Introduction
Indicated prevention implemented in specialized clinical high risk for psychosis (CHR-P) [Reference Fusar-Poli1] services [Reference Fusar-Poli, Estradé, Spencer, Gupta, Murguia-Asensio and Eranti2][Reference Kotlicka-Antczak, Podgórski, Oliver, Maric, Valmaggia and Fusar-Poli3][Reference Fusar-Poli, Spencer, De Micheli, Curzi, Nandha and McGuired4]has the potential to ameliorate presenting symptoms, delay or prevent the onset of psychosis, and reduce healthcare access and duration of untreated psychosis (secondary prevention) [Reference Oliver, Davies, Crossland, Lim, Gifford and McGuire5,Reference Fusar-Poli, McGorry and Kane6]. Individuals who meet CHR-P criteria are young help-seeking people (14–35 years old, mean age 21 years [Reference Fusar-Poli, de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt7]) presenting with several risk factors for psychotic disorders [8–10]. CHR-P criteria are assessed with validated semistructured psychometric instruments, which deliver a group-level estimate (i.e., at risk vs. not at risk) [Reference Fusar-Poli, Cappucciati, Rutigliano, Schultze-Lutter, Bonoldi and Borgwardt11] robustly associated with psychosis onset (meta-analytic odds ratio = 9.32) [Reference Radua, Ramella-Cravaro, Ioannidis, Reichenberg, Phiphopthatsanee and Amir8]. This association is tightly linked to the help-seeking behavior, because the same psychometric tools do not have prognostic value in general population [Reference Fusar-Poli12]. Other than psychotic onset, clinical trajectories for CHR-P include functional decline [Reference Fusar-Poli, Rocchetti, Sardella, Avila, Brandizzi and Caverzasi13], persistence of attenuated psychotic symptoms [Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rössler and Schultze-Lutter14], or other psychiatric comorbidities [Reference Oliver, Reilly, Boy, Petros, Davies and Borgwardt9].
CHR-P individuals are challenging to detect and follow up. Detection of most individuals at-risk for psychosis is one of the main barriers toward the implementation of the CHR-P paradigm in real-word clinical scenarios [Reference de Pablo, Radua, Pereira, Bonoldi, Arienti and Besana15].
Furthermore, meta-analytic evidence shows that only about 20% of CHR-P individuals develop a psychotic disorder after 2 years from ascertainment [Reference de Pablo, Radua, Pereira, Bonoldi, Arienti and Besana15]. It is therefore pivotal for CHR-P studies to use large samples and adequate follow-up in order to reach adequate statistical power. Considering the poor real-world outcomes associated with psychotic onset [Reference Fusar-Poli, De Micheli, Signorini, Baldwin, de Pablo and McGuire16,Reference Koutsouleris, Kambeitz-Ilankovic, Ruhrmann, Rosen, Ruef and Dwyer17], this is an upmost clinical and research priority. The consequences of inadequate statistical power in CHR-P studies can be directly observed on findings from interventional studies. For instance, while indicated prevention implemented in CHR-P services (e.g., cognitive behavioral therapy [CBT] as for [18]) has the potential to improve outcomes, the largest randomized controlled trials and the most recent network/Cochrane meta-analyses [Reference Davies, Cipriani, Ioannidis, Radua, Stahl and Provenzani19,Reference Bosnjak Kuharic, Kekin, Hew, Rojnic Kuzman and Puljak20] on CBT for psychosis prevention held negative results. A recent umbrella review (a review of meta-analyses) indicated that these trials were likely underpowered, because several hundreds of CHR-P individuals would be required to reach critical mass in interventional preventive studies [Reference Fusar-Poli, Davies, Solmi, Brondino, De Micheli and Kotlicka-Antczak21].
Implementing large-scale collaborations that focuses on specialized CHR-P clinical services [Reference de Pablo, Estradé, Cutroni, Andlauer and Fusar-Poli22] is the mainstream approach to overcome these barriers and advance clinical research to foster translational innovations in this field [Reference Fusar-Poli, de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt7]. Successful examples come from large-scale initiatives, such as the Australian and North American CHR-P consortia [Reference Addington, Liu, Brummitt, Bearden, Cadenhead and Cornblatt23], which are currently missing in Italy.
The primary aim of the current study is to fill this gap by presenting an innovative ITAlian partnership for psychosis prevention (ITAPP). The core findings will be discussed to provide directions to advance and implement clinical research collaborations in the CHR-P field in Europe, and therefore advance knowledge for the potential benefit of many young people at risk of developing this disorder.
Methods
This manuscript originates from a workshop on CHR-P services in Italy, held on two occasions (October 2, 2019: Italian Society of Biological Psychiatry; February 21, 2020: Società Italiana di Psicopatologia). Leading clinical and academic centers for psychosis prevention in Italy (Pavia, Milan, Perugia, Bari, and Naples) attended the workshop. We leveraged an empirical framework (internationally validated by our team [Reference de Pablo, Estradé, Cutroni, Andlauer and Fusar-Poli22]) for describing core characteristics of CHR-P services (Table 1): (a) type of CHR-P service (i.e., standalone vs. integrated model), catchment area, and pathways to care (i.e., outreach strategies and sources of referral); (b) service users; and (c) interventions and outcomes (i.e., psychosis onset, functioning, and persistence/remission of symptoms). For standalone CHR-P services, we defined a separate team that works independently from other generic community mental health teams. For integrated CHR-P services, we defined a team wholly embedded into community mental healthcare services, with professionals that adopt principles of early intervention in psychosis [Reference Schirmbeck, van der Burg, Blankers, Vermeulen, McGuire and Valmaggia24].
Table 1. Characteristics of the ITAPP sites.
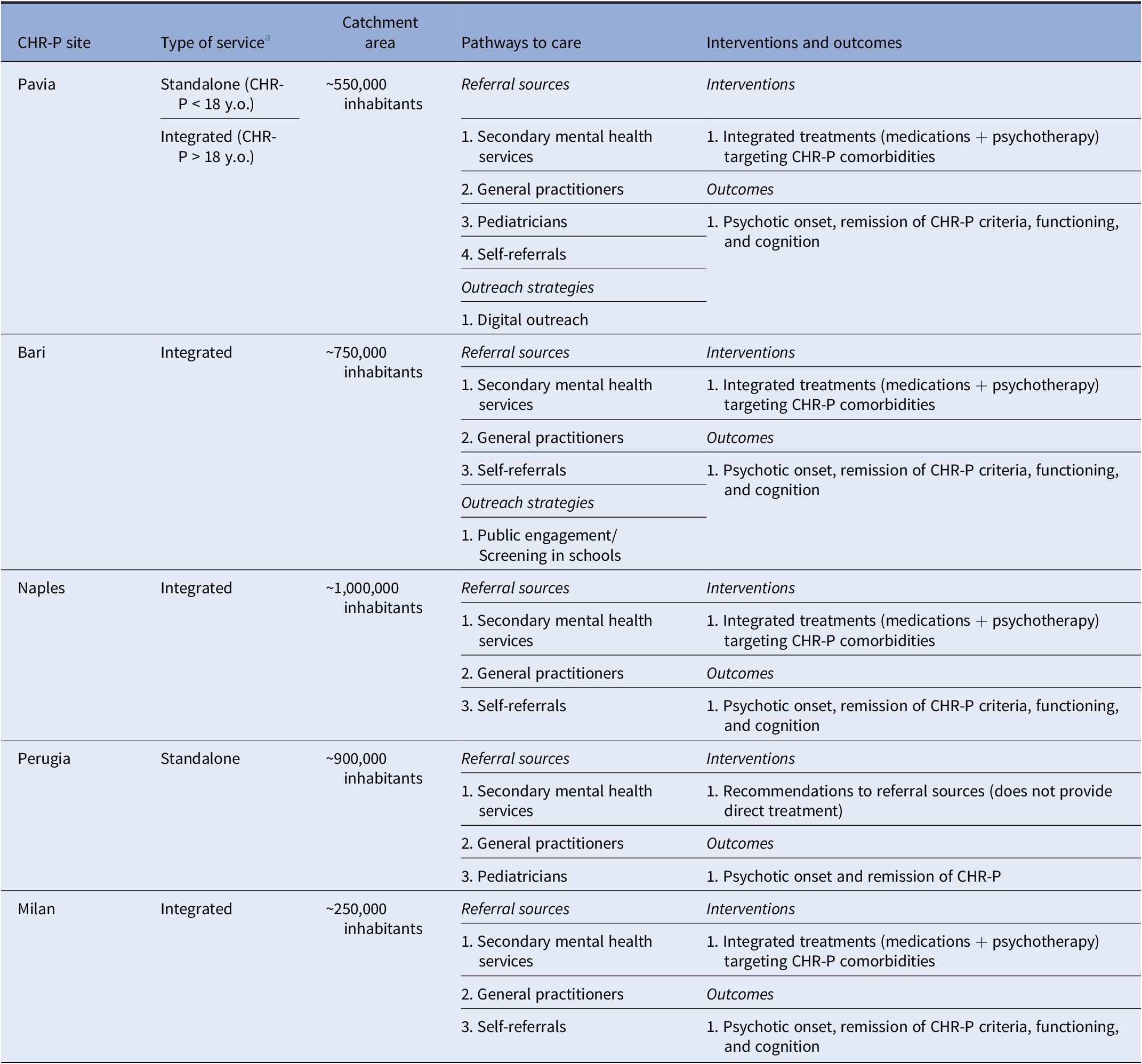
Abbreviations: CHR-P, clinical high risk for psychosis; ITAPP, ITAlian partnership for psychosis prevention.
a Standalone or integrated CHR-P services. For standalone CHR-P services, we defined a separate team that works independently from other generic community mental health teams. For integrated CHR-P services, we defined a team wholly embedded into community mental healthcare services, with professionals that adopt principles of early intervention in psychosis.
When available, quantitative data were descriptively summarized using mean (and median) and SD for continuous variables and frequencies for categorical variables. Furthermore, for each CHR-P service, we collected the baseline sample size, the individual follow-up time, and the number of events (transition to psychosis from a CHR-P stage). The ascertainment of the CHR-P state and psychotic onset were determined through standardized psychometric instruments, including the comprehensive assessment of at-risk mental state (CAARMS) [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell’Olio25]; the structured interview for prodromal syndrome (SIPS) [Reference Pandurangi26]; the schizophrenia proneness instrument, adult version (SPI-A) [Reference Fux, Walger, Schimmelmann and Schultze-Lutter27]; and the schizophrenia proneness instrument, child and youth version (SPI-CY) [Reference Fux, Walger, Schimmelmann and Schultze-Lutter27], in line with international clinical practice in this field [Reference Fusar-Poli, de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt7]. Assessment of substance misuse was based on local healthcare guidelines (mainly laboratory diagnostic and anamnesis). Substance misuse was not an exclusion criterion during assessment procedures. The cumulative incidence risk of transition to psychosis during the follow-up period was estimated with Kaplan–Meier survival analysis. These data were then plotted and analyzed with a failure function (1-Kaplan–Meier) across the overall ITAPP sample, and point estimates were reported for each year. A failure function was also used to illustrate the pattern of transition risk across ITAPP centers. The Kaplan–Meier was truncated when less than 10 CHR-P individuals were still at risk. Analyses were performed using STATA16, and p-value was set to 0.05 two-sided.
Results
CHR-P center in Pavia
Service, catchment area, and pathways to care
The CHR-P center in Pavia encompasses two main sites: a child and adolescent neuropsychiatric unit and an outpatient clinic for young adults.
The child and adolescent neuropsychiatry unit at the IRCCS Istituto Neurologico Casimiro Mondino was set up in 2007. This unit offers assessment and preventive care to help-seeking children and adolescents under the age of 18 years as part of an integrated team adopting principles of early intervention in the context of existing mental health services. The outpatient clinic is a standalone CHR-P service set up in 2019 at the Department of Brain and Behavioral Sciences. This service targets young adults (aged 18–35) with potentially emerging severe mental disorders (including bipolar and depression) and works closely with local adult psychiatric mental health services.
The research activities of these two units are embedded with those of the University of Pavia. The clinical team includes psychiatrists, psychologists, nurses, trainees, and social workers. The catchment area extends from Pavia and its surroundings (545,888 inhabitants) to the Lombardy region (10,060,000 inhabitants), with additional CHR-P referrals routinely received from all over Italy.
The primary referral sources for CHR-P are pediatricians, general practitioners, other child and adolescent mental health services in the community, and self-referrals. This center is implementing a digital outreach for CHR-P.
Service users
This center treated 129 CHR-P individuals over the past years. Being mainly embedded in child and adolescent mental health services, CHR-P mean age and age range in this site are lower than those observed in the other Italian sites (Table 2). The assessment is based on the CAARMS. The large majority (98.4%) of CHR-P individuals met criteria for attenuated psychosis symptoms (APSs), and a minority had ever used substances (18.7%; see also Table 2). CHR-P criteria were often comorbid with other psychiatric diagnoses, the most prevalent ones being personality disorders (36.8%), major depressive disorders (27.5%), and generalized anxiety disorders (15%).
Table 2. Baseline sociodemographic and clinical characteristics of CHR-P individuals in the ITAPP.
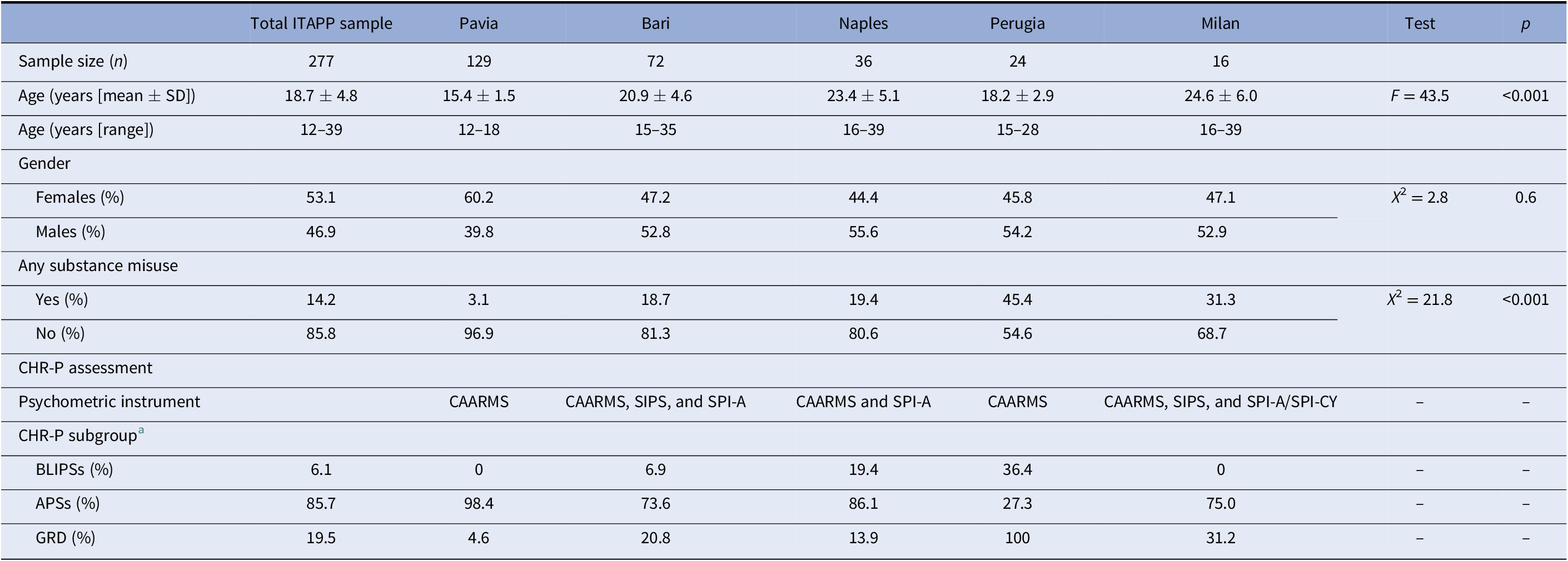
Abbreviations: APS, attenuated psychotic symptom; BLIPS, brief limited intermittent psychotic symptom; CAARMS, comprehensive assessment of the at-risk mental state; CHR-P, clinical high risk for psychosis; GRD, genetic risk and deterioration syndrome; ITAPP, ITAlian partnership for psychosis prevention; SIPS, structured interview for prodromal symptoms; SPI-A, schizophrenia proneness instrument, adult version; SPI-CY, schizophrenia proneness instrument, child and youth version.
a Subgroups may overlap, so the total count is not 100%.
Interventions and outcomes
CHR-P individuals are actively followed up over time. A yearly routine CAARMS assessment is offered to all individuals, with contingent assessments upon eventual clinical deterioration. The main outcomes of interest are psychotic onset, functioning (global, role, and social), cognition, persistence/remission of CHR-P criteria, and mental health comorbidities.
This center provides integrated interventions (medications alone, medications + psychotherapy, psychotherapy alone, and psychosocial support), which are mainly aimed at improving the mental health of young CHR-P individuals and their comorbidities.
CHR-P center in Bari
Service, catchment area, and outreach
The Individuazione Precoce del Rischio Psicotico(IPRR) CHR-P center is a section of a general adult mental health service. It was set up in 2015 to offer assessment and preventive care to help-seeking young adults (aged 18 and above). The is an integrated service that adopts principles of early intervention in the context of an outpatient clinic dedicated to the treatment of psychotic disorders. The research activities of are embedded with those of the University of Bari. The clinical team includes psychiatrists, psychologists, and social workers. The catchment area includes Bari metropolitan area (more than 750,000 inhabitants) and further extends to the whole region of Puglia, Italy (more than 4 million inhabitants).
The main referral sources are local mental health services and general practitioners. The also provides outreach activities to improve pathways to care for CHR-P such as public engagement and screening activities in school and scheduled outreach sessions in local mental health services.
Service users
The treated 72 CHR-P individuals over the past years. This unit employs the CAARMS, the SIPS, and the SPI-A. In this site, the large majority (73.6%) of CHR-P individuals met the APS criteria, and a small minority had ever used substances (14.2%; see also Table 2). CHR-P criteria were often comorbid with other psychiatric diagnoses, but these comorbid diagnoses are not systematically recorded.
Interventions and outcomes
The mainly offers psychotherapy interventions and medications (at minimal effective dose) when required. The main outcomes of interest are psychotic onset, functioning, cognition, persistence/remission of CHR-P criteria, and mental health comorbidities.
CHR-P center in Naples
Service, catchment area, and outreach
The CHR-P center in Naples is a section of a general adult mental health service. It was set up in 2015 to offer assessment and preventive care to help-seeking young adults (aged 18 and above). This CHR-P center is an integrated service that adopts principles of early intervention in the context of an outpatient clinic dedicated to the treatment of psychotic illness. The research activities of this center are embedded with those of the University of Campania Vanvitelli. The team includes academic personnel (clinical academics and PhD students), psychiatrists (consultants and trainees), psychologists, nurses, and social workers.
The catchment area consists of an established network of 13 mental health departments located in the city of Naples and across the Campania region (from 164,000 to 1,000,000 inhabitants). The main referral sources are mental health professionals, emergency departments, liaison psychiatry, general practitioners, and self-referrals.
Service users
The Vanvitelli outpatient unit for psychotic disorders screens about 500 patients every year. Approximately, 5% of these patients are CHR-P. This center treated 36 CHR-P individuals over the past years.
This unit uses the CAARMS and the SPI-A. The large majority (86.1%) of CHR-P individuals met the APS criteria, and a minority had ever used substances (19.4%; see also Table 2). More than half CHR-P individuals (52.8%) had psychiatric comorbidity, the most prevalent being generalized anxiety disorder and panic disorder.
Interventions and outcomes
Most CHR-P individuals are offered psychotherapy, cognitive remediation, and psychoeducation. Medications are also frequently used, most often in combination with psychotherapy. The use of medications is mainly intended to treat mental health comorbidities. The main outcomes of interest are psychotic onset, functioning, cognition, persistence/remission of CHR-P criteria, and mental health comorbidities. CHR-P individuals are followed up over time with clinical interviews to identify outcomes of interest. There is no defined follow-up duration. Up to now, the longest follow-up has been 58 months (range: 2–58; mean: 17).
CHR-P center in Perugia
Service, catchment area, and outreach
The Centre for Translational, Phenomenological and Developmental Psychopathology (CTPDP) is an outpatient unit, which was set up in 2018. The recruitment targets of this center are children, adolescents, and young adults (age range: 11–25 years), and it consists of a standalone second-level outpatient unit performing early differential diagnosis, monitoring and treatment supervision advice in synergy with the network of local services across Umbria Region. The research activities of the CTPDP are embedded with those of the University of Perugia. Due to the circumscribed staffing of the clinical team, which includes an academic psychiatrist (25% of time), two residents (20% of time), and two volunteer psychologists in rotational training (25% of time), integrated community treatment is performed through the referring network of local MH services following consolidated local practices and habits. The catchment area of the CTPDP is the Italian region of Umbria (about 900,000 inhabitants). The CTPDP has a pan-regional outreach receiving referrals from the two local National Health Service Trusts. The referral sources are local mental health services across the Umbria region which also scrutinize potential referrals from general practitioners and pediatricians based on clinical need of care.
Service users
The CTPDP included 24 CHR-P individuals (assessed with the CAARMS). About one-third of CHR-P met criteria for brief limited intermittent psychotic symptoms (36.4%) and a substantial proportion of the sample met criteria for genetic risk and deterioration syndrome (see also Table 2). A minority of CHR-P presented other psychiatric comorbidities; these included specific learning disabilities, and obsessive–compulsive disorders.
Interventions and outcomes
The also offers to the referring MH services the opportunity for regular longitudinal follow-up on a semester/annual basis, with the outcome of interests being psychotic onset, hospitalization, and symptoms trajectories.
The CTPDP does not offer direct preventive care to CHR-P, but it provides comprehensive recommendations for treatment to the referring service.
CHR-P center in Milan
Service, catchment area, and outreach
The CHR-P center in Milan is a section of a general adult mental health service located within the Department of Neurosciences and Mental Health of the IRCCS Ca’ Granda Ospedale Maggiore Policlinico. It was set up in 2016 to treat help-seeking adults (aged 18 and above). It is an integrated service that adopts the principles of early intervention within a larger outpatient unit for general adult psychiatry. The clinical team includes psychiatrists, psychologists, nurses, and social workers. The catchment area includes about 250,000 individuals. The main referral sources are mental health professionals, general practitioners, and self (or family)-referrals.
Service users
This center treated 16 CHR-P individuals over the past few years. Standard assessment instruments include the CAARMS, the SIPS, the SPI-A, and the SPI-CY. The large majority (75.0%) of CHR-P individuals met APS criteria, and about one-third had ever used substances (31.3%; see also Table 2). CHR-P criteria were often comorbid with other psychiatric diagnoses, including major depressive disorders, personality disorders, and anxiety disorders.
Interventions and outcomes
CHR-P undergo active monitoring with clinical interviews and cognitive testing scheduled every 3 months for up to 18 months. The main outcomes of interest are psychotic onset, functioning, cognition, persistence/remission of CHR-P criteria, and mental health comorbidities.
The CHR-P center in Milan offers multidisciplinary interventions to CHR-P such as medications, psychotherapy, social skills training, cognitive remediation, and physical exercise.
Baseline sociodemographic and clinical characteristics of the ITAPP
A total of 277 CHR-P individuals were treated within the ITAPP (129 in Pavia, 72 in Bari, 36 in Naples, 24 in Perugia, and 16 in Milan), for up to 6 years (Figure 1), across a total catchment area of approximately 12,960,000 Italian inhabitants. Overall, CHR-P individuals were aged 18.7 years (SD: 4.8; range: 12–39 years), mostly females (53.1%), without any substance abuse (85.8%); more frequently meeting the APS subgroup (85.7%) of the CHR-P state. The main clinical and sociodemographic characteristics of the baseline sample are reported in Table 2. Main differences between sites were: age, with the youngest CHR-P being in Pavia (15.4 ± 5.1) and the oldest in Milan (24.6 ± 6.0); and rates of substance misuse, with the lowest rates in Pavia (3.1%) and the highest in Perugia (45.4%) and Milan (31.3%).
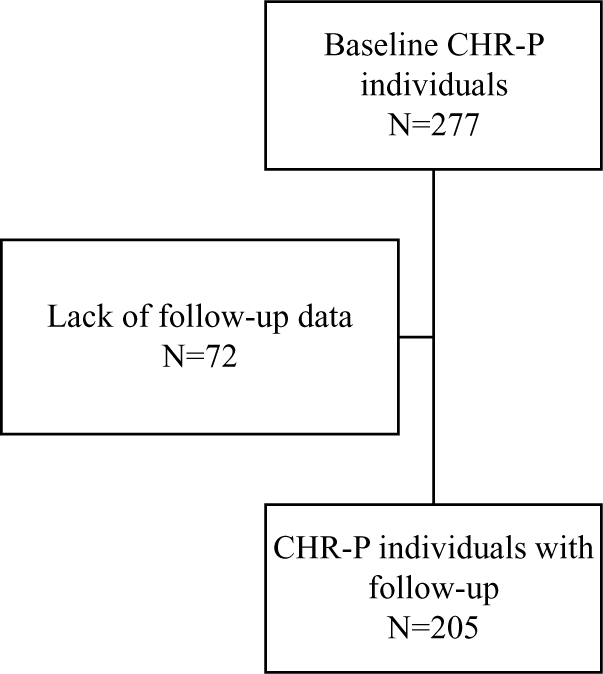
Figure 1. Flowchart of selection of study population.
Longitudinal risk of psychosis onset in the overall ITAPP sample
A total of 205 CHR-P individuals in the ITAPP had follow-up data (Figure 1). Their mean ± SD follow-up time was 663.7 ± 551.7 days (min: 5; median: 429; max: 2361).
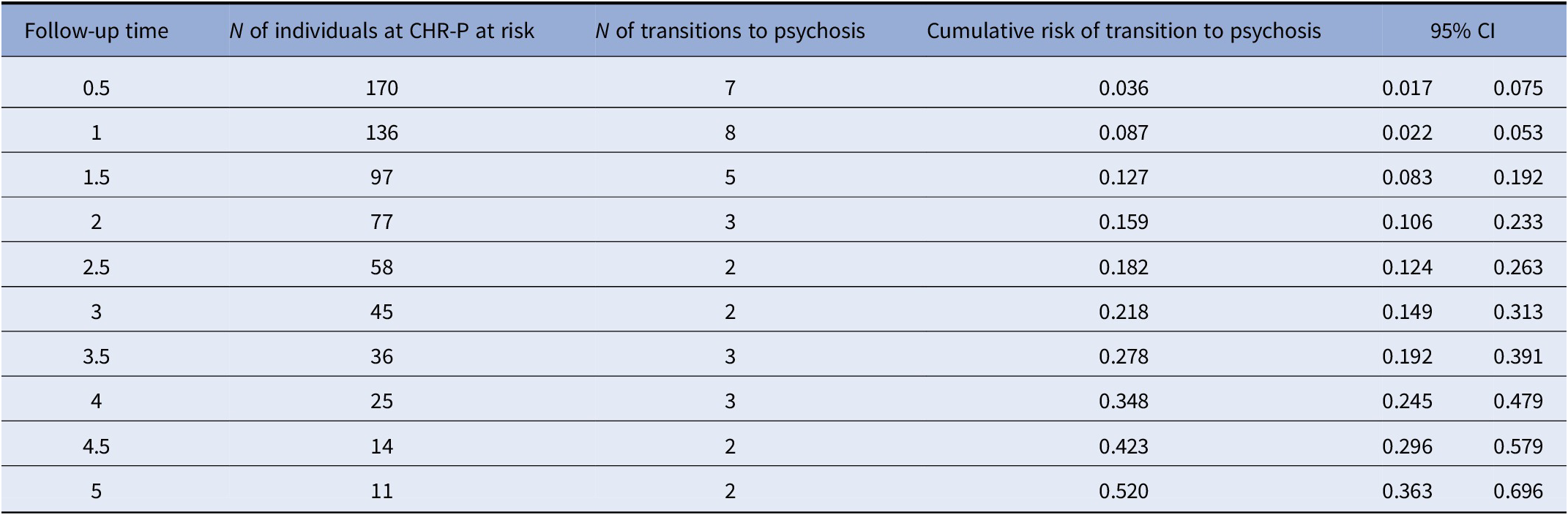
Thirty-seven of the 205 CHR-P subjects transitioned to a first episode of psychosis, with a mean ± SD time to conversion of 673.8 ± 551.8 days (min: 6; median: 407; max: 1764). Those nonconverted were followed up for a mean ± SD of 661.5 ± 553.3 days (min: 6; median: 434; max: 1764). Figure 2 presents the cumulative risk of psychosis in the ITAPP. The cumulative risk of psychosis increased from 8.7% (95% CI 5.3–14.1) at 1 year to 15.9% (95% CI 10.6–23.3) at 2 years, 21.8% (95% CI 14.9–31.3) at 3 years, 34.8% (95% CI 24.5–47.9) at 4 years, and 51.9% (95% CI 36.3–69.6) at 5 years (see also Table 3). As highlighted in Figure 2, the main between-site differences were noted in the Perugia site, with most events (transition to psychosis) occurring during the first year of follow-up and in Pavia, where the majority of events occurred in Years 3 and 4. The other three sites (Bari, Naples, and Milan) showed similar failure curves.
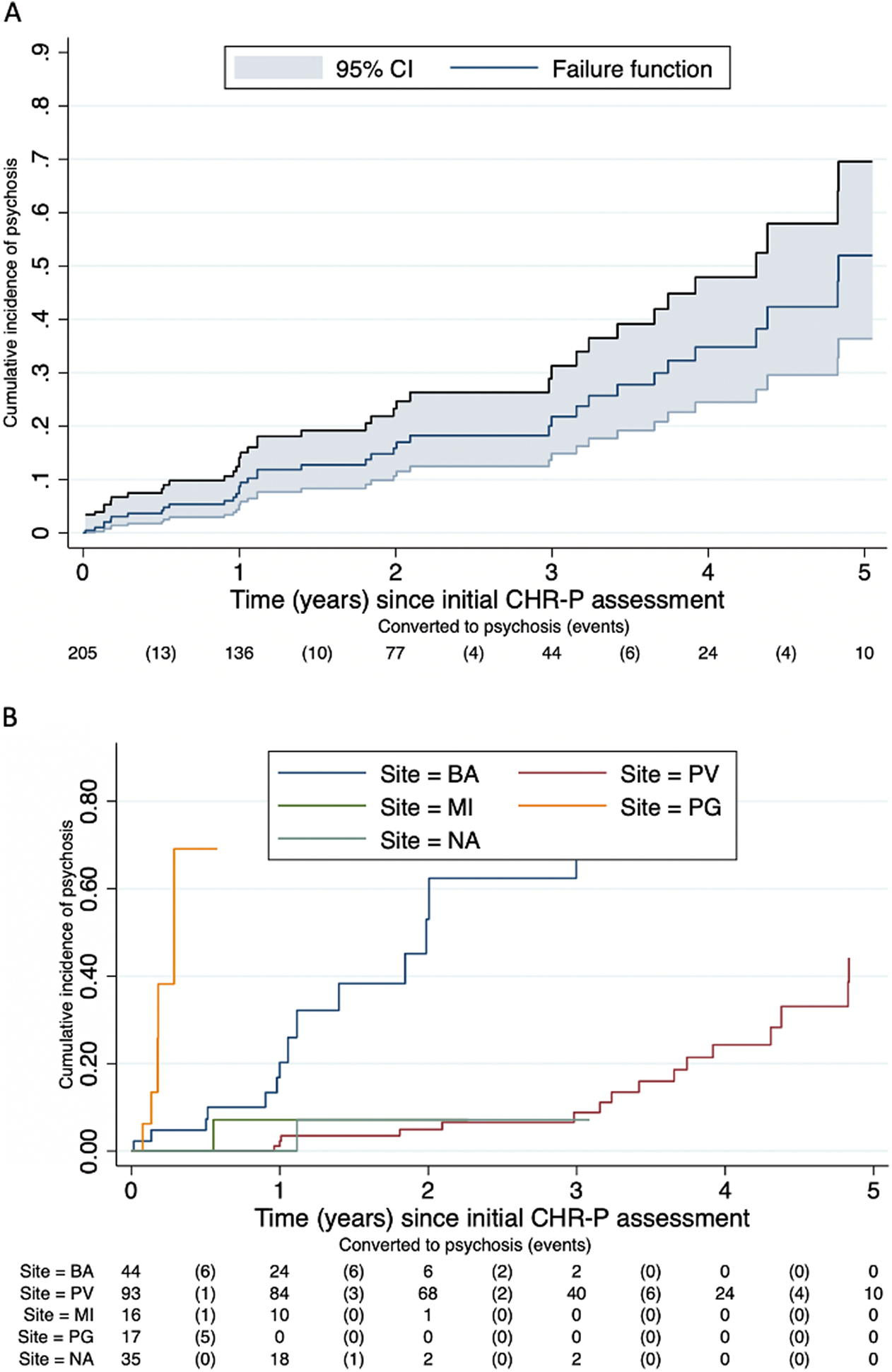
Figure 2. Cumulative incidence of psychosis in the ITAPP. (A) Overall sample. (B) By the ITAPP center.
Abbreviations: BA, Bari; MI, Milan; NA, Naples; PG, Perugia; PV, Pavi.
Table 3. Number of transitions to psychosis and cumulative risk of transition over follow-up in the ITAPP.
Abbreviations: CI, confidence interval; CHR-P, clinical high risk for psychosis; ITAPP, ITAlian partnership for psychosis prevention.
Discussion
The ITAPP included five CHR-P centers across Italy, with an overall recruitment capacity of 277 CHR-P individuals. All centers had strong academic links, were multidisciplinary, and provided care to both adolescents and young adults (transitional) mainly recruited through existing healthcare services. The CAARMS was the most widely used assessment instrument, while the duration of follow-up, type of outreach, and provision of preventive interventions were highly heterogeneous. Across 205 CHR-P individuals with follow-up, the cumulative risk of psychosis was 51.9% at 5 years.
The five ITAPP CHR-P centers were set up between 2007 and 2018 across Northern, Central, and Southern Italy, serving a total population of about 13 million inhabitants. All centers were linked to academic departments and conducting research (see below). All ITAPP centers were targeting a transitional age (12–39 years), with minor variations across sites. This is relevant, because a large-scale meta-analysis found that 12.3% of psychotic disorders occur before the age of 18 and 47.8% before 25, with a peak onset at 20.5 years [Reference Solmi, Radua, Olivola, Croce, Soardo and de Pablo28]. These findings do not support the current pediatric–adult bifurcation of mental health services (cut at the age of 15 or 18) in Italy, where young people may fall into institutional gaps when they are most liable to mental disorders [Reference Fusar-Poli, Correll, Arango, Berk, Patel and Ioannidis29]. By overcoming this limitation, the ITAPP represents a promising template for transitional mental health services [Reference Fusar-Poli, Spencer, De Micheli, Curzi, Nandha and McGuired4] aimed at early detection and intervention [Reference Kotlicka-Antczak, Podgórski, Oliver, Maric, Valmaggia and Fusar-Poli3]. In line with these considerations, ITAPP services were enriched with multidisciplinary teams and approaches.
The outreach activity across ITAPP centers was heterogeneous. Most centers relied on secondary mental healthcare and a minority on primary care. Community outreach efforts were present, but limited by challenges such as the dilution of risk-enrichment and the invalidity of CHR-P assessment in the general population [Reference Fusar-Poli, Rutigliano, Stahl, Schmidt, Ramella-Cravaro and Hitesh10,Reference Fusar-Poli12].
CHR-P recruited in ITAPP appeared slightly younger (mean age: 18.7 years) and more frequently females (53.1%) than the average CHR-P population (meta-analytic mean age: 20; 55.28% males) [Reference de Pablo, Radua, Pereira, Bonoldi, Arienti and Besana15]. These differences are likely due to the substantive child and adolescent mental health service component of the ITAPP.
All ITAPP centers employed the CAARMS, with a minority additionally using the SIPS and the SPI-A/SPI-CY. There is no evidence that using different CHR-P instruments impacts the probability of developing psychosis [Reference de Pablo, Radua, Pereira, Bonoldi, Arienti and Besana15]. In line with meta-analytic evidence on CHR-P, most (~85%) CHR-P in the ITAPP presented with attenuated psychotic symptoms [Reference Fusar-Poli, de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt7]. In the light of the relatively young age, most (~85%) of the ITAPP cohort did not present significant substance abuse. These general characteristics are informative in the context of the sampling biases that often affect CHR-P studies: unsystematic detection of CHR-P based on referrals made on suspicion of psychosis risk by heterogenous sources [Reference Fusar-Poli, Schultze-Lutter, Cappucciati, Rutigliano, Bonoldi and Stahl30]. These idiosyncratic sampling strategies lead to significant risk enrichment (about 15% risk of psychosis onset at 48 months) [Reference Fusar-Poli, Schultze-Lutter, Cappucciati, Rutigliano, Bonoldi and Stahl30] during the recruitment of young individuals undergoing CHR-P assessment [Reference Fusar-Poli, de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt7].
All ITAPP centers but one provide preventive care: psychotherapy (including psychodynamic approaches), psychosocial support, medications, cognitive remediation, physical exercise, and their combination. Therapies were heterogenous across sites, but they all aimed at treating presenting CHR-P symptoms or their mental comorbidities. While all ITAPP services routinely incorporate comprehensive needs-based interventions, only a few implemented public health initiatives to foster mental health literacy and promote good mental (e.g., resilience and good lifestyle behaviors) and physical health [Reference Fusar-Poli, de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt7]. Such heterogeneity may reflect the lack of robust evidence to favor any specific intervention to improve outcomes of CHR-P individuals and the absence of national clinical guidelines for the prevention of psychosis. Interestingly, most ITAPP centers provided comprehensive monitoring of outcomes encompassing psychotic onset, functioning (global, role, and social), cognition, persistence/remission of CHR-P criteria and symptom trajectories, hospitalization, and mental comorbidities, although the instruments used to measure these outcomes were unstandardized and heterogeneous across sites. The follow-up period was also heterogeneous across sites, with a mean length of about 1.5 years and a maximum of 6 years (Pavia site). The follow-up of our cohort aligned with the average follow-up observed worldwide [Reference de Pablo, Estradé, Cutroni, Andlauer and Fusar-Poli22], which is typically not sufficient to capture the long-term outcomes of this patient population [Reference Fusar-Poli, De Micheli, Signorini, Baldwin, de Pablo and McGuire16].
The transition risk to psychosis in ITAPP was at the highest in the first months after the initial CHR-P assessment and it did not plateau until about 4 years, in line with recent meta-analytic analyses in this field, showing that 25% of individuals at CHR-P developed psychosis within 3 years and that transition risk continued increasing in the long term [Reference de Pablo, Radua, Pereira, Bonoldi, Arienti and Besana15]. These findings are also in line with the evidence that the probability of developing other severe real-world outcomes in CHR-P individuals (e.g., risk of hospital admission and increase in psychotropic medications) doubles from the short to the long term [Reference Fusar-Poli, De Micheli, Signorini, Baldwin, de Pablo and McGuire16].
We noticed differences in the cumulative risk of psychosis across different ITAPP sites. These differences might be related to the heterogeneous recruitment and sampling procedures across sites, which resulted in heterogeneous sociodemographic characteristics (i.e., age, substance misuse, and CHR-P subgroup) of CHR-P individuals (Table 2). This heterogeneity further suggests that only large-scale recruitment efforts can provide an accurate representation of real-word scenarios in CHR-P research and provide further strength to the ITAPP initiative.
Conducting long-term follow-ups emerged as core empirical barrier to implementing CHR-P services in the national healthcare system. Additional challenges encompassed difficulties in CHR-P detection [Reference Fusar-Poli, Sullivan, Shah and Uhlhaas31], the need to reinforce the liaison with schools, universities, general hospitals, and practitioners, the lack of standardized training for staff, and the fragmentation of child/adult and general adult/addiction mental health services. A shared constrain of the ITAPP centers was the lack of dedicated funding and limited human resources to upscale the detection, prognosis, and preventive activity.
Despite these crucial challenges, most ITAPP centers are actively conducting CHR-P research. This level of activity includes implementation studies [Reference Spada, Molteni, Pistone, Chiappedi, McGuire and Fusar-Poli32], local cohort studies encompassing psychopathology, neurocognition, neuroimaging to improve prediction of outcomes [Reference Molteni, Filosi, Mensi, Spada, Zandrini and Ferro33], evidence-based medicine analyses of the CHR-P literature [Reference de Pablo, Radua, Pereira, Bonoldi, Arienti and Besana15], [Reference de Pablo, De Micheli, Nieman, Correll, Kessing and Pfennig34][Reference Fusar-Poli, Tantardini, de Simone, Ramella-Cravaro, Oliver and Kingdon35][Reference Raballo, Poletti, Preti and Parnas36], and prospective studies validating the prognostic accuracy of CHR-P criteria such as the DSM-5 APS [Reference Mensi, Molteni, Iorio, Filosi, Ballante and Balottin37]. Furthermore, some ITAPP centers have participated in international CHR-P studies, such as PRONIA [Reference Koutsouleris, Kambeitz-Ilankovic, Ruhrmann, Rosen, Ruef and Dwyer17] and PSYSCAN [Reference Tognin, van Hell, Merritt, Winter-van Rossum, Bossong and Kempton38], or are founding members of the international clinical research infrastructures, such as the European College of Neuropsychopharmacology Prevention of Mental Disorders and Mental Health Promotion Network [Reference Fusar-Poli, de Pablo, De Micheli, Nieman, Correll and Kessing39,Reference Fusar-Poli, Bauer, Borgwardt, Bechdolf, Correll and Do40].
The ITAPP initiative has therefore the potential to significantly advance and implement clinical research collaborations in the CHR-P field in Italy, in Europe, and worldwide.
The current data indicate that the ITAPP centers have the capacity to recruit meaningful samples of CHR-P individuals on the national level, to follow them up with established instruments and to offer them potentially preventive interventions. At the same time, the current study highlights important barriers to large-scale implementation of CHR-P prevention such as the lack of a standard data acquisition dataset to record individual participant data and the need of more effective interventions. Future directions include establishing a national CHR-P program using harmonized assessment and follow-up measurements and testing the feasibility of standardized preventative interventions (e.g., good cannabinoids) across the whole ITAPP CHR-P population.
Conclusions
The ITAPP is one of the few CHR-P clinical research partnerships in Europe for fostering detection, prognosis, and preventive care, as well as for translating research innovations into practice.
Acknowledgment
Nothing to disclose.
Conflict of Interest
The authors declare none.
Financial Support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
Conceptualization: P.F.-P., P.B., A.R., and S.G.; Data curation: P.F.-P., A.M., and P.B.; Formal analysis: P.F.-P., A.M., and A.R.; Funding acquisition: P.F.-P.; Investigation: A.R. and S.G.; Methodology: P.F.-P.; Project administration: P.F.-P.; Resources: A.R., A.B., and S.G.; Supervision: P.F.-P., A.B., and S.G.; Writing—original draft: all authors; Writing—review & editing: all authors.
Data Availability Statement
The authors did not give permission to share data.








Comments
No Comments have been published for this article.