To the Editor—A peripherally inserted central catheter (PICC) provides outpatient access to long-term parenteral antibiotics.Reference Wai, Frighetto, Marra, Chan and Jewesson 1 , Reference Goodfellow, Wai and Frighetto 2 Most antimicrobial stewardship systems do not have an outpatient parenteral antibiotic therapy (OPAT) program or mandatory infectious diseases (ID) consultation prior to patient discharge.Reference Lane, Marschall and Beekmann 3 Such programs ensure that PICC insertions are appropriate to avoid excessive antibiotic usage, line-associated complications, and antimicrobial resistanceReference Shrestha, Bhaskaran, Scalera, Schmitt, Rehm and Gordon 4 – Reference Paladino and Poretz 6 . Here, we report a simple intervention that identifies patients at risk for unnecessary parenteral antibiotics and recommends ID consultation. The intervention resulted in an 84% relative risk reduction in patients discharged with PICC insertions without ID consultation.
The study was performed at a 1,134-bed academic medical center. Between January 2016 and May 2016, 181 PICC orders were placed for parenteral antibiotics (Fig. 1A), and 172 of these included ID consultation (95%) while 9 (5%) did not. Two ID attending physicians retrospectively reviewed these 9 cases and concluded that 8 PICC insertions (89%) were inappropriate.
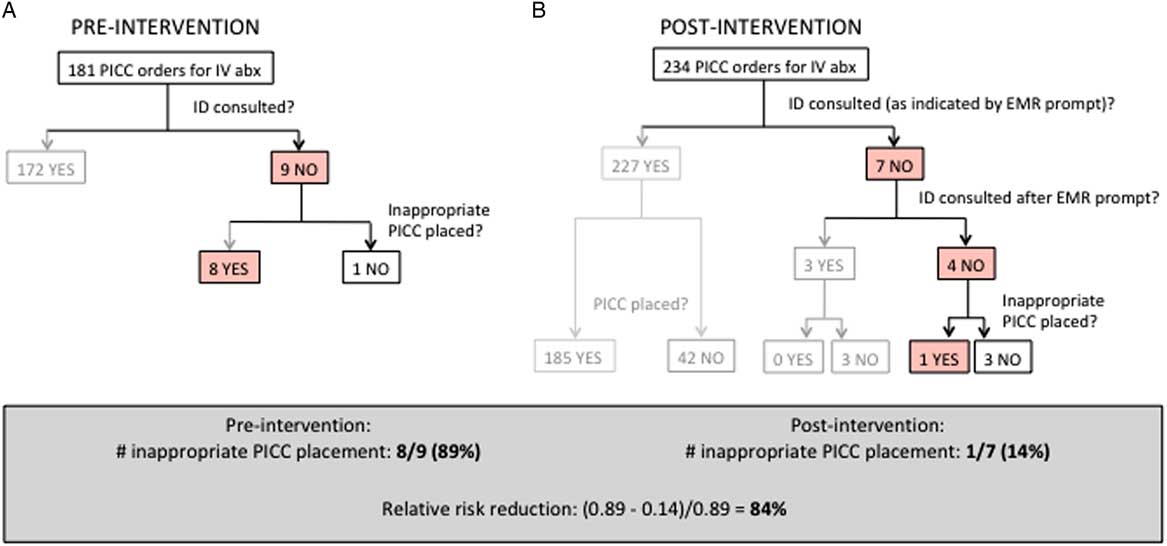
Fig. 1 Pre- and postintervention flowchart. (A) Before the intervention, 181 PICC insertion orders were placed for parenteral antibiotics. Overall, 172 patients received ID consultation, while 9 patients did not, and 8 of those 9 patients had an inappropriate PICC insertions. (B) Postintervention, 234 orders for PICC insertions were placed for parenteral antibiotics. Among 227 patients indicating that ID was consulted, 185 patients had PICC placement and 42 did not. Seven patients were prompted to consult ID. For 3 of those patients, providers consulted ID and the patients ultimately did not have PICC insertions. For 4 of those patients, ID consultation was not obtained. Of those 4 patients, 3 did not require a PICC, while 1 had a PICC placed that was deemed inappropriate.
An electronic intervention was implemented into the PICC insertion order set in November 2016. Three prompts were inserted to ensure ID consultation for all PICC insertions for parenteral antibiotics: (1) “Will the PICC be used for IV antibiotics?” A “No” response prompted the original order set. A “Yes” prompted the following question: (2) “Is ID consulted?” A “No” prompted the statement: “ID consultation is required prior to PICC placement for IV antibiotics. Please consult an ID team.” (3) In this case, the provider would need to select: “ID will be consulted immediately.” This project was a quality improvement initiative conducted by the Quality Improvement Committee at the Mount Sinai Hospital.
After launching the electronic intervention, 234 PICC orders were placed for parenteral antibiotics between December 2016 to May 2017 (Figure 1B). Seven instances triggered “ID will be consulted immediately.” Three patients had ID consultation and did not have a PICC inserted. Four patients did not have ID consultation. Among these, 3 patients were switched to oral antibiotics without ID consultation. Finally, 1 patient (among the 7 instances) was discharged with a PICC insertion without ID consultation and had an unfavorable outcome.
1 of 7 patients was discharged with an inappropriate PICC insertion without an ID consultation, a reduction of 89% (8 of 9 patients) before the intervention. Thus, the EMR intervention resulted in an 84% relative risk reduction of inappropriate PICC insertions. All charts for whom PICC insertions occurred without ID consultation were independently reviewed by 2 ID attending physicians. In 24 of 26 reviews (92%), ID consultation would have changed treatment management to avoid PICC insertion.
In conclusion, this intervention provides a sustainable and cost-effective antimicrobial stewardship approach to reduce inappropriate parenteral antibiotics usage. It also highlights the importance of ID consultation in determining the appropriateness of long-term outpatient parenteral antibiotic therapy.
Acknowledgements
We thank the EMR team for implementing the electronic intervention.
Financial support
This work was supported by a grant from the National Institutes of Health (NIH)/National Institute of Allergy and Infectious Diseases (NIAID) (grant no. K-08AI120806).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.



