Introduction
The newly incepted Coronavirus Disease 2019 (COVID-19) pandemic has become the most challenging global issue. This contagious disease has already spread out within all countries and territories worldwide after its first appearance in late December 2019 at Wuhan, China, caused by a newly discovered virus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Puspitasari et al., Reference Puspitasari, Yusuf, Sinuraya, Abdulah and Koyama2020). Regardless of the unpredictable and uncontrolled situation of the viral infection, the World Health Organization declared this outbreak as a pandemic on 11 March 2020 (BBC News, 2020; Puspitasari et al., Reference Puspitasari, Yusuf, Sinuraya, Abdulah and Koyama2020). Consequently, approximately 577K cases had been infected with the virus on 23 March 2021, with 8720 deaths in Bangladesh.
People infected with the SARS-CoV-2 manifest both symptomatic and asymptomatic signs and symptoms, including fever, cough, fatigue, headache, myalgia, muscle pain, breath shortness, acute upper respiratory tract distress, diarrhea, etc. (CDC, 2020; Chen et al., Reference Chen, Zhou, Dong, Qu, Gong, Han, Qiu, Wang, Liu and Wei2020). Even though an individual is not infected with SARS-CoV-2, the higher rates of COVID-19-related infection and mortality have an impact on their quality of life, leading to a worsening psychological state. Moreover, to alleviate this contagious outbreak at the community level, some of the non-therapeutic public health interventions were implemented globally, including countrywide lockdown, home or institution-based isolation or quarantine, shutting down all kinds of public activities along with closing educational institutions, especially restriction in social and community movements, etc. (Dsouza et al., Reference Dsouza, Quadros, Hyderabadwala and Mamun2020; Gualano et al., Reference Gualano, Lo Moro, Voglino, Bert and Siliquini2020). Prior research found that people subjected to these measures experienced significant mental health consequences, which led to people disliking the importance of social restriction measures aimed at suppressing viral infection (Hawryluck et al., Reference Hawryluck, Gold, Robinson, Pogorski, Galea and Styra2004).
In Bangladesh, the first COVID-19 case was identified on 8 March 2020 (Anwar et al., Reference Anwar, Nasrullah and Hosen2020). After some of that point time, the authority of Bangladesh seized countrywide lockdown with the title of ‘general holidays’ to mitigate the outbreak at the community level, which was a significant challenge for a lower- and middle-income country with limited resources in the healthcare settings (Anwar et al., Reference Anwar, Nasrullah and Hosen2020). Under these circumstances, many people were laid off or became unemployed, with no hope of finding new employment (Bhuiyan et al., Reference Bhuiyan, Sakib, Pakpour, Griffiths and Mamun2020). Consequently, the jobless situation led people to suffer from higher rates of mental instabilities (Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020). Due to mental problems related to unemployment and economic crisis, self-harm and suicidal incidences are also observed in Bangladesh. For instance, a study reported that all but one of the COVID-19-related suicide cases occurred as of economic and financial problems within the first 3 weeks of April 2020 (Bhuiyan et al., Reference Bhuiyan, Sakib, Pakpour, Griffiths and Mamun2020). In addition, the uncertainty about going back to everyday life, fear of being infected, social and economic disruption, rising social negligence, difficulties in getting proper treatment as of the overwhelming number of patients, etc., generally increase psychological suffering, including post-traumatic stress disorder (PTSD), insomnia, phobia, fear, anxiety, depression, etc. (Hossain et al., Reference Hossain, Rahman, Trisha, Tasnim, Nuzhath, Hasan, Clark, Das, McKyer and Ahmed2020a; Sundarasen et al., Reference Sundarasen, Chinna, Kamaludin, Nurunnabi, Baloch, Khoshaim, Hossain and Sukayt2020; World Health Organization, 2020).
In Bangladesh, after the first COVID-19 suicide incidence on 25 March 2020, epidemiological studies concerning mental health problems to identify risky individuals were recommended (Mamun and Griffiths, Reference Mamun and Griffiths2020), and many studies have already been conducted across the country. But there is no beyond a systematic evaluation to better understand the impact of the COVID-19 pandemic on people's psychological health. Therefore, this is the first systematic attempt to review Bangladeshi studies on COVID-19 pandemic-related mental health problems such as depression, anxiety, and stress. This systematic review and meta-analysis included those Bangladeshi studies reported mental health outcomes' prevalence and/or associated factors, and the findings reported herein are anticipated to be useful in facilitating appropriate mental health strategies.
Methods
Search strategies
For conducting a systematic review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2010) adhered to the present review (PRISMA 2020 checklist is provided in the online Supplementary File). Literature searches were conducted between 20 December 2020 and 5 March 2021, using a group of bounded keywords in the relevant databases. The searching keywords included three types of items, (i) exposure (e.g. ‘COVID-19’, ‘Coronavirus’, SARS-Cov-2, ‘COVID-19 pandemic’), (ii) outcome of interest (e.g. ‘mental health’, ‘depression, anxiety and stress’, ‘psychological impact’, ‘depressive disorders’, ‘depression’, ‘anxiety disorder’, ‘anxiety’, ‘stress’, ‘stress disorders’), and (iii) country (e.g. ‘Bangladesh’). The searches were conducted with the combination of these three types of keywords.
Data eligibility criteria
For being included in the present review, every article must fulfill the following requirement of (i) being a Bangladeshi study, (ii) being conducted after the inception of the COVID-19 pandemic, (iii) being an observational study (cross-sectional or longitudinal) in nature, (iv) being concerned with at least one common mental health problem (i.e. PTSD or stress, depression, and anxiety), (v) reporting the prevalence and/or risk factors of these disorders, (vi) being published in peer-reviewed journals or preprint servers, (vii) being published in the English language.
Data collection procedure
First of all, a comprehensive literature search was conducted using the databases of Medline or PubMed to identify articles related to the prevalence and/or associated factors of depression, anxiety and stress reported during the COVID-19 pandemic in Bangladesh. Later on, Scopus, PsycINFO, Web of Science, CINAHL, Google Scholar, and ResearchGate were used to retrieve missing peer-reviewed articles. Additionally, preprint servers such as PsyArxiv and MedRxiv were also searched to find relevant articles. Therefore, after a preliminary search conducted by the principal investigator, other investigators subsequently re-circled the procedure to ensure articles were not excluded from this review. As a result, a total of 175 articles were identified, whereas the ‘titles and abstracts’ of the retrieved articles were scanned to adhere to the study inclusion criteria of the present review. To the end, a total of 24 articles were included in this review after confirming all of the requirements (Fig. 1).

Fig. 1. PRISMA flow diagram.
Data extraction
In Microsoft Excel, a data extraction file was designed to make necessary changes from the recruited articles. After that, data were demonstrated by following records: information about the author and publication year, study design, sampling and data collection method, specific group and sample size, time for data collection, assessments tool along with cutoff value and the prevalence and risk factors of PTSD, stress, depression, and anxiety by the principal investigator. Finally, after the independent investigation and cross-checking by all the investigators, the disagreements were solved in the final file, as presented in Table 1.
Table 1. Characteristics of the included literature in the present review
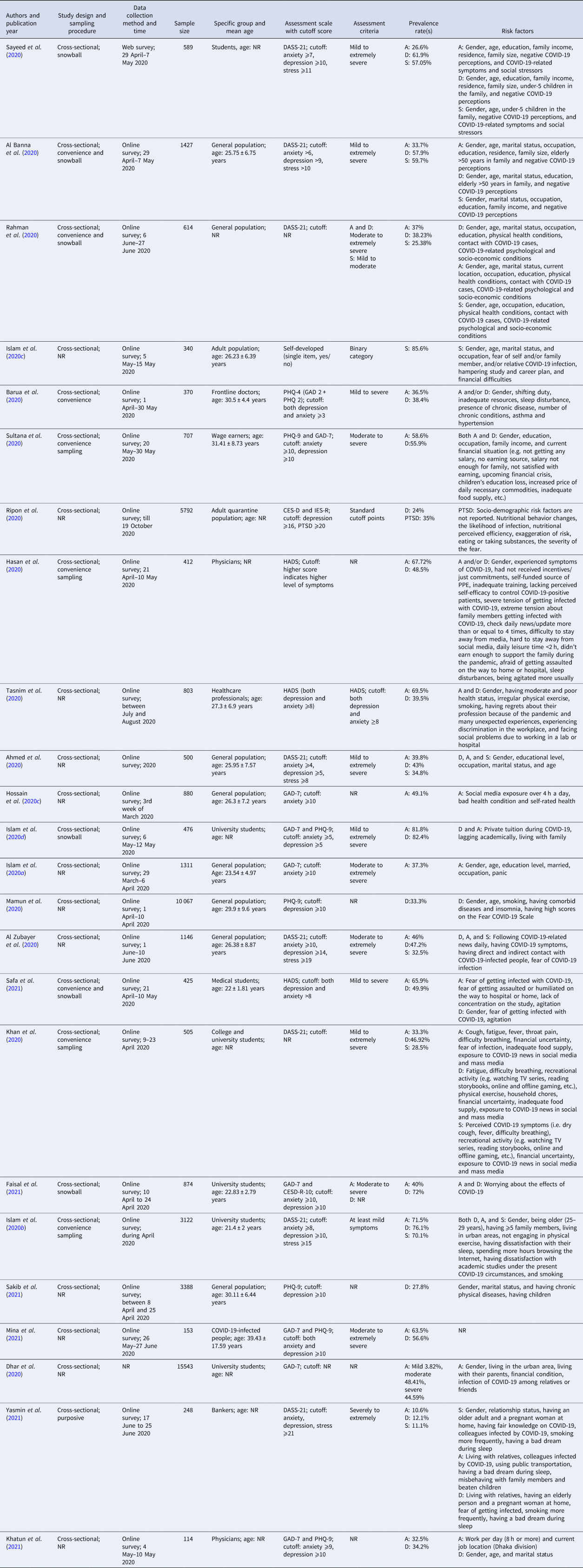
A, anxiety; D, depression; S, stress; PTSD, post-traumatic stress disorders; NR, not reported; HADS, Hospital Anxiety and Depression Scale; DASS-21, Depression, Anxiety, Stress Scale 21; IES-R, Impact of Event Scale-Revised; CES-D, Center for Epidemiologic Studies-Depression; MDD, major depressive disorder; CESD-R-10, Center for Epidemiologic Studies Depression Scale-Revised.
Quality assessment of the included studies
The risk of bias of the included studies was assessed by The Joanna Briggs Institute (JBI) checklist used for prevalence studies. The JBI uses a four-point Likert scale with answers being ‘no’, ‘yes’, ‘unclear’, or ‘not applicable’, for the following questions: (1) appropriateness of the sample frame (Was the sample frame appropriate to address the target population?); (2) recruitment procedure (Were study participants sampled in an appropriate way?); (3) adequacy of the sample size (Was the sample size adequate?); (4) description of subjects and setting (Were the study subjects and the setting described in detail?); (5) description of the identified sample (Was the data analysis conducted with sufficient coverage of the identified sample?); (6) validity of the methods used to screen for mental health problems (Were valid methods used for the identification of the mental health problems?); (7) reliability of the methods used to screen for mental health problems (Were the mental health problems measured in a standard, reliable way for all participants?); (8) adequacy of statistical analyses (Was there appropriate statistical analysis?); and (9) response rate (Was the response rate adequate, and if not, was the low response rate managed appropriately?). Articles were assigned one point per yes. Details of the quality assessment criteria can be found in the online Supplementary Materials.
Statistical analysis
Random-effect models were used in the study, assuming significant heterogeneity in all of the studies. The heterogeneity estimated of the effect of the sample size was calculated as I 2 statistic. I 2 values of <25, 25–75, and 75% or more indicated low, moderate, and substantial heterogeneity, respectively. Cochran's Q test and τ 2 statistics were used to assess the heterogeneity between studies. Subgroup analysis was performed based on the specific population group in the study. The results are presented in Forest plots as an estimate with a 95% confidence interval. The publication was assessed using the funnel plots to show the biasness graphically. In addition, Egger's test was applied for rigorous assessment of publication bias. Subgroup analysis was presented if there were three or more studies available for analysis. All the analysis was conducted using the STATA software version 16.
Results
General description of the included studies
A total of 24 studies were encompassed in the present review, whereas a total of 49 806 respondents participated autonomously, including a range of sample size 114–15 543; whereas the mean age of the participants ranged between 21.4 (±2) and 31.41 (±8.73) years. All of the included studies were cross-sectional and were conducted through online media and platforms. Most studies were surveyed among general population (n = 9) including different cohorts, e.g. students (n = 7), healthcare professionals (n = 4), quarantined individuals (n = 1), wage-earners (n = 1), SARS-CoV-2 infected individuals (n = 1), and bankers (n = 1). In addition, utmost participants belonged to younger adult age groups. Details of the included study description can be found in Table 1.
Measurements used in the included studies
Different asessment tools were used to detect mental health problems, whereas most studies utilized the DASS-21 (n = 7). There are also disparities in the prevalence cutoff values; that is, some of the studies (n = 8) considered ‘mild to severe or extremely severe conditions’ for identifying prevalence rates, whereas ‘moderate to severe or extremely severe’ in six studies, and nine studies did not report (or self-considered) the cutoff points. The description of the recruited articles' measurement use can be found in Table 1.
Overall prevalence of depression, anxiety, and stress
Prevalence of depression was reported in a total of 20 studies, the pooled estimated prevalence was 47% (95% CI 39–55%, I 2 = 99.14%) (Fig. 2). Higher rates of depression were reported among the university student's cohort (82.4%), and lower rates were reported for bankers (i.e. 12.1%). Where the prevalence of anxiety was reported among 20 studies, the pooled estimated prevalence was 47% (95% CI 39–54%, I 2 = 99.78%) (Fig. 3). Higher rates of anxiety (81.8%) were observed among university students, whereas the rate was lower for bankers (10.6%). A total of ten studies reported the prevalence of stress, the pooled estimated prevalence was 44% (95% CI 30–58%, I 2 = 99.36%) (Fig. 4). General people reported a higher level of stress (85.6%), whereas lower was reported among the bankers (11.1%).
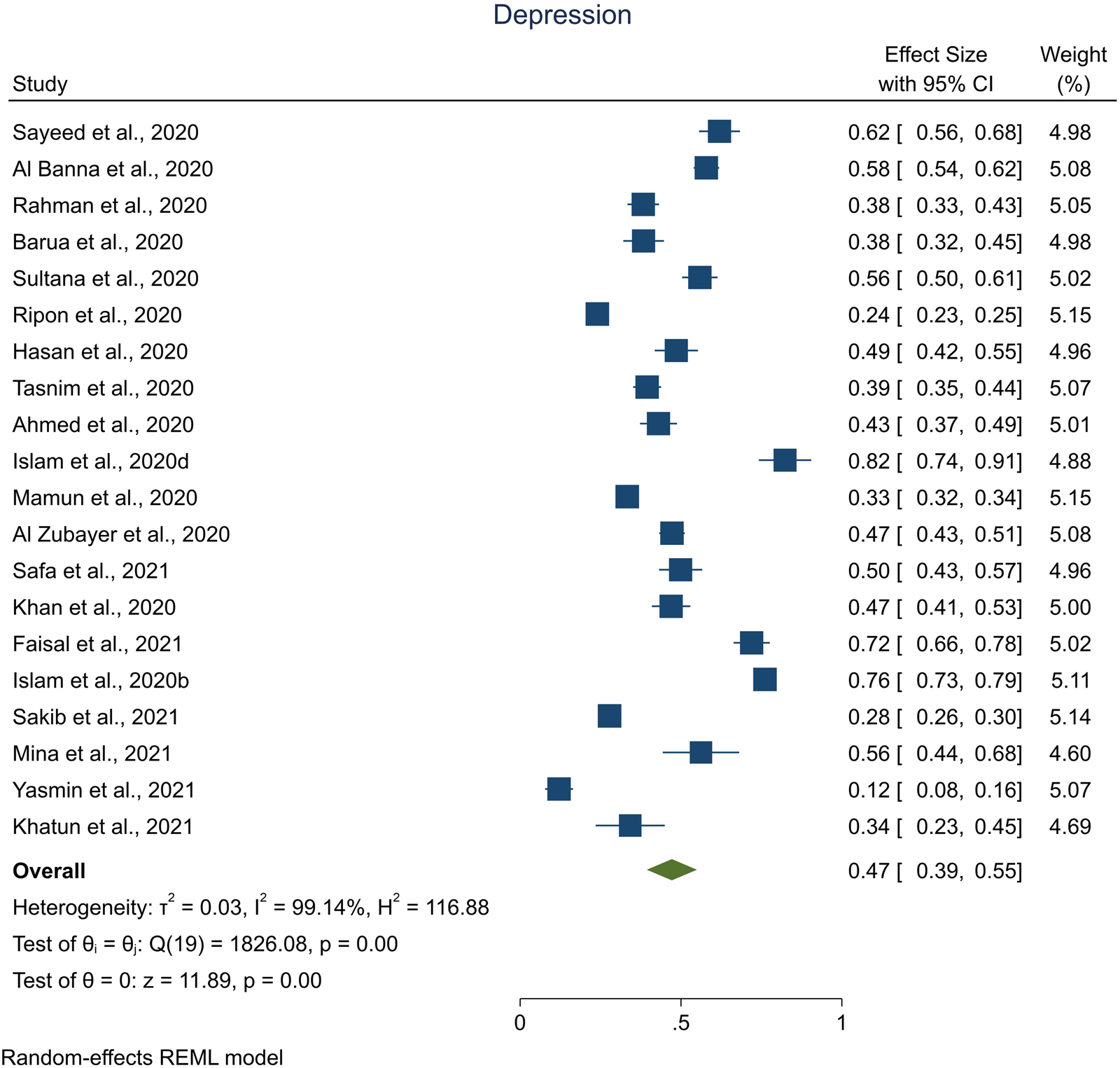
Fig. 2. Pooled prevalence of depression.
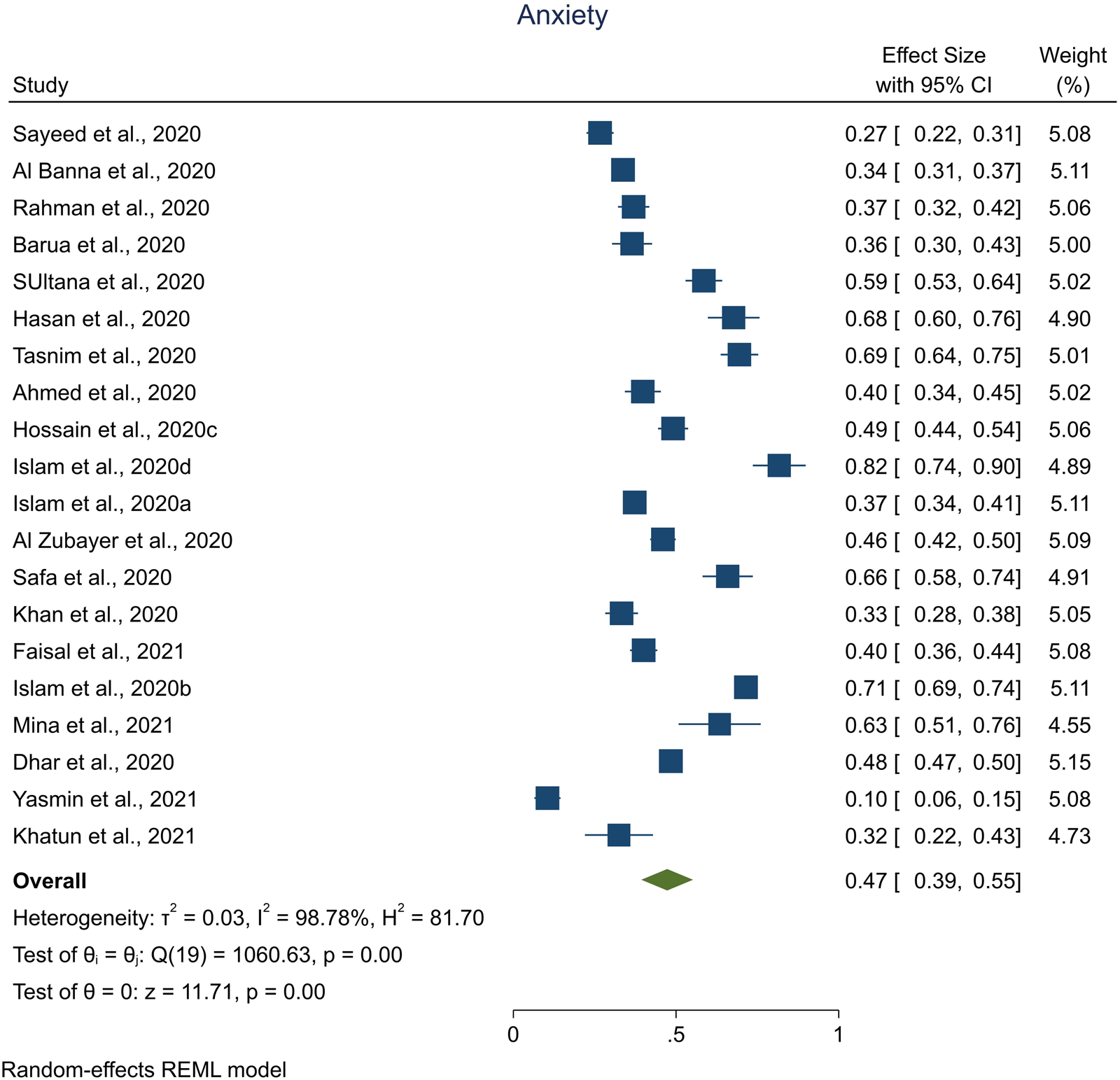
Fig. 3. Pooled prevalence of anxiety.
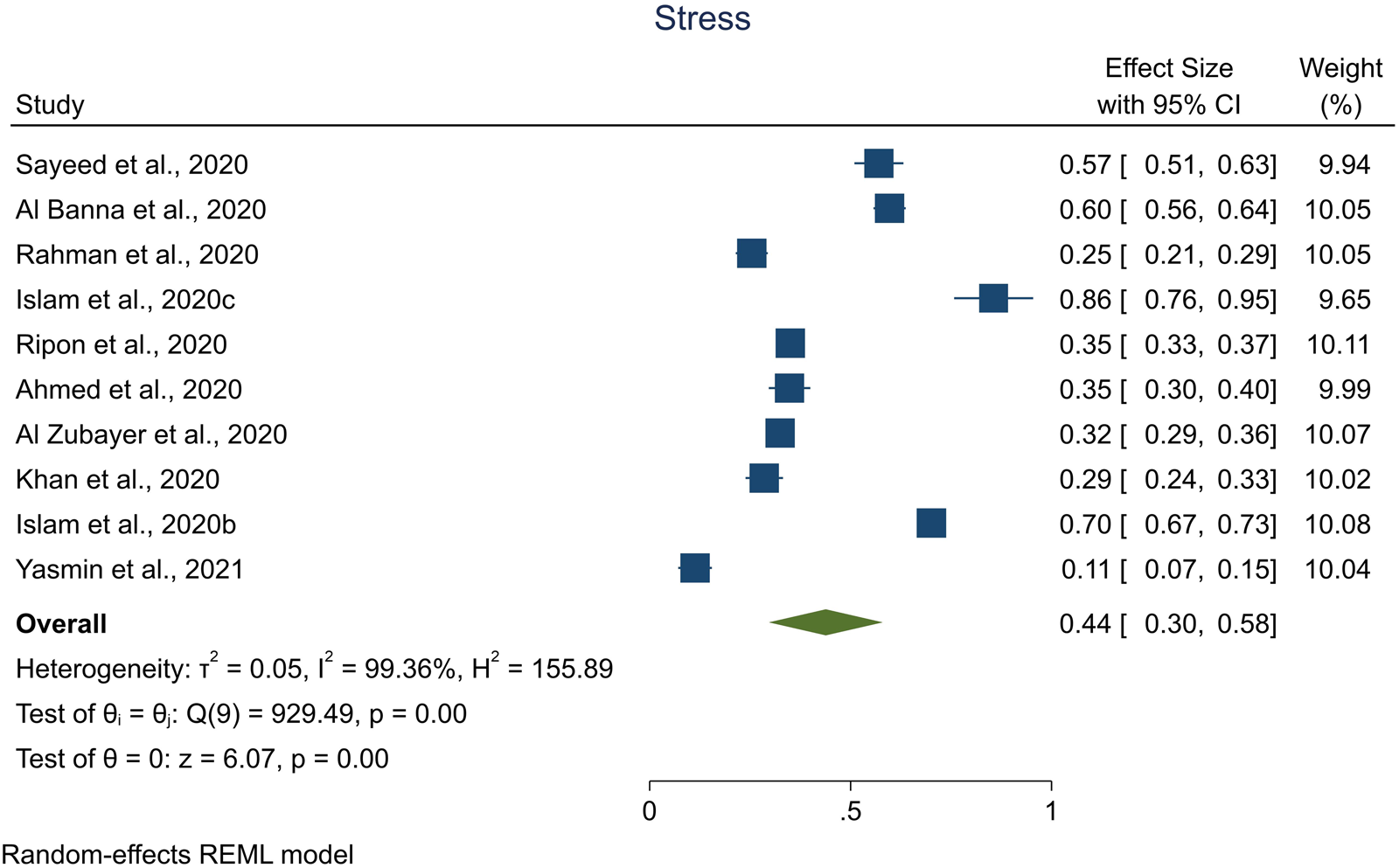
Fig. 4. Pooled prevalence of stress.
Group-specific prevalence of depression, anxiety, and stress
Subgroup analysis was graphically presented using Forest plots. Please refer to the online Supplementary Materials. Here, subgroup analysis was presented if the number of available studies was 3 or more.
Prevalence of depression, anxiety, and stress: general population
Subgroup analysis of the general people against depression, anxiety, and stress was shown in Table 2. The results showed that the overall pooled prevalence of depression was 41% (95% CI 33–50%, I 2 = 98.46%). For anxiety, the overall estimated pooled prevalence was 40% (95% CI 36–45%, I 2 = 88.10%). Furthermore, for stress, the overall prevalence was 38% (95% CI 23–53%, I 2 = 98.11%).
Table 2. Subgroup analysis of specific group in terms of depression, anxiety, and stress
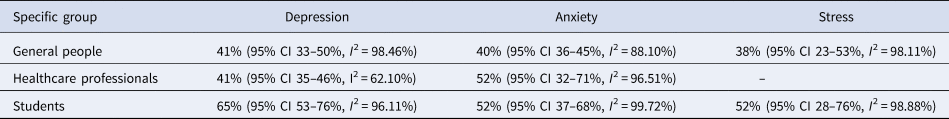
Prevalence of depression, anxiety, and stress: healthcare professionals
Subgroup analysis by a specific group in terms of depression, anxiety, and stress was presented in Table 2. The overall prevalence of depression was 41% (95% CI 35–46%, I 2 = 62.10%). Whereas it was 52% (95% CI 32–71%, I 2 = 96.51%) for anxiety.
Prevalence of depression, anxiety, and stress: students
Table 2 visualized the subgroup analysis of students in terms of depression, anxiety, and stress. Overall estimated prevalence of depression was 65% (95% CI 53–76%, I 2 = 96.11%). Similarly, for anxiety and stress, the pooled prevalence was 52% (95% CI 37–68%, I 2 = 99.72%) and 52% (95% CI 28–76%, I 2 = 98.88%), respectively.
Prevalence of depression, anxiety, and stress: bankers
During the COVID-19 pandemic, banks were not closed down, which might influence the bankers attaining higher mental health problems as they had to go to banks through public transportation mostly. Therefore, fear of being infected also increases their risk of being affected mentally. Nevertheless, only a study was directed among bankers regarding the level of anxiety, depression, and stress, which includes 10.6, 12.1, and 11.1%, respectively; the lowest prevalence rates as identified across all of the cohorts included in this review (Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021).
Prevalence of depression, anxiety, and stress: quarantined people
Quarantine or restriction of movement had been introduced to switch the transmission of SARS-CoV-2 during the COVID-19 pandemic, wherever strategies associated with quarantine were constantly washing hands, wearing masks, and departing to the hospital when experiencing any complications related to COVID-19 symptoms (Ripon et al., Reference Ripon, El-Sabban, Sikder, Hossain, Mim, Ahmed and Mehta2020). Nevertheless, these effective measures had been reported to psychologically impact the quarantined people by evolving personalized trauma, fear, and uncertainty of their natural life, etc. However, following the situation, only a study was conducted among the quarantined people, whereas the quarantined people reported experiencing 24% and 35% depression and PTSD, respectively (Ripon et al., Reference Ripon, El-Sabban, Sikder, Hossain, Mim, Ahmed and Mehta2020).
Prevalence of depression, anxiety, and stress: wage-earners
As of the COVID-19-related lockdown (e.g. movement restriction and earning losses), the wage-earning people became unable to bear the basic family needs, which effect on them being psychologically more vulnerable. Thus, as reported in a study, higher mental health problems were reported to this cohort; that is, 58.6% and 55.9% were the prevalence of anxiety and depression (Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020).
Prevalence of depression, anxiety, and stress: COVID-19-infected people
People infected with the COVID-19 generally experience a higher level of psychological problems, including depression and anxiety as a fear of mortality. Higher mental health problems were observed in this group as a vulnerable cohort, e.g. 63.5% and 56.6% for anxiety and depression. Hence, only a study was directed among this vulnerable cohort (Mina et al., Reference Mina, Billah, Karmakar, Das, Rahman, Hasan and Acharjee2021).
Risk factors associated with depression, anxiety, and stress
The risk factors for common mental health problems can be divided into three major categories, that is, (i) socio-demographic, (ii) behavior and health, and (iii) COVID-19-related risk factors. The basic socio-demographic risk factors included age, gender, family income, marital status, education, residence and family type, and having elderly and children in the family. In contrast, the behavior and health-related risk factors were smoking and alcohol use, social media exposure, physical exercise, physical health conditions, and psychological conditions. Finally, COVID-19-related risk factors included insufficient protective resources, COVID-19-related perceptions, fear of COVID-19 infection, experiencing COVID-19-related symptoms, being suspected/infected with the COVID-19, being contacted with the COVID-19 cases, being quarantined or isolated, etc.
Socio-demographic risk factors
Age
Age had been found significant in several studies that influenced mental health consequences (Ahmed et al., Reference Ahmed, Ahmed, Alim, Khan and Jobe2020; Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020; Islam et al., Reference Islam, Ferdous and Potenza2020a, Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b, Reference Islam, Bodrud-Doza, Khan, Haque and Mamun2020c; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020; Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020; Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020; Khatun et al., Reference Khatun, Parvin, Rashid, Alam, Talukder, Razu, Ward and Ali2021). Whereas Sayeed et al. (Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020) found participants' age ≤22 years were at 4.49, 4.46, and threefold higher risk of developing depression, anxiety, and stress respectively than age more than 22 years. However, another study reported that being aged between 24 and 39 than ⩾40 years had a lower risk of being anxious, but those aged ⩽23 years compared to ⩾40 years had experienced higher depressive symptoms (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020). Similarly, Mamun et al. (Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020) reported that younger people develop depressive symptoms mostly. Besides, Islam et al. (Reference Islam, Ferdous and Potenza2020a) found that participants aged 13–20 and 21–30 years were at a lower risk of anxiety than more than 30 years. Another study reported that participants' being younger were at greater risk of developing psychological sufferings (Islam et al., Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b). Furthermore, respondents aged below 25 years were approximately 2.29 times more prone to depression suffering than those more than 35 years old (Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020). The included studies to this review randomly utilized different age ranges; hence, concluding age-based mental health risk factors can be limited.
Gender
Gender was found to be a significant predictor of mental health problems in a large number of studies (Ahmed et al., Reference Ahmed, Ahmed, Alim, Khan and Jobe2020; Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020; Barua et al., Reference Barua, Zaman, Omi and Faruque2020; Dhar et al., Reference Dhar, Ayittey and Sarkar2020; Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020; Islam et al., Reference Islam, Ferdous and Potenza2020a, Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b, Reference Islam, Bodrud-Doza, Khan, Haque and Mamun2020c; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020; Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020; Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020; Tasnim et al., Reference Tasnim, Sujan, Islam, Ritu, Siddique, Toma, Nowshin, Hasan, Hossain and Nahar2020; Khatun et al., Reference Khatun, Parvin, Rashid, Alam, Talukder, Razu, Ward and Ali2021; Safa et al., Reference Safa, Anjum, Hossain, Trisa, Alam, Abdur Rafi, Podder, Koly, Azad, Ahmad, Nodi, Ashraf, Quamrul Akhter, Ahmed and Hasan2021; Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021; Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021). For example, a study found that females were suffering mostly from depression, anxiety, and stress, respectively, where it was 3.4, 3.4, and 4.5 times higher than males (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020). Similarly, Al Banna et al. (Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020) reported that male participants were reported significantly less vulnerable to stress, anxiety, and depression. Consistent with this, other studies also confirmed that female participants were at greater risk of those sufferings (Ahmed et al., Reference Ahmed, Ahmed, Alim, Khan and Jobe2020; Islam et al., Reference Islam, Ferdous and Potenza2020a; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020; Tasnim et al., Reference Tasnim, Sujan, Islam, Ritu, Siddique, Toma, Nowshin, Hasan, Hossain and Nahar2020; Safa et al., Reference Safa, Anjum, Hossain, Trisa, Alam, Abdur Rafi, Podder, Koly, Azad, Ahmad, Nodi, Ashraf, Quamrul Akhter, Ahmed and Hasan2021). However, no studies considered transgender concerning mental health in Bangladesh; although Mamun et al. (Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020) collected data on it, transgender was excluded from the analyses concerning the presentation of mental health problems.
Family monthly income
Only two studies found family income as a significant factor in psychological sufferings (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020; Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020). Participants' monthly family income ⩽2 7000 BDT [Bangladeshi Taka (currency)] was at approximately 2.56- and 2.62-folds higher risk of developing anxiety and depressive symptoms, respectively, than ⩾27 000 BDT (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020). However, another study concerning the wage-earning participants reported that the average monthly family income to be associated with both symptoms of anxiety and depression; that is, 3.31 and 4.12 times higher risk, respectively, were observed for less than 30 000 BDT compared to more than 70 000 BDT (Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020).
Marital status
Marital status had been found significant in a total of six studies (Ahmed et al., Reference Ahmed, Ahmed, Alim, Khan and Jobe2020; Islam et al., Reference Islam, Ferdous and Potenza2020a, Reference Islam, Bodrud-Doza, Khan, Haque and Mamun2020c; Khatun et al., Reference Khatun, Parvin, Rashid, Alam, Talukder, Razu, Ward and Ali2021; Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021; Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021), which depicted that a married person was at approximately two times higher risk of suffering from anxiety than an unmarried person (Islam et al., Reference Islam, Ferdous and Potenza2020a). But heterogeneity of depression rate distribution with marital status was also found in a comparative study among the general population and healthcare professionals; that is, the divorced participants reported the highest depression rate followed by those who were unmarried and married (53.5, 33.6, and 23.7%, respectively) (Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021). Similarly, physicians are either unmarried, divorced, widowed, or separated compared to married ones experiencing three times higher depressive symptoms (Khatun et al., Reference Khatun, Parvin, Rashid, Alam, Talukder, Razu, Ward and Ali2021).
Education
Education has been a significant factor for depression, anxiety, and stress in some of the studies (Ahmed et al., Reference Ahmed, Ahmed, Alim, Khan and Jobe2020; Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020; Islam et al., Reference Islam, Ferdous and Potenza2020a; Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020; Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020; Yeasmin et al., Reference Yeasmin, Banik, Hossain, Hossain, Mahumud, Salma and Hossain2020). A study claimed that higher secondary and undergraduate education participants were at less risk of stress than the graduate (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020). Contradictorily, respondents with secondary and undergraduate education were approximately 12.87- and 1.12-fold times higher risk of anxiety symptoms than the graduates (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020). Additionally, the secondary education cohort was at a 2.30 times higher risk of suffering from depression than the graduates (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020). Another study reported that participants with higher secondary education were more prone to develop depression and anxiety (Ahmed et al., Reference Ahmed, Ahmed, Alim, Khan and Jobe2020). Anxiety symptoms were less in having intermediate (11th–12th grade) education (about 0.5 times) and having bachelor education (approximately 0.64 times) than those with having higher education (above bachelor) (Islam et al., Reference Islam, Ferdous and Potenza2020a).
Residence and family size
Living areas and the size of families were independently found as the risk factors for mental health suffering among individuals (Dhar et al., Reference Dhar, Ayittey and Sarkar2020; Islam et al., Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020; Yeasmin et al., Reference Yeasmin, Banik, Hossain, Hossain, Mahumud, Salma and Hossain2020). For example, living in an urban area and families with more than five members reported having significant psychological issues (Dhar et al., Reference Dhar, Ayittey and Sarkar2020; Islam et al., Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b; Yeasmin et al., Reference Yeasmin, Banik, Hossain, Hossain, Mahumud, Salma and Hossain2020). In contrast, another study reported that having children less than five in a family experienced more mental health outcomes (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020).
Having elderly and children in the family
Having elderly and children in the family increase the risk of mental health problems (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020; Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021). For instance, student participants having children <5 years in the family had experienced higher levels of depression and stress (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020). Similarly, other studies reported that elderly >50 years old in the participants' families who were at an increased risk of COVID-19 experienced higher anxiety and depression symptoms (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Dola, Hassan, Chowdhury and Khan2020; Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021).
Behavior and health-related risk factors
Smoking and alcohol use
Smoking and alcohol use significantly influenced the risk of mental health problems such as stress, depression, and anxiety in a few studies (Islam et al., Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020; Tasnim et al., Reference Tasnim, Sujan, Islam, Ritu, Siddique, Toma, Nowshin, Hasan, Hossain and Nahar2020; Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021). For example, Mamun et al. (Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020) reported that 15.6% of the participants were depressed who were involved with smoking, whereas this rate was 3.3% for alcohol users. Besides, another study reported that those who were smoking more frequently significantly experienced a high score for stress and depression (Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021).
Social media exposure
Propaganda, falsehood, conspiracy theories, etc., related to the pandemic were increased, whereas social media was found to be one of the prime sources for collecting COVID-19-related information (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020). Therefore, constantly using social media was a significant risk factor for mental health sufferings, as some studies found (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020; Hossain et al., Reference Hossain, Ahammed, Chanda, Jahan, Ela and Islam2020c). For instance, 56.0% anxiety was found, with these participants reporting more than 4 h of social media exposure, whereas it was 42.1% for ⩽2 h (Hossain et al., Reference Hossain, Ahammed, Chanda, Jahan, Ela and Islam2020c). Similarly, a higher depression prevalence rate was observed in those physicians who reported it too hard to stay away from social media (58.3% v. 47.8%) (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020).
Physical exercise
The physical exercise patterns had been changed after the inception of the COVID-19 pandemic, which was reported significantly associated with psychological burdens. For instance, participants who were not involved or inadequately involved with physical exercise generally experienced higher levels of depression and anxiety (Islam et al., Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b; Khan et al., Reference Khan, Sultana, Hossain, Hasan, Ahmed and Sikder2020; Tasnim et al., Reference Tasnim, Sujan, Islam, Ritu, Siddique, Toma, Nowshin, Hasan, Hossain and Nahar2020).
Physical health conditions
Comorbidities were found to be a significant risk factor during the COVID-19 pandemic, leading to higher mental health problems. In contrast, the presence of several chronic diseases (i.e. hypertension, asthma, diabetes, heart diseases, chronic kidney disease, thyroid disorder) also significantly influenced mental health issues (Barua et al., Reference Barua, Zaman, Omi and Faruque2020; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020; Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020; Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021). Besides, due to more physical health problems, more severe psychological disorders were observed; for instance, it was reported among general people (Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020).
Psychological problems
A few studies reported other psychological problems associated with depression, anxiety, and stress. For instance, insomnia has been reported to have influenced the risk of mental health sufferings among university students and general people (Islam et al., Reference Islam, Sujan, Tasnim, Sikder, Potenza and van Os2020b; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020). However, the physicians who reported sleeping <6 h are significantly associated with higher depression and anxiety symptoms (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020).
COVID-19-related risk factors
Insufficient protective resources
The shortage of protective tools was a risk factor for psychological distresses during the COVID-19 pandemic. However, few studies reported that the lack of personal protection equipment, inadequate or insufficient training, and other incentives related to protection influenced the risk of mental health problems among healthcare professionals (Barua et al., Reference Barua, Zaman, Omi and Faruque2020; Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020; Tasnim et al., Reference Tasnim, Sujan, Islam, Ritu, Siddique, Toma, Nowshin, Hasan, Hossain and Nahar2020). Besides, Sakib et al. (Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021) found that only 15.9% of the healthcare professionals were satisfied with the quality of the PPE provided by the authorities, and the prevalence of depression was higher among HCPs who were dissatisfied with PPE (30.2% v. 18.0%). However, no studies that reported PPE-related issues in respect to mental health were conducted in other cohorts.
COVID-19-related perceptions
Peoples' perception of the COVID-19 pandemic significantly impacted their mental health. A study found that participants who had the lowest confidence in their current living place due to the COVID-19 pandemic and were highly concerned about their earning showed enormously significant associations with higher mental health sufferings (Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020). Whereas, in the case of perception of the current social life, satisfied respondents were less likely to have depression, anxiety, and stress (Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020). In addition, perceptions related to (i) normal life disruption caused by the COVID-19 pandemic, (ii) its negative mental health effect of the pandemic, (iii) its effects on the healthcare system, leading people not be able to get enough medical care, (iv) for Bangladesh, the COVID-19 pandemic does/will not be a major problem, (v) its negative impact on education, etc., had been observed being associated with mental health problems (Islam et al., Reference Islam, Bodrud-Doza, Khan, Haque and Mamun2020c; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020).
Fear of COVID-19 infection
Most of the studies reported fear of COVID-19 infection influencing the risk of mental health problems, whereas fear of getting infected by the SARS-CoV-2 either by themselves or their family members or relatives were the risk factors (Al Zubayer et al., Reference Al Zubayer, Rahman, Islam, Babu, Rahman, Bhuiyan, Khan, Chowdhury, Hossain and Habib2020; Khan et al., Reference Khan, Sultana, Hossain, Hasan, Ahmed and Sikder2020; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020; Yeasmin et al., Reference Yeasmin, Banik, Hossain, Hossain, Mahumud, Salma and Hossain2020; Faisal et al., Reference Faisal, Jobe, Ahmed and Sharker2021; Safa et al., Reference Safa, Anjum, Hossain, Trisa, Alam, Abdur Rafi, Podder, Koly, Azad, Ahmad, Nodi, Ashraf, Quamrul Akhter, Ahmed and Hasan2021; Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021). For instance, bankers reported that they were fearful of getting infected by the SARS-CoV-2 as their colleagues became infected, which later developed mental health problems (more specifically depression) among the other bankers (Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021).
COVID-19-related symptoms
People feeling or suffering from the COVID-19-related symptoms were at an increased risk of mental health-related outcomes (Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020; Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020). A study among the students found having more than one symptom had higher odds of stress and anxiety levels compared to those with one symptom (3.06 v. 1.60, and 4.96 v. 3.02, respectively; reference: no symptom) (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020). Correspondingly, another study observed that participants who had COVID-19-like symptoms, including fever, fatigue, and dry cough in the last 14 days, were significantly prone to suffering from depression, anxiety, and stress (Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020).
Being suspected/infected with the COVID-19
Individuals who suspected or confirmed that they had close or indirect contact with the confirmed cases of COVID-19 were significantly suffered from higher levels of anxiety, depression, and stress (Rahman et al., Reference Rahman, Khan, Sakib, Chakma, Procheta, Mamun, Arony, Rahman and Rahman2020). Similarly, 3.17 and 3.99 times higher risk of anxiety and stress suffering were observed in these participants reporting contact with individuals with confirmed cases of COVID-19 (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020).
Being quarantined or isolated
Quarantine and isolation are the situations that generally increase the higher risk of mental health problems through developing trauma among the quarantined or isolated individuals. For example, a study found that participants reported being quarantined 3.67-fold anxious than those who were not quarantined (Sayeed et al., Reference Sayeed, Kundu, Banna, Hasan, Begum and Khan2020). Another study by Ripon et al. (Reference Ripon, El-Sabban, Sikder, Hossain, Mim, Ahmed and Mehta2020) reported that females generally developed a 4.7 and 4.8 times higher risk of PTSD and depression among home-quarantined people than male-quarantined people.
Healthcare facility and patient-related information
Physicians reporting inadequate resources to deal with the COVID-19-infected patients were at an increased risk of depression and/or anxiety; that is, 2.28, 5.30, and 2.99 times higher risk was predicted for the mild, moderate, and severe levels of depression and/or anxiety, respectively (Barua et al., Reference Barua, Zaman, Omi and Faruque2020). Thus, healthcare professionals were being reported restlessness while examining the patients with flu-like symptoms, whereas a double depression rate was identified to these physicians compared to those who were not restless (Sakib et al., Reference Sakib, Akter, Zohra, Bhuiyan, Mamun and Griffiths2021). Consequently, physicians who reported to be ready to deal with a COVID-19-positive patient had experienced higher levels of depression and anxiety (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020).
Publication bias
Publication bias was visualized using Funnel plots (Fig. 5), where Egger's test was assessed for detecting publication bias. No significant publication bias was found in terms of depression (p = 0.14), anxiety (p = 0.08), and stress (p = 0.10).
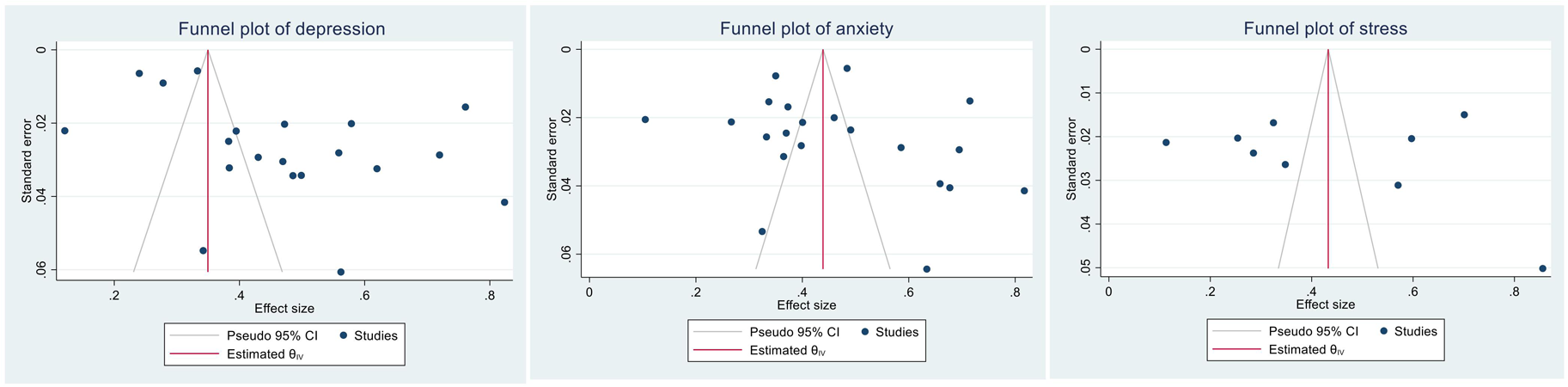
Fig. 5. Funnel plots for depression, anxiety, and stress.
Discussion
This study, the first systematic review and meta-analysis on common mental health problems during the COVID-19 pandemic in Bangladesh has potential implications for mental health policymaking and practice. It is anticipated that the findings presented herein can be implemented for (i) developing cost-effective mental health strategies, (ii) prioritizing and integrating mental health in existing healthcare systems, (iii) improving access to information and mental health resources, (iv) addressing mental health disparities across different cohorts, (v) mobilizing social and community resources and organizations, (vi) strengthening mental health systems for the forthcoming public health emergencies, etc. (Hossain et al., Reference Hossain, Tasnim, Sultana, Faizah, Mazumder, Zou, McKyer, Ahmed and Ma2020b).
After investigating a total of 24 recruited studies related to the COVID-19 pandemic, the pooled prevalence of depression, anxiety, and stress was 47% (95% CI 39–55%, I 2 = 99.14%), 47% (95% CI 39–54%, I 2 = 99.78%), and 44% (95% CI 30–58%, I 2 = 99.36%), respectively. Higher rates of depression were reported among the university student's cohort, that is, 82.4%, and lower rates were reported for bankers (i.e. 12.1%). Similarly, higher rates of anxiety (81.8%) were observed among university students, whereas the rate was lower for bankers (10.6%). In addition, general people reported a higher level of stress (85.6%), whereas lower was reported among the bankers (11.1%). Most importantly, the prevalence rates of depression, anxiety, and stress vary within a specific group (general population, for example) due to the utilization of different scales along with discrete cutoff values. Besides this, the sampling method and non-representativeness of the included studies may also limit its reproducibility (al Mamun et al., Reference al Mamun, Hosen, Misti, Kaggwa and Mamun2021). In addition, there may be an effect of the participants' area's COVID-19 exposure rate, personal and familiar history of the COVID-19 infection, financial conditions, and so forth lockdown-related issues, which are not possibly identified from the included studies for concluding an overall assumption on mental health problems prevalence rates across the cohorts (al Mamun et al., Reference al Mamun, Hosen, Misti, Kaggwa and Mamun2021). However, despite these limitations of the included studies, this review, for the first time, estimated the mental health problems' prevalence rates, which are anticipated to be worthy of consideration for defining the pandemic as a cautious situation rather than factual findings.
The COVID-19 pandemic has dramatically interchanged the consistent activities of individuals to prevent and control the outbreak. Under this circumstance, existing healthcare facilities in the country transformed into increased demands beyond its existence as competent. During the normal period, effective and efficient health care services were allegedly absent in Bangladesh (Anwar et al., Reference Anwar, Nasrullah and Hosen2020; Al-Zaman, Reference Al-Zaman2020). Along with this, due to the shortage of adequate preventive equipment, frontline healthcare professionals frequently feel unsafe and get scared to be infected as they have to directly take care of the COVID-19-infected patients (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020). Besides, many frontline healthcare professionals lost their lives worldwide being infected with the SARS-CoV-2 in their workplaces (Bandyopadhyay et al., Reference Bandyopadhyay, Baticulon, Kadhum, Alser, Ojuka, Badereddin, Kamath, Parepalli, Brown and Iharchane2020). Later on, this situation also upsurges psychological weight, including suicidal occurrences among the healthcare providers (Jahan et al., Reference Jahan, Ullah, Griffiths and Mamun2021). Consistent with the scenario, the physicians who provided services in the Dhaka division were more susceptible to being anxious than other divisional physicians, which may be due to being identified in most cases and deaths in the Dhaka division.
Applying some of the mandatory restrictions, including social distancing at the earlier period of the pandemic inception, people started grabbing and worrying about their lives and personal safety, fear of getting infected, lost a beloved one, absence of appropriate treatment, etc., which influenced the risk of depression, anxiety, and stress (Hossain et al., Reference Hossain, Rahman, Trisha, Tasnim, Nuzhath, Hasan, Clark, Das, McKyer and Ahmed2020a, Reference Hossain, Tasnim, Sultana, Faizah, Mazumder, Zou, McKyer, Ahmed and Ma2020b). Thus, participants belonging to general people and students cohorts had to experience mental health problems. Besides this, daily wage-earners were at higher risk of adverse psychological effects as they were unable to provide for their families' needs due to the nationwide lockdown and the loss of their jobs (Sultana et al., Reference Sultana, Khan, Hossain, Islam, Hasan, Ahmed and Khan2020), where economic crisis and unemployment is reported as the main suicide stressors during the COVID-19 pandemic (Mamun, Reference Mamun2021). However, despite the wage-earners being a risky group, only one study was conducted within this cohort. Similarly, a study was conducted for other vulnerable cohorts, e.g. COVID-19-infected people, COVID-19-suspected people, and bankers. Through the RT-PCR test, the individuals diagnosed with the COVID-19 generally got scared about the mortality risk, which affects their adverse psychological consequences and leads to suicidal situations [please refer to Mamun (Reference Mamun2021) for details]. For similar reasons, the quarantined people were found experiencing detraction of psychological well-being (Ripon et al., Reference Ripon, El-Sabban, Sikder, Hossain, Mim, Ahmed and Mehta2020). In addition, bankers were also at higher risk of being affected psychologically as they had to deal with the clients during the pandemic since the banks were not completely shut down. Therefore, their colleague's news of being infected got scary, although lower prevalence rates of anxiety, depression, and stress were reported in this cohort. Nevertheless of the situation, only one study was directed upon this mentally susceptible group, which may result in vague pictures concluding bankers compared to other cohorts are not at risk of higher mental health problems as reported in the only study (Yasmin et al., Reference Yasmin, Alam, Ali, Banik and Salma2021).
This review also revealed the associated risk factors that influenced the incidence of psychological consequences during the COVID-19 pandemic situation in Bangladesh. Based on the present review, socio-demographic factors including gender (mostly being female), younger people, living in an urban area, family size (more than five members), being unemployed, marital and educational status, having children and elderly in a family influenced the risk of being mentally affected. Furthermore, it was observed that people who had existing physical health-related comorbidities developed higher psychological problems (Barua et al., Reference Barua, Zaman, Omi and Faruque2020; Mamun et al., Reference Mamun, Sakib, Gozal, Bhuiyan, Hossain, Bodrud-Doza, Al Mamun, Hosen, Safiq and Abdullah2020). Besides this, being physically inactive and constantly using social media and watching news reported an increase in the risk of mental instabilities (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020; Hossain et al., Reference Hossain, Ahammed, Chanda, Jahan, Ela and Islam2020c). In addition, the COVID-19-related perceptions, experiencing the COVID-19-related symptoms, being suspected or infected with the SARS-CoV-2, being contacted with the COVID-19 confirmed cases, being quarantined or isolated, etc., were reported as the psychological suffering risk factors. Finally, the fear of being infected with the virus due to the scarcity of appropriate preventive equipment and inadequate resources in healthcare settings to deal with the COVID-19 infected patients were also reported as a risk factor of those psychological consequences (Hasan et al., Reference Hasan, Hossain, Safa, Anjum, Khan, Koly, Alam, Rafi, Podder and Trisa2020). In the end, it can be said that any of the COVID-19-related adverse outcomes increased the risk of higher mental health problems.
Several limitations of this review are yet to be mentioned. First of all, potential studies that could have met this review inclusion criterion were not included beyond the strategies, which may limit the review by selection bias; although databases such as Google Scholar and ResearchGate were used for screening additional articles, and the research team tried their best to sort out all of the eligible articles. Preprint articles were included in this review in view of disseminating the available relevant information; however, these articles being non-peer-reviewed can be one of the limitations of study inclusion. In addition, the study had significant heterogeneity in terms of reporting a pooled prevalence of depression, anxiety, and stress. Using different assessment scales and cutoff values simply explained the heterogeneity found in the review. Additionally, the risk factors associated with mental health problems were estimated from different analyses in the included studies. Despite these limitations, the present review provides an overall estimation of the mental health problems (e.g. depression, anxiety, stress) during the COVID-19 in the context of Bangladesh, which may have potential influences on adopting preventive mental health strategies, including knowledge exchange and training people through employing online-based intervention programs along with providing psychological cares, implementing cohort-based intervention program, arranging series webinar with a special focus on mental health, telecasting positivity about COVID-19 on media channel by taking as caution rather than factual findings.
Concluding remarks
The COVID-19 pandemic has become a global public health threat due to its devastating effects on peoples' lives worldwide. As an infectious life-threatening pneumonic disease, the pandemic impacted individuals' psychological well-being and physiological departures. This pandemic situation adversely altered the normal life patterns of all sections of people due to its adverse effect and implemented some restrictive measures associated with developing psychological problems such as depression, anxiety, and stress. To facilitate mental health policymaking and practice, there is no beyond integrated information. Therefore, for the first time, the present study depicts the prevalence rates for these mental health outcomes along with its influencing factors, which demand the potential attention of the government of Bangladesh to alleviate these outcomes by implementing some appropriate measures based on specific cohorts; for instance, raising awareness by providing proper knowledge and effective psychological care by a psychologist or psychiatric nurse by organizing online-based intervention programs. In addition, the authorities should also telecast positive information on media (such as recovery rate) related to COVID-19 to reduce psychological burdens.
The mental health prevention approach for psychiatric professionals should consist of two major aspects: prevention of mental health issues and mental well-being promotion. The burden of mental health problems can be prevented through three levels (i.e. primary, secondary, or tertiary). Identified risk factors of depression, anxiety, and stress exacerbated by the COVID-19 pandemic situation include socio-economic inequalities, unemployment, poverty, debt, food insecurity, child adversity, parental mental disorder, physical conditions, isolation, and quarantine issues should care at the primary level. Later on, early intervention to reduce the adverse effects and rehabilitation of the suffering people should be considered by education, reducing stigma, etc. Mental health promotional programs (e.g. tele-mental health services, online campaigns, etc.) are suggested considering by psychiatric professionals. However, from this review, the provided baseline information related to prevalence and risk factors of depression, anxiety, and stress across different cohorts can be utilized in the policy levels to adopt appropriate preventive measures and practices to alleviate psychological consequences.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2021.49
Data
All relevant data are within the manuscript cited in the respective places.
Acknowledgements
The authors would like to acknowledge that their affiliation, CHINTA Research Bangladesh, was formerly known as Undergraduate Research Organization.
Financial support
None.
Conflict of interest
None.
Ethical standards
Not applicable.










