“Everyone who made fun of me
Thought that I could not live anymore
All mockers are ashamed today, aha!
Today I am strong
Today I am happy
When I was raped
My relatives and neighbors abandoned me
Today I accept myself
All my enemies are ashamed”
(Cohorte Femmes Heroines, 2018 A4A Records Inc.)
Introduction
The Democratic Republic of the Congo (DRC) has continued to suffer from conflict and instability since the civil wars in 1996–1997, and 1998–2003 that killed over 5.4 million people (Warren, Reference Warren2011). Rape has been one of the most brutal weapons used during these conflicts and subsequently by rebel militias to destabilize communities (Mukwege and Nangini, Reference Mukwege and Nangini2009; Meger, Reference Meger2010; Banwell, Reference Banwell2014). Estimates suggest 40% of women in the region have experienced sexual violence (Johnson et al., Reference Johnson, Scott, Rughita, Kisielewski, Asher, Ong and Lawry2010). Sexual violence occurs within a broader context of insecurity including armed robbery of households, pillaging and looting of villages, kidnappings, and murder (Human Rights Watch, 2002; Bartels et al., Reference Bartels, Scott, Leaning, Mukwege, Lipton and VanRooyen2010). Given the adverse impact of sexual violence and conflict-associated trauma on mental health (Campbell et al., Reference Campbell, Dworkin and Cabral2009; Chen et al., Reference Chen, Murad, Paras, Colbenson, Sattler, Goranson, Elamin, Seime, Shinozaki, Prokop and Zirakzadeh2010; Dossa et al., Reference Dossa, Zunzunegui, Hatem and Fraser2014; Ba and Bhopal, Reference Ba and Bhopal2017), provision of evidence-based interventions effective in the context of humanitarian crises and low-income post-conflict settings is critical (Bass et al., Reference Bass, Annan, Murray, Kaysen, Griffiths, Cetinoglu, Wachter, Murray and Bolton2013; Murray et al., Reference Murray, Augustinavicius, Kaysen, Rao, Murray, Wachter, Annan, Falb, Bolton and Bass2018; Purgato et al., Reference Purgato, Gastaldon, Papola, van Ommeren, Barbui and Tol2018; Bangpan et al., Reference Bangpan, Felix and Dickson2019).
Research on psychological services in the context of humanitarian crises remains limited, but recent meta-analyses (Morina et al., Reference Morina, Malek, Nickerson and Bryant2017; Purgato et al., Reference Purgato, Gastaldon, Papola, van Ommeren, Barbui and Tol2018; Bangpan et al., Reference Bangpan, Felix and Dickson2019) support the value of such services. One meta-analysis of 18 randomized controlled trials providing psychotherapy to survivors of mass violence concluded that psychotherapy reduced post-traumatic stress disorder (PTSD) and depression (Morina et al., Reference Morina, Malek, Nickerson and Bryant2017). A second meta-analysis assessed 35 controlled trials among adults affected by humanitarian crises in low- and middle-income countries. Nine assessed cognitive behavioral therapy (CBT) (Bangpan et al., Reference Bangpan, Felix and Dickson2019). In those studies, CBT reduced PTSD, depression, and anxiety. A third meta-analysis of 36 studies found that psychological therapy had large to moderate effects, but impact of the interventions declined over time (Purgato et al., Reference Purgato, Gastaldon, Papola, van Ommeren, Barbui and Tol2018). In the eastern DRC, a randomized control trial among survivors of sexual violence (Bass et al., Reference Bass, Annan, Murray, Kaysen, Griffiths, Cetinoglu, Wachter, Murray and Bolton2013), reported that group cognitive processing therapy (CPT) was more effective than individual support sessions in reducing anxiety and depression with improvements sustained in the CPT group at 6 months post-intervention.
The Panzi Hospital in Bukavu, South Kivu, having treated more than 30,000 survivors of sexual violence, developed a four-pillar holistic model of care (Panzi Foundation, 2020) that integrates medical therapy and psychosocial support, economic re-integration, and legal assistance. In 2015, Make Music Matter partnered with Panzi to incorporate an innovative music therapy program, Healing in Harmony (HiH), into their holistic healing model (Make Music Matter, 2020). Music therapy, that pairs therapy with lyrical music training has been shown to be effective at reducing anxiety, depression, and PTSD (Erkkilä et al., Reference Erkkilä, Punkanen, Fachner, Ala-Ruona, Pöntiö, Tervaniemi, Vanhala and Gold2011; Carr et al., Reference Carr, d'Ardenne, Sloboda, Scott, Wang and Priebe2012; Carr et al., Reference Carr, Odell-Miller and Priebe2013; Aalbers et al., Reference Aalbers, Fusar-Poli, Freeman, Spreen, Ket, Vink, Maratos, Crawford, Chen and Gold2017; Landis-Shack et al., Reference Landis-Shack, Heinz and Bonn-Miller2017). Music stimulates areas of the brain involved in traumatic memory and sensory-emotional processing (Koelsch, Reference Koelsch2009). As music and trauma are both sensory mediated, music can also provide an alternate means of accessing severe past trauma and facilitate processing of these experiences and expression of related emotions (Johnson, Reference Johnson1987; Bensimon et al., Reference Bensimon, Amir and Wolf2012; Carr et al., Reference Carr, d'Ardenne, Sloboda, Scott, Wang and Priebe2012). As the photographic nature of traumatic memories can be difficult to express in linguistic forms (Johnson, Reference Johnson1987; Bensimon et al., Reference Bensimon, Amir and Wolf2012), symbols and metaphors, such as those present in music and lyric writing, can help in verbalization and processing of trauma. In their critical synthesis, McFerran et al. organize musical therapy approaches into four categories of stabilizing, entrainment, expressive, and performative purposes (McFerran et al., Reference McFerran, Lai, Chang, Acquaro, Chin, Stokes and Crooke2020). The performative category includes recognition of the tolerant societal context in which traumas such as war and abuse occur, aiming to enable identities to be reconstructed and ‘brought to life’ through songs and public musical performances which also support advocacy. Recognizing that the physical and psychosocial needs of sexual violence survivors are linked, HiH is centered around a locally built professional recording studio situated on the campus of a health facility.
HiH provides music therapy to survivors of sexual violence and violence-related trauma. Working with a trained therapist and professional music producer, participants begin the healing process by writing, recording, and professionally producing songs about their emotions and experiences, simultaneously engaging in therapy and developing their own musical artistry. The therapeutic approach, based on CBT (Rothbaum et al., Reference Rothbaum, Meadows, Resick, Foy, Foa, Kean and Friedman2000), aims through group-therapy and lyrical music to help participants verbalize their trauma and initiate the assessment and cognitive stages of the healing process. As they talk through their experiences, the developing artists are encouraged to write down their stories. When a narrative emerges, the producer begins composing an instrumental accompaniment that eventually creates a song performed individually or in groups. The emotional state of each participant is closely monitored, and individual counseling is provided when required. The environment created is one of joy and healing, focusing on turning negative thinking patterns into positive and more adaptive ones through cognitive restructuring. The goal is for participants to emerge as confident artists and advocates, publicly disseminating their music through local radio and television broadcasts, social media, community concerts, and CD distribution.
Prior research has demonstrated the effectiveness of psychological interventions in humanitarian contexts to reduce anxiety, depression, and PTSD (Purgato et al., Reference Purgato, Gastaldon, Papola, van Ommeren, Barbui and Tol2018; Bangpan et al., Reference Bangpan, Felix and Dickson2019). Yet, few studies have been conducted in the DRC or in the context of ongoing violence and insecurity (Bass et al., Reference Bass, Annan, Murray, Kaysen, Griffiths, Cetinoglu, Wachter, Murray and Bolton2013). This study aimed to assess whether participation in HIH was associated with a decrease in symptoms of anxiety, depression, or PTSD or in improvement in women's self-perception; and, to evaluate whether demographic and trauma-related risk factors were associated with symptom improvement in the context of ongoing insecurity.
Methods
This study utilized a stepped-wedge design (Hemming et al., Reference Hemming, Haines, Chilton, Girling and Lilford2015) to assess an HiH program being rolled out to in an area of ongoing conflict, violence, and instability at a rural hospital affiliated with Panzi Hospital in Mulamba. Mulamba is a grouping of 45 villages situated in the Walungu territory of South Kivu province. Participants came from villages within a 5 min to 1-h walk from the Mulamba Hospital. A stepped-wedge design sequentially enrolls groups of participants at regular intervals (steps) such that in the first interval one group is exposed to the program while other groups remain unexposed. The second group is exposed to the program in the second interval, and so on, until all groups are exposed to the program. The unexposed period provides a self-control for a given group across time as well as a secular control for the exposed group in a given time-window. Throughout the study period, especially during the fall of 2017, villages in the area reported armed robbers attacking and threatening to attack households, pillaging, and looting at night, kidnappings, and murder.
The Healing in Harmony program
HiH program staff were trained and supervised by a psychologist (JC) and music producer with prior experience implementing the program at Panzi Hospital. Each cycle offered a 12 week program, with sessions held twice per week, followed by a period of community engagement. The therapeutic approach is more fully described in Supplementary Box S1.
Study population
Women aged 15–69 years referred for psychological services were screened in September 2017 (groups 1 and 2, n = 128) and January 2018 (group 3, n = 72), and by design began their HiH sessions in September 2017 (group 1), February 2018 (group 2), and July 2018 (group 3). As the HiH program had to transport women seeking services from their villages to the rural clinic and given program cost constraints, all women from each village were assigned to the same group. To allocate women screened in September into group 1 or 2, women were clustered by village, median mental health scores for each village were calculated, villages were sorted by their median mental health scores, and then villages were systematically allocated alternately into groups 1 and 2 (i.e. the village with the highest scores was allocated to group 1 and the village with the next highest scores to group 2, etc.). Women referred to the rural clinic after September were enrolled in group 3. Each group was organized into therapy sections of approximately 15 women (range: 9–18) with most sections meeting for 23–27 sessions, although three ran just 13–14 sessions. Thirty-two women who were screened but did not participate in HiH and one who participated partially in two different program offerings were excluded, thus 167 (83.5%) were eligible for analysis. Participants and non-participants did not differ by demographic characteristics or trauma-related risk factors (Supplemental Table S1). Among eligible participants, 106 in groups 1 and 2 (91.4%) participated in all planned assessments, while in group 3, 45 (88.2%) participated in all planned assessments.
The stepped-wedge design and measurement timing is illustrated in Fig. 1. Each group was administered a mental health screening shortly before (pre-test/time 0) and immediately after completing (post-test/time + 1) their HiH Program. Groups 2 and 3 participated in an additional pretest (time − 1) three months prior to beginning their HiH program, serving as an unexposed self-control from time − 1 to time 0. Groups 1 and 2 participated in an interview 3 months post treatment (time + 2). Group 1 also completed an interview 6 months post-treatment (time + 3). The study was approved by the Institutional Ethics Commission of the Catholic University in Bukavu (UCB/CIE/NC/003C/2017). All women provided informed consent. Interviews were conducted in Mashi and Swahili by trained interviewers who were psychologists. As interviews included sensitive questions related to women's experiences of trauma, the HiH clinical psychologists were present to counsel women if needed during the data collection interviews. In addition to assessing mental health, interviews obtained information on demographic characteristics, risk factors, and perceptions of life and self.

Fig. 1. Illustration of the stepped-wedge design. The HiH program was implemented sequentially across three time periods (orange): September to December 2017, February to April 2018, and June to August 2018, with data collection occurring in September 2017, December and January 2018, May 2018, and September 2018. Groups 2 and 3 contributed time as unexposed (red) and all groups contributed post-exposure time (green). −1 corresponds to the measure 3 months prior to treatment, 0 to the measure at start of treatment and +1, +2, +3 to the measures at immediately post-treatment and at the 3 and 6 month follow-ups, respectively.
Mental Health Screening Questionnaires
Mental Health Screening Questionnaires included the Hopkins Symptom Checklist (Hemming et al., Reference Hemming, Haines, Chilton, Girling and Lilford2015) to assess anxiety and depression and The Harvard Trauma Questionnaire to assess post-traumatic stress syndrome (PTSD) (Mollica et al., Reference Mollica, Caspiyavin, Bollini, Truong, Tor and Lavelle1992; Mollica et al., Reference Mollica, McDonald, Massagli and Silove2004). Average depression, anxiety, and PTSD scores were calculated as total score divided by the number of questions answered, with average scores ranging from 1 to 4 (higher values indicating greater levels of depression/anxiety/PTSD). Women were classified as screening positive for each outcome if they scored greater than or equal to 1.75 (Mollica et al., Reference Mollica, McDonald, Massagli and Silove2004).
Perceptions of life and self
We asked women whether they felt happy, sad, proud of their life, had hope for the future, and whether they liked themselves as they were. Response categories (yes, not very, no) were re-grouped for analysis (yes, not very/no).
Demographic characteristics and risk factors
Demographic characteristics included age, although it should be noted women often do not know their age, schooling (none, some primary, primary or above), marital status (married/co-habiting, single, divorced/separated or widowed), whether or not she had children (yes/no). Occupation was assessed by asking whether she worked in her own field (yes/no), another's field (yes/no), or had a job or small business (yes/no). Women were asked whether they had ever experienced a traumatic event and time since the most recent event; whether she was a survivor of sexual violence; whether she was a refugee, an internally displaced person or had had to abandon her home due to violence or lack of security; and, whether she had been abandoned by her husband, her family, or her community.
Statistical analysis
Means and standard deviations were calculated for continuous variables and frequencies for categorical variables at the initial screening by participation status (yes/no). We calculated significance of differences using chi-squared tests and Fisher's exact tests. Given the ongoing insecurity in the region, we calculated the proportion of individuals who reported a trauma within the past 3 months at the pre-test, post-test, and 3-month follow-up interviews and ascertained the number of women who first reported being a survivor of sexual violence at the post test or follow-up interviews.
To assess change over time, a time variable was defined in relation to start of the therapy (−1 = 3 months prior to therapy, 0 = start of therapy, +1 = end of therapy, +2 = 3 months post therapy, and +3 = six months post therapy). We also summarized the HiH program effects by collapsing time into pre-treatment (time − 1 and 0) or post-treatment (time + 1, +2, or +3) periods. Descriptive statistics were calculated and box plots were plotted for depression, anxiety, and PTSD scores at each time point. We calculated the percentage and 95% confidence intervals (CIs) for scoring positive for depression, anxiety, and PTSD at each time point.
We used generalized estimating equation (GEE) models with unstructured covariance and a normal distribution to estimate mean differences and 95% CIs in continuous scores. We modeled proportions using GEE models with an unstructured covariance and Poisson distribution (Zou and Donner, Reference Zou and Donner2013) to estimate relative risks (RRs) and 95% CIs. All models were adjusted for age (scaled by 10 years) and the design variable “Group”. First, we ran models evaluating each outcome by time with time 0, the immediate pre-test, as the reference point. Next, we re-ran models using the pre v. post treatment variable adjusting for demographic characteristics and time-varying risk factors. Statistical significance was defined at α < 0.05. Analyses were performed using RStudio version 1.1.456 (RStudio Team) and SAS version 9.4 (SAS Institute).
Results
The 167 women ranged in age from 15 to 69 years of age with a median age of 37 years. Table 1 provides information on the distribution of participant characteristics, overall and by group. Two-thirds were of reproductive age (15–44 years) and one-third were 45 years and older. A total of 38.3% had no schooling, 34.1% had some primary schooling, and 27.5% had completed primary school or more. Almost all women (94.6%) had ever been married, with approximately two-thirds currently married/cohabiting, and 95.2% reported having children. Over 70% worked in their own fields and in others' fields, while 37.7% reported having a job or small business. Groups differed slightly in age (p = 0.017) but not by other demographic characteristics.
Table 1. Demographic characteristics and vulnerability factors of women enrolled in the HiH program in South Kivu, DRC

a Chi-square test.
b Fisher's exact test.
At their initial interview, three-quarters of the women reported having ever experienced a traumatic event, 41.3% reported being the survivor of sexual violence, and one-third reported being a refugee, displaced, or having had to abandon their home. The proportion who reported a trauma within the past 3 months at the pre-test, post-test, and 3-month follow-up interview was 9.7% (n = 16), 14.6% (n = 23), and 25.2% (n = 28), respectively. At the post-test interviews, an additional 26 women reported being survivors of sexual violence. One-quarter of the women reported having been abandoned by their husband, approximately one-fifth by their family, and slightly more than one-tenth by their community. Women enrolled in group 3 were least likely to report having experienced a traumatic event (p < 0.001), to report being a sexual survivor (p = 0.006), or to have been displaced (p = 0.036). Most women (86.8%) attended half or more of their therapy sessions.
Depression, anxiety, and PTSD
Figure 2 presents boxplots of the average scores for anxiety, depression, and PTSD by time and Fig. 3 presents similar boxplots by group. Three months prior to participating in the program (time − 1), median scores for depression were 2.00 (interquartile range [IQR] = 1.67–2.47), anxiety 2.25 (IQR = 1.90–2.90), and PTSD 1.81 (IQR = 1.31–2.50), slightly lower than at the pre-test (time 0) assessment. At the pre-test (time 0), median scores for depression were 2.20 (IQR = 1.73–2.67) declining to 1.40 (IQR = 1.07–2.07) at the post-test assessment while scores for anxiety were 2.70 (IQR = 2.00–3.00) declining to 1.75 (IQR = 1.10–2.40) and for PTSD were 2.06 (IQR = 1.56–2.69) declining to 1.31 (IQR = 1.06–2.00) (see also Supplemental Table S2). After the HiH program, median scores remained stable at 3 (time + 2) and 6-months (time + 3).
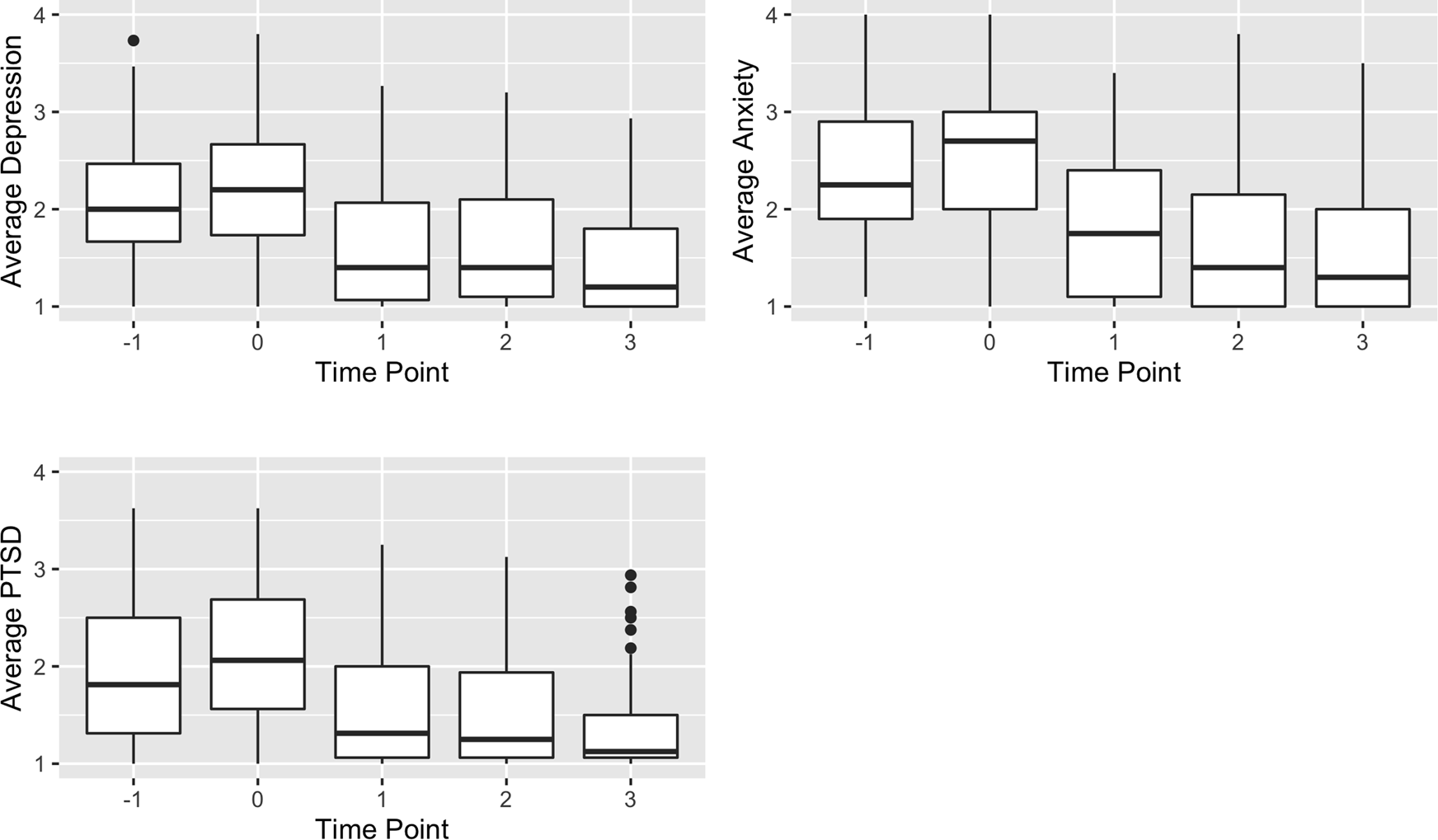
Fig. 2. Boxplots of anxiety, depression, and PTSD average scores by time, HiH program South Kivu, DRC by time.

Fig. 3. Boxplots of average scores for anxiety, depression, and PTSD by time and group, HiH program in South Kivu, DRC (n = 167).
The proportion of women screening positive for depression, anxiety, and PTSD across time is presented in Table 2. At the pre-test (time 0), three-quarters of women screened positive for depression, over four-fifths for anxiety, and two-thirds for PTSD. Seventy-five percent screened positive for two conditions and two-thirds screened positive for all three conditions. At the post-test (time + 1), only one-third screened positive for depression, half screened positive for anxiety, and one-third screened positive for PTSD with 40% and 28% scoring positive for two and three conditions, respectively. The decline in the proportion screening positive post-therapy remained stable at follow-up. Median scores at the initial screening assessment were similar for groups 1 and 2, but more than a half a point lower in group 3 (Supplementary Table S3).
Table 2. Proportion (and 95% CIs) scoring positive for depression, anxiety, and PTSD among women enrolled in the HiH program in South Kivu, DRC by time (N = 167)

a As time + 3 includes only group 1 it is not presented here (see Fig. 2).
Table 3 presents the multivariable regression results adjusting for age and group. Schooling, marital status, and occupation were not associated with mental health scores (data not shown). Depression and PTSD scores declined significantly, by slightly more than half a point on average, from the pre-test (time 0) to the post-test (time + 1). The probability of screening positive for depression and PTSD at the post-test also declined by about half (RR = 0.49, 95% CI 0.40–0.61 and RR = 0.54, 95% CI 0.44–0.67, respectively) compared to the probability at the pre-test (time 0). Similarly, anxiety scores declined by two-thirds of a point and the probability of screening positive for anxiety declined by 40% (RR = 0.61, 95% CI 0.52–0.72). No significant differences were observed for depression or anxiety in scores 3-months before to the score at the start of the HiH program (time − 1 to time 0); however, PTSD scores were slightly but significantly lower at time − 1 than at time 0. Improvements in scores were sustained at the 3-month (time + 2) follow-up assessment. Results were similar when we categorized time by pre/post-program participation, with the average post treatment decline in scores being −0.57 (95% CI −0.66 to −0.47), −0.73 (95% CI−0.85 to −0.62), and −0.52 (95% CI −0.62 to −0.42) for depression, anxiety, and PTSD, respectively. The probability of screening positive declined by approximately half.
Table 3. Regression models for depression, anxiety, and PTSD by time adjusted for group and age, among women enrolled in the HiH program in South Kivu, DRC (N = 167)
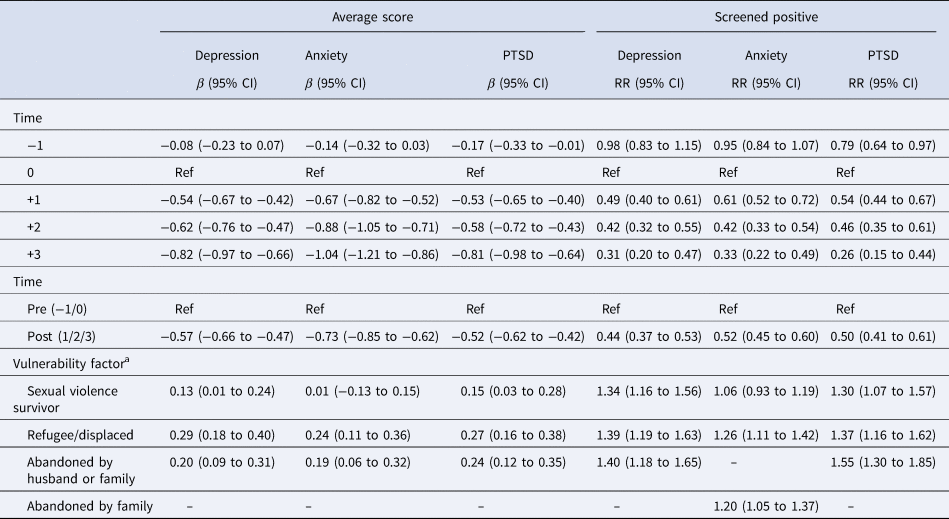
a Models adjusted for time (pre v. post-treatment), group, and age.
Trauma-related risk factors were associated with higher average scores for depression, anxiety, and PTSD (Table 3). Women who reported being survivors of sexual violence had a 30% increased risk of screening positive for depression and PTSD and their average scores for these two conditions averaged about a tenth of a point higher than women who were not survivors. Women who were refugees or had been displaced from their homes had a 25–39% higher probability of screening positive for a mental health condition and their average scores averaged about a quarter of a point higher than other women. Women who had been abandoned by their husbands or family had a 40% and 55% higher probability of scoring positive for depression and PTSD, respectively, while women abandoned by their family had a 20% higher probability of scoring positive for anxiety. There were no interactions between pre v. post treatment and these risk factors.
Perceptions of self and life
Table 4 provides information on women's perception of self and life over time. At the pretest, about 40% of women reported feeling happy and 35% reported feeling sad, yet notably three-quarters reported feeling hopeful. Less than one-third were proud of themselves while just 40% liked themselves as they were. Following the program, a substantially greater proportion of women reported being happy (62.4%), having a sense of pride (59.2%), being hopeful (83.4%), and liking themselves (66.2%), and a lower proportion reported being sad (17.7%). Group 3 differed from groups 1 and 2 in the proportion of women who reported feeling sad and proud of themselves (Supplementary Table S4). In the multivariable models adjusting for age and group (Table 5), the probability of reporting feeling happy increased by 50% and feeling sad was halved at the time of the post-test (time + 1) compared to the pre-test (time 0). The probability of feeling proud of oneself nearly doubled and there was a 65% increase in the proportion reporting that they liked themselves as they were. Similar to results for the mental health screening tests, improvements in perceptions of self and life were sustained through the follow-up assessments and results were similar when we analyzed time by pre/post-program participation. For both feeling happy and being proud of oneself, an interaction was present between time and being a survivor of sexual violence. Prior to participation in the program, survivors were half as likely to report feeling happy (RR = 0.52, 95% CI 0.37–0.73) or proud of themselves (RR = 0.55, 95% CI 0.38–0.81) compared to women who had not experienced sexual violence. However, participation in the program more than doubled the probability of happiness in survivors (RR = 2.31, 95% CI 1.70–3.14) compared to a 32% increase in other women (RR = 1.32, 95% CI 1.07–1.62). The probability of reporting being proud of oneself also increased over 2.5 times for survivors post-treatment (RR = 2.64, 95% CI 1.90–3.67) compared to a 71% increase in other women (RR = 1.71, 95% CI 1.35–2.17).
Table 4. Proportion (95% CI) of women participating in the HiH program reporting they felt happy, sad, proud, hopeful and that they liked themselves by time, South Kivu, DRC by time (N = 167)

Table 5. Regression modelsa for perceptions of self by time adjusted for group and age, women enrolled in the HiH program in South Kivu, DRC (N = 167)

a Models adjusted for group and age.
Discussion
This paper assessed the impact of HiH, an innovative program that develops musical artistry while providing psychotherapy, on the mental health of women who had suffered from trauma and lived in areas of ongoing insecurity in the eastern DRC. At baseline, three-quarters screened positive for depression, four-fifths for anxiety, and two-thirds for PTSD. The HiH program reduced anxiety, depressive, and PTSD significantly with the probability of screening positive declining by 40, 50, and 50%, respectively. It also reduced self-perceived stigma, feelings of unworthiness, and unhappiness. At baseline, survivors of sexual violence were at increased risk of screening positive for depression and PTSD while displaced and abandoned women were at increased risk of all three conditions compared to women who were not survivors and not displaced/abandoned respectively. Improvement in mental health and self-perception occurred in the context of ongoing trauma and insecurity and was sustained up to 6 months following the program.
Research on the impact of psychological services in the context of humanitarian crises remains limited but recent meta-analyses (Morina et al., Reference Morina, Malek, Nickerson and Bryant2017; Purgato et al., Reference Purgato, Gastaldon, Papola, van Ommeren, Barbui and Tol2018; Bangpan et al., Reference Bangpan, Felix and Dickson2019) document that psychotherapy reduced PTSD, depression, and anxiety with large to moderate effects, although its impact declined over time (Purgato et al., Reference Purgato, Gastaldon, Papola, van Ommeren, Barbui and Tol2018). In nine studies of CBT, the standardized mean differences in anxiety, depression, anxiety, and PTSD scores were −0.69, −0.71, and −0.66, respectively (Bangpan et al., Reference Bangpan, Felix and Dickson2019), comparable to results of our study. In the randomized control trial among survivors of sexual violence in the DRC (Bass et al., Reference Bass, Annan, Murray, Kaysen, Griffiths, Cetinoglu, Wachter, Murray and Bolton2013), group CPT was more effective than individual support sessions in reducing anxiety and depression with improvements sustained in the CPT group at 6 months. The combined anxiety and depression score declined by 1.2 post-treatment in the CPT group and 0.5 in the individual support group, compared to 0.61 in the current study. We also demonstrated sustained improvements in mental health up to 6-months post treatment. However, approximately one-third of the women continued to screen positive for at least two of the three conditions. Further research is needed to address chronic mental health conditions.
Women reported traumatic events occurring concurrent with the program, thus ongoing violence and instability may have continued to cause distress, possibly dampening the impact of the HiH program. Nonetheless, PTSD, depression, and anxiety were reduced substantially following participation in the program and sustained up through the 6-month follow-up interview, supporting the value of offering HiH in the context of ongoing insecurity. The probability of reporting a sense of happiness, feeling proud in one's self, and of liking one-self increased substantially following participation in the HiH program.
This study measured risk factors associated with trauma, stigma, and social exclusion. The increased risk of family rejection associated with conflict-related trauma has been documented in other studies (Kohli et al., Reference Kohli, Perrin, Mpanano, Mullany, Murhala, Birnkurhorhwa, Mirindi, Banywesize, Bufole, Ntwali and Glass2014). Although women with these risk factors were more likely to screen positive for mental health conditions at baseline, we found little evidence of a differential impact of the program on mental health or ones sense of self or life. Although our power to assess interactions was limited, survivors of sexual violence reported greater improvements in their happiness and in feelings of self-pride than other women. We hypothesize that survivors may benefit from the creation of songs that restore dignity, instill pride, and reduce shame, potentially serving as a tool to transfer the shame of violation to perpetrators. This hypothesis could be investigated in future studies.
During the course of the program, staff inquired why women did not participate or missed sessions. Women reported that some men forbid women from attending, fearing discrimination. The community perceived that participation signified that a woman had been raped, contributing to women's stigmatization and affecting men's perceived dignity. Community information sessions were organized to clarify the program's purpose and to articulate its benefits. Some men subsequently expressed the desire to enroll in the HiH program to support women's healing, address the impact of violence on their own mental health, and provide an example to the community that the program was a health resource for everybody. Notably, during the initial screening period, interviewers had reported back that women were asking for their husbands to be included and in response to an open-ended question in the post-test interview some women stated that a session for men was needed. After completion of the research described here, a session was organized for men. Those who participated expressed their gratitude and proposed that sessions for men be continued to facilitate social integration and acceptance of psychological care.
This experience highlighted the importance of addressing the psychological care needs of communities as a whole and the potential harm in providing interventions only to subsets of a community at risk. Including only subgroups in the healing process within a traumatized community may reinforce stigmatization and weaken already fragile relationships within couples. In cultures that use collective approaches to solving individual and community problems, psychological interventions would optimally be designed from the outset with a community-based strategy. Others have stressed the importance of culturally sensitive mental health and psycho-social support services informed by gendered understanding and collective approaches that train local counselors, and use holistic strategies, e.g. combining music with the offer of counseling, plus social enterprises and justice programs (Liebling et al., Reference Liebling, Barrett and Artz2020). In the DRC, the number of skilled psychologists, social workers, and psychiatrists remains limited and should be increased, with professional training reinforcing eco-systemic theory and skills. By constructing a music studio within the health facility structure and embedding psychological care within the Panzi four pillar holistic structure, the HiH program reinforced the concept of multi-sectorial and interconnected interventions, appropriately contextualized for the eastern DRC. Additionally, the program is culturally well situated as music permeates African culture, influences the development of moral, religious, social, and political beliefs (Mbaegbu, Reference Mbaegbu2015), and has been used as a means of education and communication for generations (Levitin, Reference Levitin2008).
This study had limitations. Approximately 15% of screened women did not participate in the HiH program and about 10% of participants were lost to follow-up, thus selection bias is possible. However, analyses including all women did not differ substantially from results reported here (data not shown) and participants did not differ from non-participants in demographic characteristics or risk factors. Study participants were not randomly assigned to treatment groups. Although we were unable to randomly assign women to groups 1 and 2, they were systematically allocated by villages after stratification by mental health scores. Also, as we did not observe group 1 prior to starting the program we cannot rule out regression to the mean in this group. Group 3, which sought care after the program was initiated, had lower mental health scores at the time of enrollment than groups 1 and 2, suggesting that women recruited initially into the HIH program were the most affected women in this rural region. Nonetheless, the stepped wedge design accounted for secular change in mental health and women served as their own control. We did not have information on costs of the program. Future studies should consider including cost-effectiveness and cost-saving analyses.
Strengths of the study include the large sample size and multiple assessments per woman, with information on mental health status obtained prior to and up to 6 months after the program. We used standardized instruments and standardized their translation into Mashi. As the program was conducted in a context of ongoing insecurity, the study contributes to understanding of the value of providing psychosocial services in the context of ongoing conflict. Availability of information on trauma-related risk factors and psychological well-being addresses significant gaps in scientific knowledge.
In conclusion, participation in the HiH music therapy program had a positive impact on women's mental health, with improvements observed in the prevalence of PTSD, anxiety, and depression. Women's psychological-wellbeing and sense of self-worth also improved. The data suggest benefits of the program were substantially maintained up to 6 months following completion of the program. This impact persisted despite evidence that some women continued to experience conflict-related trauma during the study period. These data support the value of providing an integrated music and psychological care program in the context of ongoing humanitarian crises. Further research should test the HiH program in other humanitarian settings, in male and child conflict survivors, and in clinical comparative trials. Formal evaluation of the impact of the HiH program on reducing stigma and increasing social inclusion at the community level is needed. Creation of lyrical music helps women verbalize internalized pain but also diffuses through song a message with the potential to change women's self-image and community perceptions (McFerran et al., Reference McFerran, Lai, Chang, Acquaro, Chin, Stokes and Crooke2020). Further studies are needed to assess the effects of participants' lyrical expressions and community engagements at the societal level. Finally, in the context of humanitarian crises, conflict, and insecurity, more consideration should be given to ensuring availability of psychological support programs to all persons in need in the community, as targeting only women without including their partners, children, and other family members in the healing process may weaken cohesion of couples, families, and in the community.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2021.11.
Acknowledgements
We thank Helen Liebling and Josiah Kaplan for their comments on the draft manuscript. We also thank the Advisory Board for their service and counsel (Bhramar Mukerjee, Professor and Associate Chair, Department of Biostatistics, University of Michigan; Rachel Jewkes, Director, Gender and Health Research Unit, South African Medical Research Council; Helen Liebling, Senior Lecturer at Coventry University and clinical psychologist; Gunilla Berglund, Associate Professor, Department of Psychology, Stockholm University; Juvenal Bazilashe Mukungu Balegamire, Professor of Clinical Psychology, Evangelical University in Africa).
Financial support
Healing in Harmony was funded and supported by Elrha's Humanitarian Innovation Fund (HIF) program, a grant making facility which improves outcomes for people affected by humanitarian crises by identifying, nurturing, and sharing more effective, innovative, and scalable solutions. Elrha's HIF is funded by aid from the Netherlands Ministry of Foreign Affairs (MFA) and the UK Department for International Development (DFID). Elrha is a global charity that finds solutions to complex humanitarian problems through research and innovation. Visit www.elrha.org to find out more. SDH was supported as a Fulbright Scholar in the DRC during the period of field work.
Conflict of interest
JBB, AB, AM, MMH, PMS, BM, and SDH have no conflicts of interest. JC is currently employed by MakeMusicMatter to implement the HiH program globally (https://makemusicmatter.org/healing-in-harmony/).
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.











