1. Policy points
• At the start of the COVID-19 pandemic, the World Health Organization (WHO) issued the Access to COVID-19 Tools Accelerator (ACT-A), for equitable global access to COVID-19 health technologies. While innovative, internal and external reviews suggest the need for a new mechanism for expanding access to essential countermeasures.
• Several international processes to better prepare for and respond to future pandemics are ongoing. The United Nations' High Level Meetings on Pandemic Preparedness and Response took place in September 2023 and produced a political declaration attempting to galvanise political leadership. If negotiations in Geneva succeed, the World Health Assembly is set to consider adoption of two international instruments in May: a new pandemic agreement to improve preparedness, response, and equity; and amendments to the International Health Regulations (IHR) (World Health Organization, 2024). This will likely be followed by a WHO design and consultation process on a new medical countermeasures platform. The current draft of the pandemic agreement outlines a Pathogen Access and Benefit Sharing System to work in conjunction with a Global Supply Chain and Logistics Network and the conference of parties as well as several more specific provisions or articles to improve access to essential countermeasures in a declared pandemic that might be part of this platform. Yet, there is currently disagreement about how robust these mechanisms will be. To advance these efforts, we propose an enhanced countermeasures platform that we will refer to as the APT-A (Access to Pandemic Tools Accelerator). Our proposal goes beyond the previous, and outlined, global architecture and includes two new components or pillars – one for economic assistance and another to combat structural inequalities for future pandemic preparedness and response.
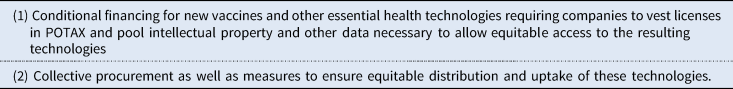
• As part of the APT-A, and in light of the Independent Panel on Pandemic Preparation & Response's call for an enhanced end-to-end platform for access to essential health technologies, we propose a new mechanism that we call the Pandemic Open Technology Access Accelerator (POTAX). This mechanism can be implemented through the medical countermeasures platform and the pandemic agreement currently under negotiation through the World Health Assembly and inform upcoming reviews of the High-Level Meeting on Pandemic Prevention, Preparedness, and Response's aspirations at the United Nations. This mechanism will 1) provide conditional financing for new vaccines and other essential health technologies requiring companies to vest licenses in POTAX and pool intellectual property and other data necessary to allow equitable access to the resulting technologies. It will also 2) support collective procurement as well as measures to ensure equitable distribution and uptake of these technologies.
2. Improving pandemic response plans
To date 7 million people have died from the COVID-19 pandemic and some estimates suggest it cost the world 12.5 trillion dollars (World Health Organization, 2020b, 2022a, 2022b, Shalal, Reference Shalal2022). Nevertheless, in terms of the potential lives lost, it was not a major pandemic (LePan, Reference LePan2020; World Health Organization, 2020b; Shalal, Reference Shalal2022). The 1918 flu cost 50 million lives and AIDS and smallpox pandemics killed over 25 and 50 million people, respectively (LePan, Reference LePan2020), and the world's population was much smaller on all of those occasions.
As COVID-19 first surged around the world, the World Health Organization (WHO) issued a Solidarity Call to Action for equitable global access to COVID-19 health technologies by pooling of knowledge, data, and intellectual property. The WHO COVID-19 Strategic Preparedness and Response Plan to guide country-response efforts and the Access to COVID-19 Tools Accelerator (ACT-A) – a platform for international support – were the other main components of the global response (World Health Organization, 2020c, 2020d).
As has become clear, especially in hindsight, the global response to the COVID-19 pandemic has been grossly inadequate. Starting from the perspective that there were significant inequalities in the global response we seek here to provide a way to overcome key criticism of the response (The Civil Society and Community Representatives of the ACT-A, 2021; World Health Organization, 2022a, 2022b). Critics of the ACT-A argued that the international mechanism for cooperation was not sustainable or well-governed and that it did not ensure equitable access to new vaccines and other essential health technologies for all. Moreover, they argued that much more sustained investments in basic health systems were necessary to address the structural inequalities in health that exacerbated the pandemic's negative economic, as well as health, consequences (Sabatello et al., Reference Sabatello, Scroggins, Goto, Santiago, McCormick, Morris, Daulton, Easter and Darien2021). Finally, many contend that much greater cooperation is necessary for the international community to prevent and respond to future pandemics (Dodds, Reference Dodds2019; The Civil Society and Community Representatives of the ACT-A, 2021).
In light of this criticism, several international processes to better prepare for, and respond to, future pandemics are ongoing. Recent United Nations' High Level Meetings have produced a political declaration on pandemic preparedness and response attempting to galvanise political leadership and coordination and ensure more equitable access to essential countermeasures (United Nations, 2023). If negotiations in Geneva succeed, the World Health Assembly is set to consider adoption of two international instruments in May: a new pandemic agreement to improve preparedness, response, and equity; and amendments to the International Health Regulations (IHR) (World Health Organization, 2024). This will likely be followed by a WHO design and consultation process on a new medical countermeasures platform as an ‘interim global coordination mechanism…’ and its structure will depend on how ‘the Intergovernmental Negotiating Body (INB) deliberations on a future Pandemic Accord and the deliberations of the Working Group on Amendments to the International Health Regulations (2005) (WGIHR)’ turn out as they will likely have ‘substantial implications for the future pandemic countermeasures architecture’ (World Health Organization, 2023a, 2023b). The current draft of the pandemic agreement outlines a Pathogen Access and Benefit Sharing System to work in conjunction with a Global Supply Chain and Logistics Network and the conference of parties as well as several more specific provisions or articles to improve access to essential countermeasures in a declared pandemic that might be part of this platform. Yet, there is currently disagreement about how robust these mechanisms will be. To advance these efforts, we propose an enhanced countermeasures platform that we will refer to as the APT-A (Access to Pandemic Tools Accelerator). This proposal provides a concrete mechanism for implementing the Independent Panel on Pandemic Preparation & Response's recommendation to create an enhanced end-to-end platform that will ensure equitable access to essential health technologies. We detail some specific recommendations for treaty text development in Appendix C (Evaborhene et al., Reference Evaborhene, Udokanma, Adebisi, Okorie, Kafuko, Conde, Waliaula and Mburu2023; Moss, Reference Moss2023).
More precisely, we propose the APT-A as a way of enhancing equity and access to essential countermeasures in a new pandemic preparedness and response agreement and similar initiatives under discussion. Our proposal goes beyond the previous and outlined global architecture and includes two new components or pillars – one for economic assistance and another to combat structural inequalities (World Health Organization, 2022a, 2022b). As part of the APT-A, we advance a new mechanism that we call the Pandemic Open Technology Access Accelerator (POTAX) (Saxena et al., Reference Saxena, Baker, Banda, Herlitz, Miller, Karrar, Fleurbaey, Chiwa, Atuire, Hirose and Hassoun2023). This mechanism requires (1) conditional financing for new vaccines and other essential health technologies requiring companies to vest licenses in POTAX and pool intellectual property and other data necessary to allow equitable access to the resulting technologies. Our mechanism also requires (2) supporting collective procurement – or coordinated purchasing efforts through organisations like UNICEF – as well as measures to ensure equitable distribution and uptake of essential countermeasures (UNICEF, 2022).
We argue that our proposal may help make the investments in health technologies and systems necessary to prevent and address future pandemic threats sustainable. Responsibility for the APT-A and POTAX would not be vested in anything like the ACT-A's facilitation council, however, as it failed to represent the global population's interests and gave undue weight to industry perspectives (Moon et al., Reference Moon, Armstrong, Hutler, Upshur, Katz, Atuire, Bhan, Emanuel, Faden and Ghimire2022). Rather, the Secretariat of the pandemic agreement, with support from the UN's High-Level process, should create a governance mechanism that represents the interests of the global population independent of membership in a particular state. This mechanism should, thus, ensure that developing country perspectives and interests cannot be sidelined by more powerful states. After reviewing previous pandemic response plans in more detail, this paper 1) explains each component of our proposal in turn, 2) considers its governance, financing, and implementation, and 3) evaluates past successes, obstacles, and potential modifications.
2.1 The COVID-19 pandemic preparation and response architecture
Critics argue that the global response to the COVID-19 pandemic failed to live up to expectation because the international community failed to respect, protect, and fulfil individuals' human rights to health (Haldane et al., Reference Haldane, Jung, De Foo, Bonk, Jamieson, Wu, Verma, Abdalla, Singh, Nordstrom and Legido-Quigley2021; The Civil Society and Community Representatives of the ACT-A, 2021; Pushkaran et al., Reference Pushkaran, Chattu and Narayanan2023). The International Covenant on Economic, Social and Cultural Rights Article 12 on the human right to health states that everyone has a right to physical and mental health and this right requires controlling endemic, epidemic, and other diseases. The General Comments on the right specify that it requires helping people access the social determinants of health as well as essential medical services – including essential vaccines, treatments, and other basic healthcare services (United Nations Committee on Economic, Social and Cultural Rights, 1990).
We suppose throughout that equitable access to essential medical services requires making these technologies available, affordable, acceptable, adaptable, and accessible to everyone without discrimination. Moreover, we endorse the other ICESCR Articles and Comments that explain the corresponding human rights responsibilities. Article 2(1) specifies, for instance, that each state must undertake:
steps, individually and through international assistance and cooperation, especially economic and technical, to the maximum of its available resources, with a view to achieving progressively the full realisation of the rights recognized in the present Covenant by all appropriate means, including particularly the adoption of legislative measures (UNCESCR, 1990).
While, the third General Comment notes that:
The phrase [in Article 2(1)] ‘to the maximum of its available resources’ was intended by the drafters of the Covenant to refer to both the resources existing within a State and those available from the international community through international cooperation and assistance. The Committee wishes to emphasize that in accordance with Articles 55 and 56 of the Charter of the United Nations, with well-established principles of international law, and with the provisions of the Covenant itself, international cooperation for development and thus for the realisation of economic, social and cultural rights is an obligation of all States. It is particularly incumbent upon those States which are in a position to assist others in this regard (UNCESCR, 1990).
States must protect, respect, and fulfil their citizens' human rights to health and help other states that require assistance.Footnote 1 Even though not all states have ratified the Covenant, we start here from the proposition that everyone should have this legally secured right to the socially controllable determinants of health to protect their ability to live minimally good, or dignified, lives (Hassoun, Reference Hassoun2020). This commitment is echoed at the start of the current draft of the pandemic agreement which states: ‘The objective of the WHO Pandemic Agreement, guided by equity, and the principles and approaches set forth herein, is to prevent, prepare for and respond to pandemics… To achieve the objective of the WHO Pandemic Agreement and to implement its provisions, the Parties will be guided, inter alia, by … full respect for the dignity, human rights and fundamental freedoms of all persons, and the enjoyment of the highest attainable standard of health of every human being.’ (World Health Organization, 2024, Articles 2 & 3) Moreover, it is the basis for much criticism of the COVID-19 global response that we outline below.
The largest component of the global response to the COVID-19 pandemic was through the ACT-A (World Health Organization, 2020a, 2020b, 2020c, 2020d, 2020e). The ACT-A included four pillars and one workstream which are (1) vaccines (2) diagnostics, (3) therapeutics, and (4) the health systems connector as well as the (5) country allocation and access workstream (World Health Organization, 2021a). Countries and other funders met together to invest in each aspect of this global response. They offered a variety of direct grants and advanced market commitments to increase the supply of essential health technologies and help deliver them. International health organisations and funders led different aspects of this response effort from the World Health Organization, Gavi, the Vaccine Alliance, and the Coalition for Epidemic Preparedness Interventions (CEPI) to the Foundation for Innovative New Diagnostics (FIND), UNITAID, and the Gates Foundation.
Critics charge that the global response failed to respect, protect, and fulfil everyone's human right to health in part because the ACT-A's best funded pillar – the COVID-19 Vaccines Global Access pillar (COVAX, Berkeley, Reference Berkeley2020) aimed to increase manufacturing and distribution of COVID-19 vaccines around the world – but did not secure the requisite resources to roll out the vaccine globally in a timely manner (Sekalala et al., Reference Sekalala, Forman, Hodgson, Mulumba, Namyalo-Ganafa and Meier2021; Privor-Dumm et al., Reference Privor-Dumm, Excler, Gilbert, Abdool Karim, Hotez, Thompson and Kim2023; World Health Organization, 2023a, 2020a, 2020b, 2020c, 2020d, 2020e). The COVAX facility offered advance market commitments for new vaccine development – agreeing to purchase vaccines if they were developed to create a stable market and incentives for innovation. COVAX failed to meet its target of vaccinating 20% of the global population by the end of 2021 and 70% of the global population by fall 2022 (Legge, Reference Legge2020; Kavanagh et al., Reference Kavanagh, Gostin and Sunder2021; Aizenman, Reference Aizenman2022; World Health Organization, 2022a, 2022b). By April 2023, only 30% of people in low income countries had received even a single dose and only 24% of low income countries had vaccinated more than 40% of their populations (Gavi, the Vaccine Alliance, 2023; World Health Organization, 2023a).Footnote 2 The other ACT-A components faced similar issues with meeting targets and ensuring equitable access to essential health technologies, in part, because the ACT-A's diagnostics and therapeutics pillars were woefully underfunded; while vaccines received 4.19 billion USD, therapeutics received 0.15 billion, and diagnostics received 0.07 billion in the October 2022 funding cycle (World Health Organization, 2022a, 2022b).Footnote 3 The facility's health system connector (previously called the health systems pillar) and country allocation and access components struggled even to provide health care workers with personal protective equipment – an unambitious goal (The Lancet, 2021).
There are several reasons the ACT-A did not succeed in meeting its targets. Wealthy countries purchased most of the global supply depriving poor countries of access (Reza et al., Reference Reza Mahmud, Agarwal, Sultana, Bari and Mobarak2022). Even when they did share doses, they often did so too late and without providing adequate support to actually distribute the doses around the world (Van de Pas et al., Reference Van De Pas, Widdowson, Ravinetto, Srinivas, Ochoa, Fofana and Van Damme2022). Moreover, companies initially refused to share intellectual property and other data and knowledge necessary for developing essential counter-measures, e.g. through the Covid-19 Technology Access Pool (C-TAP), making it difficult for many countries to manufacture these technologies (Legge, Reference Legge2020; Baumgaertner, Reference Baumgaertner2021; Hassoun, Reference Hassoun2021a; Kavanagh et al., Reference Kavanagh, Gostin and Sunder2021; Sariola, Reference Sariola2021). Even after the vaccines were widely distributed companies insisted on preserving their control over technologies and data that, if shared more widely, could save many more lives (Durkin et al., Reference Durkin, Sta Maria, Willmore and Kapczynski2021).
Furthermore, critics charge that the governance for the ACT-A coordination mechanism failed to represent the interests of all those affected by the pandemic (The Civil Society and Community Representatives of the ACT-A, 2021; World Health Organization, 2022a, 2022b). To be effective and equitable – such coordination mechanisms must give due weight to the perspectives and interests of those their policies affect – empowering them to shape their basic life prospects. Because good coordination mechanisms were not established, and access to essential health technologies was anything but equitable, variants proliferated, many more lives were lost, and economies suffered (Cioffi and Cioffi, Reference Cioffi and Cioffi2021; Morgan et al., Reference Morgan, Awafo and Quartey2021).
Moreover, significant economic support during the crisis was not forthcoming in many countries (Chabert et al., Reference Chabert, Gregory and Pierre2021; International Labor Organization, 2021; Stubbs et al., Reference Stubbs, Kring, Laskaridis, Kentikelenis and Gallagher2021; Okafor and Khalid, Reference Okafor and Khalid2023). The World Bank's Pandemic Emergency Financing Facility (PEF) failed to disburse funds during the acute phase of the pandemic claiming that it was not clear whether countries qualified for assistance. Although the International Financial Institutions eventually offered some additional financing and debt relief for poor countries, sufficient financing to prevent severe economic crises –was not forthcoming (Steel and Harris, Reference Steel and Harris2021). Moreover, critics charge that large stimulus packages in rich countries (and international conflict) exacerbated global inflation and competition for scarce goods, sometimes depriving the world's poorest people of even the most basic sustenance (Shah, Reference Shah2021; Okafor and Khalid, Reference Okafor and Khalid2023).
Perhaps most importantly, critics argue that states and the international community did not take the steps necessary to respect, protect, and fulfil everyone's human right to health before the COVID-19 pandemic hit (United Nations, 2020; Shamasunder et al., Reference Shamasunder, Holmes, Goronga, Carrasco, Katz, Frankfurter and Keshavjee2020; Tessema et al., Reference Tessema, Kinfu, Dachew, Tesema, Assefa, Alene and Aregay2021; Zhang, Reference Zhang2021). Critics charge that many countries lacked sufficient surveillance and containment mechanisms, and that health inequalities exacerbated global pandemic risks (Filip et al., Reference Filip, Gheorghita Puscaselu, Anchidin-Norocel, Dimian and Savage2022). They argue that, historically, the international community did not invest enough in basic health systems in developing countries capable of preventing and addressing many pre-existing conditions that heightened risks of serious illness and death in the pandemic (Katz et al., Reference Katz, Sorrell, Kornblet and Fischer2014; Shamasunder et al., Reference Shamasunder, Holmes, Goronga, Carrasco, Katz, Frankfurter and Keshavjee2020).
In short, critics charge that there are many reasons the global response failed to respect, protect, and fulfil everyone's human right to health: They argue that the global response was poorly governed and did not represent the global populations' interests (ACT-A; World Health Organization, 2021a, 2021b, 2021c, 2021d, 2021e). Instead, states engaged in vaccine nationalism (Hassoun, Reference Hassoun2021b competed for scarce supply, while most pharmaceutical companies insisted on preserving their control over technologies and data that, if shared more widely, would arguably have saved millions more lives (Amnesty International, 2021; Baumgaertner, Reference Baumgaertner2021). Critics argue that poor people in developing countries, in particular, also lacked sufficient economic support in the pandemic, so global poverty increased by between 119 and 124 million people in 2020 (Josephson et al., Reference Josephson, Kilic and Michler2021; Onyeaka et al., Reference Onyeaka, Anumudu, Al-Sharify, Egele-Godswill and Mbaegbu2021; Yonzan et al., Reference Yonzan, Lakner, Mahler, Aguilar and Wu2021).Footnote 4 Finally, critics charge that the international community failed to invest sufficiently in basic health systems, with increased mortality in many countries' because of pre-existing inequality in access to essential health technologies and services (Bollyky and Bown, Reference Bollyky and Bown2020; Dyer, Reference Dyer2020; Acharya et al., Reference Acharya, Ghimire and Subramanya2021; Forman et al., Reference Forman, Shah, Jeurissen, Jit and Mossialos2021; Hassoun, Reference Hassoun2021a).
2.2 Beyond the ACT-A architecture
Given these criticisms, we start here from the premise that greater international cooperation is essential to combat future pandemic threats and address many existing pandemics beyond COVID-19, including AIDS and tuberculosis, and attempt to outline an optimal response mechanism (Bloom and Cadarette, Reference Bloom and Cadarette2019; World Health Organization, 2021a, 2021b, 2021c, 2021d, 2021e). That is, we assume that as drug resistance and climate change threaten to accelerate pandemics, the global community must better prepare for and respond to pandemic threats to uphold everyone's human right to health. We argue for creating an international agreement to sustain cooperation in Appendix A. Of course, criticism is easier with hindsight, but it is important to address these concerns. We discuss some reasons for countries to endorse, and adhere to, an international agreement to implement a proposal along the lines of what we suggest below, but our main aim here is not to argue that such an agreement is sustainable (it may not be). Rather, we set out an aspirational plan for better preventing and addressing pandemics to respect and protect human rights that we believe countries should implement.
Having an ideal, or failing that at least an aspirational, plan in hand is important for several reasons (Krikorian and Torreele, Reference Krikorian and Torreele2021). First, we believe that what the international community can do together is up to us. We outline a mechanism that can inform the pandemic agreement negotiations and the development of new countermeasures platforms. Even if it is impossible to implement an optimal response, articulating it may help inform and improve existing plans that will better fulfil individuals' human rights to the socially controllable determinants of health. Finally, even if it is not fully implemented now, outlining the mechanism can inform public discussions and debates about pandemic preparedness and response architecture in the future.
2.3 Our proposal
We propose creating a new response mechanism – the APT-A – that will provide more funding for vaccines, diagnostics, therapeutics, health systems and access and include two new pillars – one for economic assistance in pandemic times and another for preparedness in combating structural inequalities in health. As part of our proposal, we argue for creating something like an expanded version of COVAX – POTAX – to sustainably increase access to essential health technologies over time. Finally, we propose adopting a new governance structure to ensure decisions reflect the interests of all those affected by pandemic diseases (Table 1).
Table 1. Access to pandemic tools accelerator (APT-A) pillars or workstreams

POTAX aims to speed up research, development, and equitable provision of essential countermeasures at low prices and provides (1) conditional financing for new countermeasures requiring companies to vest licenses in POTAX and pool intellectual property and other data necessary to allow equitable access to the resulting technologies. It also (2) supports collective procurement as well as measures to ensure equitable distribution and uptake of these technologies (Table 2).
Table 2. Key provisions of the pandemic open technology access accelerator (POTAX)
3. POTAX and the APT-A
3.1 POTAX
Consider each component of our proposal, in turn, starting with the components in POTAX that can be implemented through the medical countermeasures platform and the pandemic accord and supported by UN processes. First, we propose that countries finance essential countermeasures on the condition that companies vest licenses in POTAX and pool intellectual property and other data necessary to allow equitable access to the resulting technologies (World Health Organization, 2020e). Although COVID-19 vaccines were produced in record time, many counter-measures necessary for adequate pandemic preparedness and response are simply not forthcoming given the status-quo incentives for new innovation. Companies have produced few new antibiotics despite growing resistance rates, for instance, and the COVID response rate demonstrates that, for similarly complex innovations, it is possible to accelerate the development timeline.Footnote 5 Reducing barriers to innovation through a collaborative R&D system can increase R&D.Footnote 6 So, the international community should support and, in some cases, require companies to utilise patent pools – and share non-patented information – as trade secrets can greatly hinder the global response. Ensuring equitable access to new technologies may also require data and market exclusivity waivers (to allow generics and biosimilar production) in voluntary licensing agreements (World Health Organization, 2020e; Morin et al., Reference Morin, Hannah, Oliver, von Christian, Jeffrey and Burrone2022). In entering into such agreements, companies agree to forego some (or all) patent rights. Where companies refuse to offer voluntary licenses, the World Trade Organizations' Trade Related Intellectual Property Rights Agreement (TRIPS) allows compulsory licenses, and states should require companies to share their intellectual property, data, and know-how for fair compensation in public health emergencies.Footnote 7 Countries and international organisations should also streamline new drug approval processes.
We propose offering financial incentives for new research and development where possible based on health impact. As long as the incentives generate the requisite research and development, this system can be voluntary. Alternatively, countries can require companies to share the requisite data on R&D costs and provide additional funds based on the global health impacts of the technologies with milestone – as well as some up front – payments. Good measures of new technologies' health impacts already exist and researchers can expand this evaluation to form the basis for the requisite incentives (Hassoun, Reference Hassoun2015; Hassoun and Cosler, Reference Hassoun and Cosler2023; Hassoun et al., Reference Hassoun, Friedman and Cosler2022).
This proposal delinks companies' profits from sales volume and ties them to good health consequences instead. Though, in specifying an ideal outcome, we have to be mindful of the incentives needed for individuals and corporations to produce new countermeasures, we believe that the current system wrongly allows major companies to reap profits by holding back production and pushing up prices. Holding back supplies may be fine by way of incentives for luxury goods but not for necessities. The international community should implement other existing ways of compensating corporations and, if advanced economies cooperate, that is certainly feasible. It is likely more feasible in non-pandemic times (where there is no supply crunch) than at the onset of a major pandemic. So, we suggest investing in an arsenal of interventions to combat long-term ongoing health crises and future pandemic threats today.
We propose offering financing, however, only on the condition that there is equitable access to the resulting vaccines and other technologies (Moon et al., Reference Moon, Adrian and Vieira2021; World Health Organization, 2021a, 2021b, 2021c, 2021d, 2021e). The key is that if the international community pays for new technologies, they should own the resulting products (The Global Health Centre at Graduate Institute Geneva, 2021). Rights to new technologies should be vested in POTAX under the purview of the WHO – which should be tasked with licensing production to (e.g. generic) manufacturers with specific pricing and other equitable access conditions (e.g. requiring first purchase rights go to collective procurement organisations at set price points). About 80% of global manufacturing is in the generics sector and generic competition often reduces drug costs (Miller, Reference Miller2020: 12–13; Conrad and Lutter, Reference Conrad and Lutter2019). So, rather than letting patent holding companies compete for manufacturing capacity, allowing generics (or bioequivalent) competition will reduce transaction costs, and may greatly reduce consumers' costs when supply is not limited. Licenses, data, and knowledge vested in POTAX might allow it to specify access conditions (costs and supply conditions) in sublicenses for manufacturers when supply is constrained. If new technologies are approved by stringent regulatory authorities and receive WHO Prequalification, there should be few further regulatory hurdles necessary for production.Footnote 8
Second, countries should support collective procurement as well as other measures to ensure equitable distribution and uptake of these technologies. Countries should commit to fully funding provision of resulting products for all in a timely and equitable manner and allow POTAX to coordinate procurement. Working together with international and regional procurement agencies like UNICEF and the Pan American Health Organization's (PAHO's) revolving fund, POTAX can help coordinate global distribution and set prices sufficient to recoup investments in rich countries while subsidising production in poorer ones.Footnote 9 Some collective procurement efforts only involve sharing information (on price, budgets, forecasts, or the legal landscape). Others include or pooled price negotiation, contracting, logistics, acquisition, and delivery of essential health technologies (Nemzoff et al., Reference Nemzoff, Kalipso and Mead2019). Here we support scaling up acquisition and delivery efforts to ensure that people even in the poorest countries receive essential health technologies in a timely manner (Nemzoff et al., Reference Nemzoff, Kalipso and Mead2019). Global coordination should help ensure that products are priced differentially to ensure affordability and recoup investment costs (Nemzoff et al., Reference Nemzoff, Kalipso and Mead2019). Other measures to support the distribution and uptake of essential health technologies should be in scope.
3.2 Other APT-A pillars and governance structure
Beyond POTAX, countries should provide much more support for the APT-A's diagnostics, therapeutics, access, and basic health systems pillars. Each of these pillars and workstreams is essential for combatting pandemics. However, basic health systems and equitable access are also important for distributing essential health technologies. For, it is not enough just to produce these technologies, they have to be manufactured, distributed, and consumed by people around the world (Herlitz et al., Reference Herlitz, Lederman, Miller, Fleurbaey, Venkatapuram, Atuire, Eckenwiler and Hassoun2021). Funding is essential not only for manufacturing, but transportation and distribution, health care infrastructure, and workers.
Members of marginalised communities are often most at risk in health emergencies due to pre-existing inequalities in access to health and other resources, opportunities, and institutions, as well as structural injustice (Benfer et al., Reference Benfer, Mohapatra, Wiley and Yearby2021). Members of religious and ethnic minority groups were often more likely to acquire COVID-19 and suffer from its devastating effects (Office of the United Nations High Commissioner for Human Rights, 2021). The global poor were also less likely to secure diagnostics, therapeutics, and vaccines (Shadmi et al., Reference Shadmi, Chen, Dourado, Faran-Perach, Furler, Hangoma, Hanvoravongchai, Obando, Petrosyan, Rao, Ruano, Shi, de Souza, Spitzer-Shohat, Sturgiss, Suphanchaimat, Uribe and Willems2020). Moreover, health inequalities, and inequalities in access to care, afflict people with many conditions besides COVID-19 (and pandemics can exacerbate these inequalities) (World Health Organization and The World Bank, 2021). The poorest, least educated, and most vulnerable subgroups (e.g. those living in rural areas) are often at the greatest disadvantage (World Health Organization and The World Bank, 2021). This applies to testing as well as treatment. For instance, there is significant inequality in HIV testing, while children under 5 in the poorest, least educated, and rural sub-groups were the least likely to receive malaria care (World Health Organization, 2022a, 2022b). So, we propose a preparation pillar or workstream to combat structural health inequities and prepare for the future pandemics.
To combat structural inequities, our proposed preparation pillar or workstream would provide significant funding to address major health inequities. The social determinants of health include food, water, education, healthcare but also community and social context, built and natural environment, and economic stability (Artiga and Hinton, Reference Artiga and Hinton2018). It is possible to improve the baseline health of minority populations with targeted investments in nutrition, education, social and economic support, as well as healthcare systems (Williams et al., Reference Williams, Costa, Odunlami and Mohammed2008). Structural determinants of health include economic, social, and political policies that affect the distribution of prestige, power, and resources and, thereby, health (Mays, Reference Mays2021). Addressing the social and structural determinants of health requires investing significantly in education and outreach initiatives, healthcare workforce and infrastructure, but also access to other resources and social support services.Footnote 10 Along with significant investments in traditional healthcare infrastructure and workforce, where people cannot get to health clinics, telemedicine and mobile clinics may be particularly important (Yu et al., Reference Yu, Hill, Ricks, Bennet and Oriol2017; Parker et al., Reference Parker, Fang and Bradlyn2020; Haleem et al., Reference Haleem, Javaid, Singh and Suman2021). Programs intended to improve access to clean and safe food, water, shelter and other social support services should be in scope (Gundersen and Ziliak, Reference Gundersen and Ziliak2015). The preparation pillar or workstream, would also invest and engage members of underrepresented groups in the develoment, and implementation of, potentially inequality-reducing laws, policies, and practices (Chin et al., Reference Chin, King, Jones, Jones, Ameratunga, Muramatsu and Derrett2018; Baum et al., Reference Baum, Townsend, Fisher, Browne-Yung, Freeman, Ziersch, Harris and Friel2022).
Moreover, when a pandemic strikes, countries and their inhabitants require economic assistance so we propose including an economic support pillar or workstream in collaboration with international financial institutions including the International Monetary Fund, World Bank, and regional development banks. Rich countries should provide adequate international aid, perhaps supported by special drawing rights for unconditional, interest-free loans to poor countries (Huang et al., Reference Huang, Tan, Zhang and Zhu2021: 21–37). This will require creating better mechanisms to provide surge financing at the start of major outbreaks. The international community should also provide more support for debt relief and economic recovery going significantly beyond the G20's ‘Debt Service Suspension Initiative’ (DSSI) and its ‘Common Framework for Debt Treatments Beyond the DSSI’ (Huang et al., Reference Huang, Tan, Zhang and Zhu2021: 21–37).Footnote 11 Providing stimulus support along the lines of what the US provided for its population (25% of GDP) for developing countries would cost 7.75 trillion US dollars, but more targeted support would cost much less and it is essential to keep in mind all the costs of providing stimulus for the poor (e.g. due to increasing inflation) (The World Bank, 2019; Statistica, 2021). Financing plans should suffice to uphold individuals’ human rights to health (including sufficient economic security for health). However, the Pandemic Financial Intermediary Fund has so far fallen far short of its goal – countries have pledged US$1.6 billion of the US$10.5 billion it aims to mobilise per year – and significant additional financing is necessary even to ensure access to essential countermeasures in pandemic times (see Appendix B and Table B1) (Geneva Global Health Hub, 2022; Pecetta et al., Reference Pecetta, Tortorice, Scorza, Pizza, Dougan, Hatchett, Black, Bloom and Rappuoli2022; The World Bank, 2022). The requisite security also has an intricate economic dynamic requiring consideration: If each nation worries that it may not have enough vaccines in a pandemic, it will stockpile. But this in turn can increase other nations’ anxiety further increasing stockpiling. If there is a carefully designed system of inter-country mediation, countries may stockpile less, easing the shortage faced by poorer nations. The World Bank, United Nations, and other international agencies are well placed to design this kind of multi-country policy.
Finally, to avoid privileging the interests of private organisations or rich countries' citizens, countries must work together to advance the interests of all affected in implementing the APT-A.Footnote 12 Transparency, accountability, and adequate representation across all governance components are essential so that the APT-A truly advances the interests of its diverse, global constituency (Duff et al., Reference Duff, Liu, Saavedra, Batycki, Morancy, Stocking, Gostin, Galea, Bertozzi, Zuniga, Alberto-Banatin, Dansua, del Rio, Kulzhanov, Lee, Scaglia, Shahpar, Ullmann, Hoffman, Weinstein and Szapocznik2021: 428–433, Faviero et al., Reference Faviero, Stocking, Hoffman, Liu, Bausch, Galea, Gostin, Gurría, Halton, Kulzhanov, Leite, Mahama, Mahmood, Miranda, del Rio, Weinstein, Saavedra and Szapocznik2022). This requires diversifying decision-making throughout the mechanism's governance structure and empowering regional as well as national and sub-national leadership. Global South/LIMIC representatives should be included from the start and have proportional influence in all pillars and parts of the global response plan from financing to delivery. Voices from the Global South must receive due weight to ensure that the mechanism is attentive and responsive to the indigenous knowledge necessary for developing adequate preparation and response plans (Marquez et al., Reference Marquez, Kerkhoff, Naso, Contreras, Diaz, Rojas, Peng, Rubio, Jones, Rojas, Gonzalez, Fuchs, Black, Ribeiro, Nossokoff, Tulier-Laiwa, Martinez, Chamie, Pilarowski, DeRisi, Petersen and Havlir2021; WHO 2022a, 2022b; Evaborhen et al., 2023).
3.3 On financing and implementation
Cost estimates for adequate pandemic preparation and response vary widely, and we endorse significant investments. The EU Commission and US government have proposed between US $50 and 65.3 billion over 10 years for pandemic preparedness efforts (Duff et al., Reference Duff, Liu, Saavedra, Batycki, Morancy, Stocking, Gostin, Galea, Bertozzi, Zuniga, Alberto-Banatin, Dansua, del Rio, Kulzhanov, Lee, Scaglia, Shahpar, Ullmann, Hoffman, Weinstein and Szapocznik2021: 428–433). But the international community needs to invest much more. The G20 independent panel estimates that the international community needs to invest US $170 billion for health system strengthening and medical countermeasures over 5 years alone and a recent paper in Science argues that to develop vaccines for 20 potential pandemic pathogens requires US $680 billion (Shanmugaratnam et al., Reference Shanmugaratnam, Summers, Okonjo-Iweala, Botin, El-Erian, Frenkel, Grynspan, Ishii, Kremer, Mazumdar-Shaw, Moreno, Reichlin, Røttingen, Songwe, Suzman, Thiam, Trichet, Woods, Min, Ahmed, Wolff, Dzau and Farrar2021; Pecetta et al., Reference Pecetta, Tortorice, Scorza, Pizza, Dougan, Hatchett, Black, Bloom and Rappuoli2022). Moreover, on the ground estimates for actual vaccination costs in developing countries are often around US 20 dollars per person (Chinkhota et al., Reference Chinkhota, Janoch, Kalyanpur, Mwale and Shannon2022; Janoch et al., Reference Janoch, Santa and Nikantha2022, Reference Janoch, Jamshidi and Ojwang2023; Juneja et al., Reference Juneja, Gupta, Moon, Resch and Beck2017; Zulu et al., Reference Zulu, Janoch, Prather and Selva2022). So, even once vaccines are developed, it might cost more than US $120 billion to vaccinate everyone (that is the more than 6 billion people) in developing countries. Still, given that the pandemic was burning up half a trillion USD per month at its start, speeding up vaccine production by even 8 days would suffice to pay back this cost (Pecetta et al., Reference Pecetta, Tortorice, Scorza, Pizza, Dougan, Hatchett, Black, Bloom and Rappuoli2022). Sustained investments in basic health systems and economic recovery might also prove cost-effective (see Appendix B).
Historically, the international community has implemented mechanisms similar to our proposal and historical evidence suggests that they can be quite effective especially when market incentives are too weak to generate sufficient supply (as is the case in inter-pandemic times for essential counter-measures). Consider the Medicines Patent Pool (MPP), which allows companies to pool patents for HIV, hepatitis C, and tuberculosis and COVID-19 technologies. It has helped develop key HIV, TB, and hepatitis C drugs, expand generic production, reduce prices, and ensure access to several essential medicines (Cox, Reference Cox2012; t'Hoen, Reference t'Hoen2022). The MPP gets companies to offer products on non-exclusive licenses to manufacturers for generic production. For instance, the White House/National Institutes of Health offered a non-exclusive, royalty free license to distribute darunavir to all LMICs in 2010 (Shanmugaratnam et al., Reference Shanmugaratnam, Summers, Okonjo-Iweala, Botin, El-Erian, Frenkel, Grynspan, Ishii, Kremer, Mazumdar-Shaw, Moreno, Reichlin, Røttingen, Songwe, Suzman, Thiam, Trichet, Woods, Min, Ahmed, Wolff, Dzau and Farrar2021: 298–9).Footnote 13 Data suggests that the MPP increases both licensing and the speed with which licenses are granted – hastening the introduction of life-saving drugs in poor countries (Galasso and Schankerman, Reference Galasso and Schankerman2021: 15–27). Researchers find that the MPP increased generic production by about 7% points per drug/country ‘a substantial increase given the already high generic drug coverage in developing countries’ (Wang, Reference Wang2021: 18). By 2016, the MPP had entered into agreements with seven patent holders for 13 anti-retroviral medicines with 12 manufacturers and had more than 60 sub-licensed projects (Wang, Reference Wang2021). They report having saved consumers US $312 million by 2015 and project cost savings from ARVs of US $2.3 billion by 2028 (Wang, Reference Wang2021).Footnote 14 More recently the MPP has secured licenses for several key patents for COVID-19.
Other organisations like Drugs for Neglected Disease Initiative (DfNDi) and Medicines for Malaria venture have also succeeded in securing licenses and good access terms on new technologies at low cost as have some prize funds and other public private partnerships (World Bank Group, 2007; Drugs For Neglected Diseases Initiative, 2014). DfNDi has, for instance, helped develop key anti-malarial artesunate and mefloquine (AS + MQ), a fixed dose combination treatment.Footnote 15 Precisely to help in discussions of the pandemic accord and medical countermeasures design and consultation process, DfNDi recently released the terms of its agreements that proponents of proposals like the APT-A and POVAX might utilise to implement some of its key provisions (Junod Moser et al., Reference Moser D, Boulet, Childs, Shieh and Pecoul2023).Footnote 16
Moreover, the main parts of our proposal are separable and collective procurement may bring great benefits on its own.Footnote 17 UNICEF and regional procurement organisations coordinate a great portion of global medicines' distribution with significant cost savings (Sakane, Reference Sakane2006). In 2015, UNICEF procured approximately 70% of the global vaccine supply (Bare, Reference Bare2015). They offer suppliers long term contracts through competitive bidding and shared production and provide market forecasts, supplying 80–100 countries annually. UNICEF thereby helps address the global vaccine shortage, as many low-income countries lack the resources and bargaining power to secure low prices on vaccines independently (Bare, Reference Bare2015). Other regional and international pooled procurement efforts – from the WHO Procurement Platform and Global Fund’s WAMBO to Pan-Americal Health Organization’s revolving fund, and the African Medicines and Supplies Platform – function in different ways and facilitate lower-price access to quality-assured essential health technologies.Footnote 18
Furthermore, many potential mechanisms for securing and enforcing international agreement on aspects of our proposal exist. One option is for the international community to implement this proposal through the pandemic agreement (World Health Organization, 2022a, 2022b). Incentives for participation might include foreign aid, data/information, technical assistance, policy guidance, and other help with pandemic preparation and response. Side agreements on other matters, might also facilitate a pandemic accord that includes the provisions we have outlined (The Independent Panel for Pandemic Preparedness and Response, 2021). Given that countries not participating in international pandemic preparedness and response mechanisms pose a public health threat, enforcement measures might include restrictions on international travel and transportation (insofar as existing international law is, or can be made, compatible with this suggestion).Footnote 19 The accord could include a council for arbitrating disputes (Nina et al., Reference Nina, Elliot and Susana2024).Footnote 20
Whether countries will sign on to an accord that requires participating in, and fully supporting, a counter-measures platform like the APT-A depends, in part, on its design (Dutton, Reference Dutton2012, 1–66). Investments in research and development, manufacturing, infrastructure and other services can be dual purpose – that is, employed in ways that help meet current health needs and better prepare us to respond well to future pandemics. Through POVAX, we provide a mechanism that will make many of these investments self-sustaining into the future allowing the international community to recoup investment costs through licensing with differential pricing. Moreover, there are significant economies of scale and savings from lower transaction costs in pooled procurement, and both the health and economic costs of future pandemics could be even more devastating than COVID-19 (Bloom and Cadarette, Reference Bloom and Cadarette2019). So, we believe that there is a strong investment case to be made for many aspects of our proposal.
Moreover, we believe states should bind themselves to act according to the rule of law, rather than to exercise political and economic power to promote their own short-term interests, to secure the gains possible from cooperation. The accord should create binding core obligations that ‘define baseline capacities, programs, policies, or capabilities while still allowing countries wide latitude in defining how these activities and operational plans fit into the context of their national priorities and systems’ (Katz et al., Reference Katz, Sorrell, Kornblet and Fischer2014: 231). Countries should establish an international legal mechanism that provides a neutral forum to help resolve disagreements, interpret their legal obligations, and define their rights.Footnote 21 A strong mechanism could guarantee dispute resolution via ‘(1) initial legal opinion, which, if unsatisfactory to one of the parties, could be appealed to an (2) advisory body, which, if also unsatisfactory to one of the parties, could be appealed to an (3) adjudicative body for final resolution’ (Hoffman, Reference Hoffman, Rushton and Youde2014: 10). The WHO's or UN's Chief Legal Officer could provide the necessary legal opinion and state members of the World Health Assembly could elect a sub-committee to the advisory body. Alternately, leaders from the World Health Organization's three governing bodies (the Chair of the Executive Board, President of the World Health Assembly, and Director-General of the Secretariat) could appoint experts to the role. The Permanent Court of Arbitration could appoint members of the final adjudicative body (Hoffman, Reference Hoffman, Rushton and Youde2014: 10). Because appeal is possible (but not mandated) countries have reason to seek a fair resolution to disputes through informal conciliation, negotiation, and mediation.
Moreover, instituting an agreement along the lines suggested above can create reliance on mechanisms embodied in POTAX and help sustain cooperation in pandemic times, yielding benefits into the future. Countries might come to rely on collective procurement efforts as well as technical and other assistance they receive through collaboration and, so, become less likely to defect from an agreement after implementation (LePan, Reference LePan2020). Further, there can be political costs to deviating from a good agreement. Even if it is only possible to sustain cooperation in interpandemic times, the agreement would incentivise companies to provide many essential counter-measures – such as new antibiotics. Moreover, the potential benefits from preventing future pandemics, and having diagnostics, therapeutics, and vaccines available are significant (Ahmadiani and Nikfar, Reference Ahmadiani and Nikfar2016: 1–7).
Our proposal aims to secure everyone's human rights to health by providing a ‘global approach to the development and distribution of vaccines, medicines and treatments based on solidarity and cooperation’ (UN-OHCHR, 2022: 2). Respect for human rights requires that ‘benefits of scientific and technological development …be fairly shared, both within and between nations’ (UN-OHCHR, 2022: 2). More precisely, POTAX provides a concrete mechanism for helping to fulfil individuals' human rights to health by ensuring ‘the availability, accessibility, and quality of diagnostics, medications, vaccines, therapeutics, and other health services’ (Hodgson et al., Reference Hodgson, Habibi, Meier, Sekalala, Seiderman, Falchetta, Schwarz, Tayler, Tait, Staberock and Davis2021). It also provides a mechanism by which the international community might generate sustainable financing for investments that ‘maintain core public health capacities’ as the right requires (Hodgson et al., Reference Hodgson, Habibi, Meier, Sekalala, Seiderman, Falchetta, Schwarz, Tayler, Tait, Staberock and Davis2021). Our proposal's other pillars support ‘universal health coverage and primary health care’ provision and ‘essential health services’ as well as ‘universal, comprehensive, human rights based social protection systems that guarantee at least a basic level of social security for all, over the entire life cycle’ (UN-OHCHR, 2022: 2; Evaborhene et al., Reference Evaborhene, Udokanma, Adebisi, Okorie, Kafuko, Conde, Waliaula and Mburu2023). And we propose governance mechanisms to enhance ‘equity and non-discrimination in pandemic response, participation from affected communities, transparency in government decision-making, and accountability for health outcomes and rights protections,’ as well as financing for investments that ‘maintain core public health capacities’ as the right requires (Hodgson et al., Reference Hodgson, Habibi, Meier, Sekalala, Seiderman, Falchetta, Schwarz, Tayler, Tait, Staberock and Davis2021). They also support the other social, economic, political human rights – the social and structural determinants of health. As the UN points out, respect for human rights requires ‘meaningful, inclusive and safe… participation of all stakeholders from all regions, including civil society organisations, communities and community health workers, in the process’ (UN-OHCHR, 2022: 2).
Consider the potential health and economic benefits of such an agreement. Epidemiological models suggest that equitable COVID-19 vaccine distribution could have halved death rates (Chinazzi et al., Reference Chinazzi, Davis, Dean, Mu, Piontti, Xiong, Halloran, Longini and Vespignani2020; Rotesi et al., Reference Rotesi, Pin, Malik, Paintsil, Bokemper, Willebrand, Huber, Melegaro and Omer2021). Bilateral vaccine deals drove up prices and delayed equitable access, suggesting POTAX could generate significant returns (Callaway, Reference Callaway2020). Some estimate that, in 2020, the COVID-19 crisis cost the world US$ 375 billion monthly and that it will cost the world economy US$ $13.8 trillion through 2024 (UN-OHCHR, 1966; Gopinath, Reference Gopinath2022). Others suggest bilateral deals and competition for scarce vaccines alone cost the world US$1.2 trillion (RAND Corporation, 2020). Implementing alternative reward mechanisms and collective bargaining, sharing research and development data, and reducing transactions and other costs through POTAX may speed up the production of essential countermeasures. Speeding up production even by a few months may make this global collaboration for open access research and development highly cost effective – reducing competition globally for a global public good (Beaton et al., Reference Beaton, Gadomski, Manson and Kok-Chor2021: 285–300).
Some will object that poor countries may rely too heavily on this mechanism and ‘rent seek’ to get access to new technologies they should purchase at full cost, but we believe a global agreement can clearly articulate national, regional, and global obligations that protect everyone's human rights to health. Only when there is insufficient incentive for innovation and high risk do we propose that the international community invest in new technologies' development, procure, and distribute them based on the need to protect everyone's human rights to health. The international community can still recoup investments based on ability to pay. That is, the agreement can require sufficient country, as well as regional and global investments, to prevent free-riding.
In short, our proposal – justified on moral (human right) as well as pragmatic grounds – has the potential to save millions of lives and trillions of dollars. We believe POTAX would benefit even some of the world's richest countries if it accelerates research and development and helps people access essential countermeasures in a timely and equitable manner. In this globally interconnected world, everyone's health as well as economic fortunes are deeply intertwined. The international community must create effective global response mechanisms now as future pandemics may be even more devastating than COVID-19 (The Civil Society and Community Representatives of the ACT-A, 2021).
4. Conclusion
Wealthy nations bought most of the world's COVID-19 diagnostic, therapeutic, and vaccine supply despite having a small proportion of the global population leaving many countries without access to essential health technologies, and even those who could access these technologies often lacked other things they needed to effectively combat the virus (Amnesty International, 2021). Future pandemics may prove much more devastating without global cooperation. We believe that the international community can greatly speed up research, development, and provision of new technologies at low prices if every high-income country joins, and fully supports, the APT-A. The APT-A includes components to address structural inequalities and expand economic support for poor countries as well as provide more funding for vaccines, diagnostics, treatments, access, and basic health systems and these components should be implemented now and ongoing. The proposal can be instituted through the counter-measures platform and the pandemic accord with support from the UN's High-Level process. But, however it is implemented, we believe it is essential to create a truly transparent, and accountable, governance structure. This requires adequate participation from a diverse, global constituency so that the APT-A truly represents the interests of all those affected by pandemic diseases. Part of our proposal is POTAX, which would (1) provide conditional financing for new vaccines and other essential health technologies requiring companies to vest licenses in POTAX and pool intellectual property and other data necessary to allow equitable access to the resulting technologies. It also (2) supports collective procurement as well as measures to ensure equitable distribution and uptake of these technologies. Only by working together can the international community hope to adequately address, and prevent, future pandemics.
Financial support
The Authors would like to thank The Brookings Institution and Helsinki Collegium for Advanced Studie for their support.
Competing interests
None.
Appendix A
Critics charge that ‘unfair vaccine grabs by the governments of some advanced countries’ worsened the COVID-19 pandemic resulting in inequitable access to essential countermeasures (Institute for New Economic Thinking, 2021). Quite apart from the unfairness of this, it may not be in the ultimate self-interest of advanced economies. Why, then, did this happen with the COVID-19 vaccine, and can the international community solve the problem for future pandemics through voluntary action or does the world need some binding international agreement? To understand this challenge, and to get a conditional answer, it is important to sharpen the analysis with some elementary game theory.
Suppose there are n (≥2) high-income countries that are also capable of producing or buying up vaccines for their own population. They are the ‘advanced economies’ that the INET report talks about. Each of these nations has to decide whether to attend solely to the vaccine needs of its own citizens and residents by producing and buying up large amounts (strategy N, N for nationalist) or to buy only an essential amount for its own residents and contribute in some ways to the global effort to provide vaccines in low- and middle-income countries (strategy G, G for global). In order to describe this as a game, we shall use pi to represent country i's payoff function. The payoff earned by country i is determined by the choices made by all n nations. We shall assume that the decisions of low- and middle-income countries do not affect the high-income countries in any serious way.
Here is a partial description of each country i's payoff function. If all nations choose G, let xi denote country i's payoff or well-being. If all nations choose N, let yi denote country i's payoff. And if country i chooses action G, while all other countries choose N, then country i gets a payoff of zi. Further, we assume xi > yi > zi, for every country i.
In essence what we are saying is that, if all advanced economies choose to share vaccines with the poorer economies, that is, choose G, each of them would be better off than if no one shared vaccines, that is, each followed the vaccine nationalism agenda, N. The reason for this was increasingly clear in the COVID-19 pandemic as the virus kept on mutating and new strains made an appearance. In any serious future pandemic, short of a total travel ban that will have a devastating economic cost, this will keep happening without a robust global effort, which basically means a concerted effort by virtually all advanced economies. As the INET (2021) report notes, ‘Delayed vaccination of people across the world increases possibilities of virus mutation, reducing the ability to control the virus even in rich countries that have bagged the vaccines’ (Institute for New Economic Thinking, 2021). This is summed up by the inequality xi > yi, for every country i.
The payoff function described above also says that if every other nation is following the nationalist policy N, for one to be generous and global, that is, choosing G, is not in its self-interest. That way, this one nation will use some of its own resources to help other poor nations. That will, of course, be good for the poor nations, but that is unlikely to be enough to stop the virus surviving and possibly mutating elsewhere. You need more of a concerted effort across nations for that to happen.
Note that the above description does not fully specify nation i's payoff function. It does not, for instance, tell us what happens to nation i if all other nations choose G and nation i chooses N, or (assuming there are 4 or more rich nations), if half or half plus one of all the nations choose N, and the remaining nations choose G. We have deliberately kept the payoff function partially defined because we simply do not, at this stage, know the outcomes of all possible scenarios. Much more research involving epidemiology (how easily a virus multiplies and how it affects the infected person), physics (how the virus is transmitted and how easily) and economics (how people behave in terms of wearing masks and socialising and interacting with one another etc) is necessary to determine these payoffs.
Another reason for leaving a part of the payoff function unspecified is that there will be differences between the returns and externalities of what smaller nations, such as Switzerland, Belgium and Singapore, do and what larger nations, such as the United States, Russia and China, do. For some of the detailed specification of a global convention we will have to take account of these size asymmetries.
In the context of the present paper what is interesting is that even with this partial specification we can begin to describe some of the implications of vaccine policy. We can see that each nation choosing to be inward looking, that is, choosing strategy N, is a Nash equilibrium. No nation can do better by unilaterally deviating.
But is each nation taking on some global responsibility (action G) an equilibrium? From the description of the partial payoff function above, we do not know. We know that everybody choosing G would make everybody better off than the case where everybody chooses N, but we do not know if that good state is sustainable as an equilibrium. If we use wi to denote the payoff nation i earns when all other nations choose G and nation i chooses N, then it all depends on the relation between wi and xi. If wi > xi, the game the nations are playing is like a Prisoner's Dilemma; and if wi < xi, the game is akin to what Sen (Reference Sen1967) had called the Assurance Game, which is a special kind of coordination game.
In either case, the nations acting in some kind of concert can deliver benefits to each one of them. This is true for a lot of fiscal and monetary policy initiatives. The effect can be very different when nations act in concert and when they move unilaterally. This is also true for the sharing of necessities, like vaccines and medicines (Sen, Reference Sen1967).
It may be pointed out that even concerning good socially responsible individual behavior during a pandemic, such as not gathering in certain kinds of venues, there can be interesting applications of the Assurance Game which show how making certain predictions concerning the spread of the virus associated with certain kinds of behavior can be self-fulfilling.
This argument becomes even more clear if we consider a special case. Suppose there are just 2 advanced economies (N = 2), and xi = 8, yi = 6 and zi = 4 (so condition 2 above is satisfied). Then this game can be represented as a standard 2-by-2 payoff matrix, as shown below (Table A1).
Table A1. The vaccine sharing game
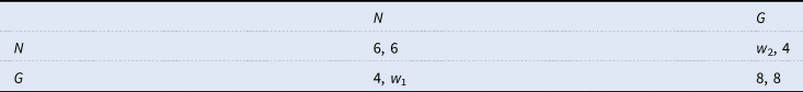
Clearly (N, N) is an equilibrium. If country 1, that is, the one choosing between the columns, shifts unilaterally to G, it will get 4 instead of 6. If country 2 chooses G it will get 4. Hence, neither will want to move, making (N, N) a Nash equilibrium. (G, G) is a superior outcome, but it may or may not be an equilibrium. That depends on the value of w 1 and w 2. If both of these are less than or equal to 8, then (G, G) is an equilibrium. Otherwise not. But even with this partial information, it is arguable that the international community should try to shift away from the ‘vaccine grab equilibrium’ to the ‘sharing outcome’ (G, G). If the sharing outcome is a Nash equilibrium, all we would need to do is to somehow get there. No further global action is needed. If, however, the ‘sharing outcome’ is not an equilibrium, we need some kind of multilateral agreement to hold countries to the vaccine sharing arrangement.
Since we do not know if (G, G) is an equilibrium but we do know it is the good outcome and it is also clear that in case it is an equilibrium, having an agreement to hold countries there will be redundant but do no harm, a multilateral agreement is the right strategy to use. That is what we are arguing for in this paper.
What we have not gone into here is the fact that a nation's pandemic related interventions are invariably intertwined with economic policies and other political considerations. If this inter-connection were to be modelled, the game would be more complicated but it is arguable that the case for policy coordination across nations would be even stronger.
Appendix B
These are cost estimates for counter-measures of development for 40 potential pathogens and distributing a vaccine.
Table B1. Estimated APT-A Financing Needs: R&D, Manufacturing, Distribution and Stimulus Estimates – High and Low Bound (in Billions USD)Footnote 22

Appendix C
To implement our proposal within the current (April 18) draft of the pandemic agreement currently under negotiation at the World Health Assembly (WHO, 2024), we recommend the following:
Parties should strengthen Article 9 to better reflect our commitment to global health equity and preparedness revising the current language to more explicitly emphasize not only the sustained investment in the research and development (R&D) of public health priorities, including pandemic-related products, but also to guarantee equitable access to, and delivery of, essential countermeasures in middle-income, as well as low-income, countries: Licenses to intellectual property, data, and knowledge necessary to produce and distribute essential countermeasures globally should be vested in the WHO.
Parties should strengthen Article 11 to implement intellectual property waivers for essential health technologies in pandemic times and require companies to share their intellectual property, data, and know-how.
Parties should strengthen language around the Global Supply Chain and Logistics Network (the Network) in Article 13 to require expanding collective procurement efforts. Developed as well as developing countries should commit to utilising collective procurement through the network in inter-pandemic as well as pandemic times. National procurement should be limited, insofar as possible, to only the resources not available through collective procurement efforts.
Parties should strengthen Article 6 and 7 to provide significant international financing for investments in manufacturing, distribution, and basic health systems including investments in infrastructure, workforce development, disease surveillance, universal healthcare systems, and technology transfer initiatives. Investments in infrastructure, workforce development, disease surveillance, universal healthcare systems, and technology transfer initiatives must be sufficient to ensure timely, and equitable, distribution of countermeasures in pandemic times and to ensure for all the social and structural determinants of health.
Although the PABs system may generate some funds, and should arguably require manufacturers to provide much larger real-time contributions, parties should strengthen Article 20 to include specific assessed financing contributions and detail a mechanism for recouping costs and supporting investments in health systems, manufacturing, and distribution, as well as research and development.
In Article 20 or a new article, parties should also commit to providing significant economic support that goes beyond debt cancellation to protect the most vulnerable in low- and middle-income countries (LMICs) and aid LMICs in economic recovery.
Parties should strengthen Article 25's dispute resolution mechanism to implement a council for arbitrating disputes.
Throughout the agreement, it is essential to strengthen the language so as to require the outlined investments, improvements, and measures. All parties should have clearly defined international obligations to ensure sufficient technology transfer, utilise collective procurement, provide adequate financing, and invest in the development of well-functioning basic health systems with sufficient workforce training and deployment globally. For instance, all countries should require (not just facilitate, promote, consider, or encourage voluntary) technology transfer necessary for the development of essential countermeasures from both public and private sector developers. Similarly, LMICs require significant international support to improve basic health infrastructure and capacities. The accord should prohibit reservations to all the articles of the agreement necessary to implement the recommendations we outline.Footnote 23







