, they represent only a fraction of all ALCs. The DHHS and other health agencies may consider targeting funding to facilities at higher risk of disease spread, for example, those located in more disadvantaged areas. Third, with the success of COVID-19 vaccine rollouts, the CDC has lifted the nationwide mask mandates and recommendations for social distancing for vaccinated people. 39,40 ALCs, particularly those at high risk of COVID-19 spread, may need to exercise extra caution when lifting these pandemic precautions within their community. Finally, as state-level policy stringency appears to reduce the spread of COVID-19 in long-term care facilities, including in ALCs, public policy experts may wish to consider how to expedite and/or target the rollout of such policies in future epidemics or pandemics.
This study had several limitations. First, due to data availability, we only examined a 5-week trend, which may not have adequately captured the crest of the Fall 2020 COVID-19 wave across some states. However, our findings were statistically significant even prior to the peak of the wave in some states; thus, a longer time trend would likely confirm the results we presented. Second, omitted variable bias is a concern. Specifically, information on the frequency of COVID-19 testing and/or positivity among ALC caregivers was not available. Third, information on ALC-level characteristics was derived from the 2018 MBSF data. Although it is not likely that these characteristics have changed dramatically in 2019–2020, the possibility remains.
In conclusion, ALCs with higher proportions of dual-eligible minority residents were more likely to have COVID-19 outbreaks within their communities. ALCs located in states with less stringent state-level policies on social distancing and those in more socioeconomically deprived neighborhoods tended to experience greater COVID-19 penetration. These findings suggest that state policy makers may consider paying more attention to and allocating resources to ALCs serving more dually eligible residents, particularly those located in more socioeconomically deprived areas.
Acknowledgments
Financial support
This study was funded by the Agency for Healthcare Research and Quality (AHRQ grant no. R01HS026893) and by The Patrick and Catherine Weldon Donaghue Medical Research Foundation, Another Look 2020.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.