No CrossRef data available.
Published online by Cambridge University Press: 19 July 2023
During the COVID 19 pandemic children and young people (CYP) faced significant restrictions. The virus and restrictions also affected how health services could function, including mental health. Research analysing the COVID 19 pandemic is important to ensure dynamic and resilient service design in case of future national emergencies.
To investigate the impact of COVID-19 lockdowns on CYP psychiatric admission trends during lockdowns 1 (started 26 March 2020) and 2 (started 20 November 2020) of the COVID 19 pandemic in England.
Routinely collected, retrospective, English, administrative data looking at the CYP hospital admissions, length of stay and patient demographics were analysed using an interrupted time series analysis to compare pre-pandemic service use with service use during COVID 19 lockdowns 1 and 2. The analysis used an ordinary least squares (OLS) approach with Newey–West standard errors to handle autocorrelation and heteroscedasticity.
Table 1.
| Variable | Pre-pandemic | Post-pandemic | Total sample |
|---|---|---|---|
| (n=1,156) | (n=94) | (n=6,250) | |
| Mean age at admission (SD) [Median; IQR] | 15.3 (1.7) [16;3] | 15.6 (1.6) [16;2] | 15.3 (1.7) [16;3] |
| Gender | |||
| Female | 70% | 72% | 70% |
| Missing | 1% | 2% | 1% |
| BAME background | |||
| Yes | 18% | 18% | 18% |
| Missing | 7% | 6% | 7% |
| Looked after | |||
| Yes | 11% | 8% | 11% |
| Missing | 14% | 13% | 14% |
| In full education | |||
| Yes | 43% | 34% | 43% |
| Missing | 35% | 47% | 35% |
| Mean number of admissions per patient (SD) [Median; IQR] | 1.7 (1.2) [1;1] | 1.2 (0.6) [1;0] | 1.7 (1.2) [1;1] |
| Mean length of stay (SD) [Median; IQR] n | 93 (94) [68;94] 6,065 | 65 (65) [43;77] 71 | 93 (94) [67;94] 6,136 |
| Mean number of out-of-area admissions per patient (SD) [Median; IQR] | 0.48 (0.8) [0;1] | 0.33 (0.6) [0;1] | 0.48 (0.80) [0;1] |
SD: standard deviation; IQR: Interquartile range
Image:
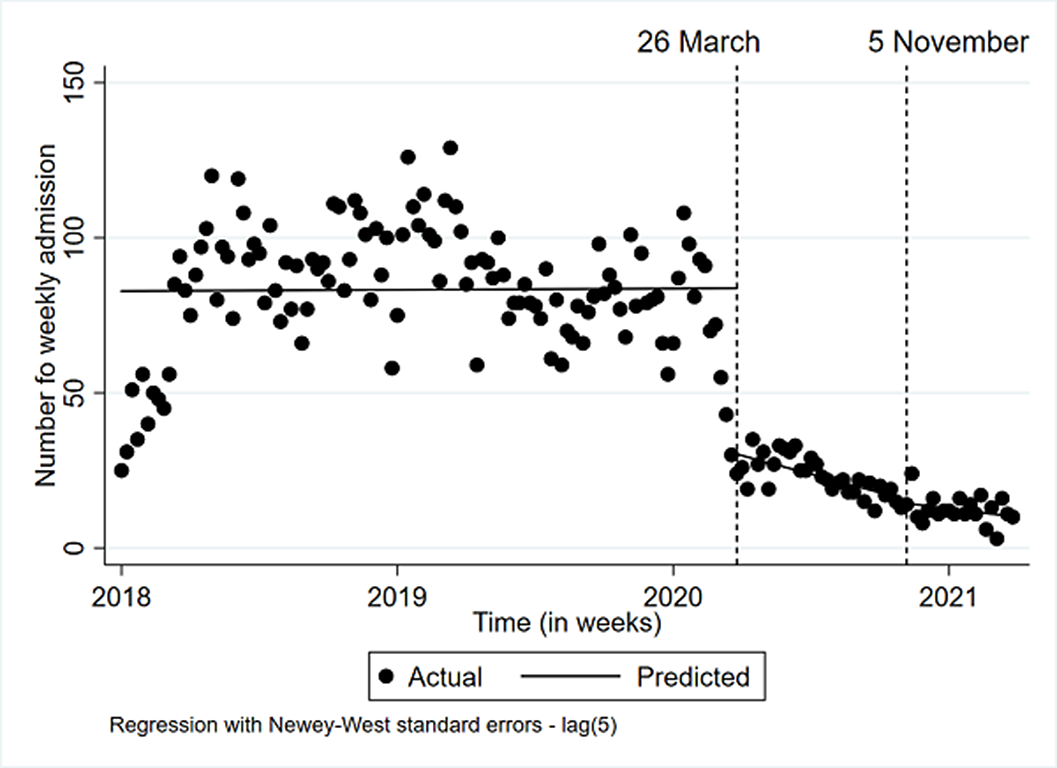
Image 2:
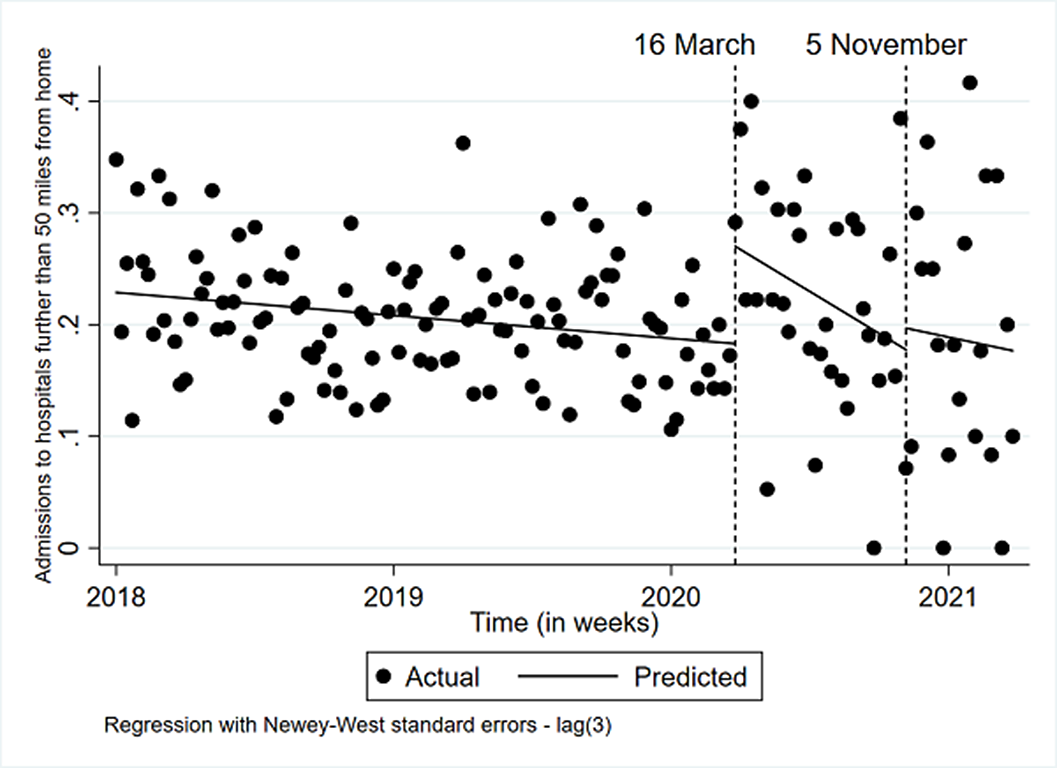
Image 3:
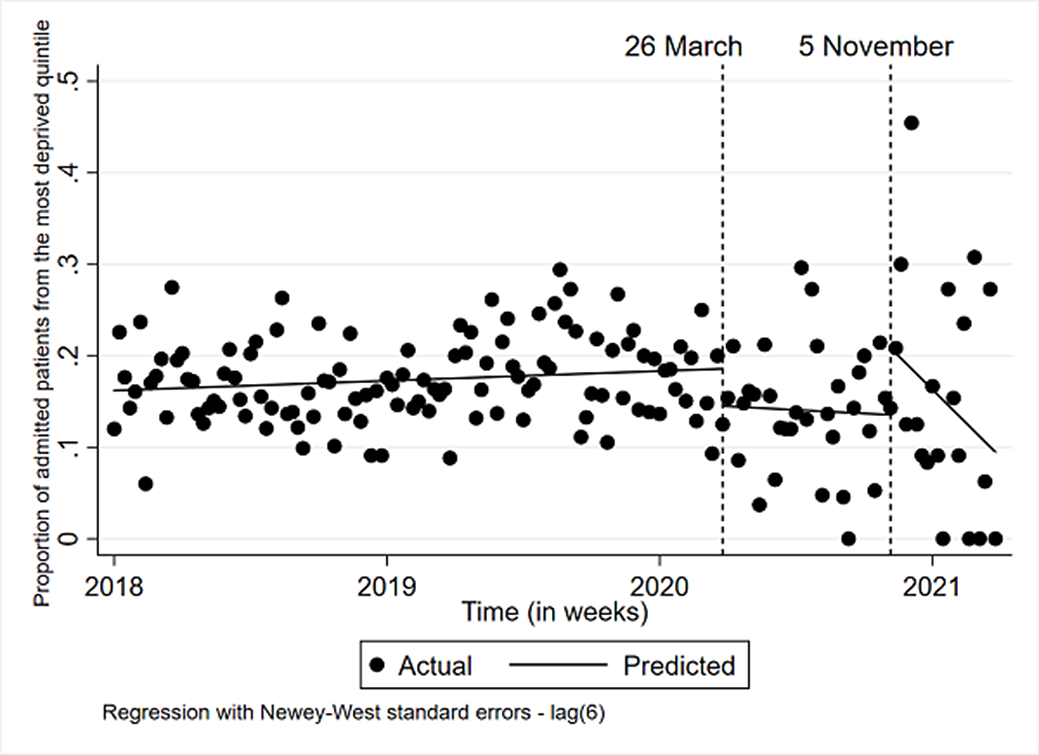
During lockdown 1 and 2, psychiatric admissions for CYP were fewer and shorter. The rise in admissions for more deprived CYP and looked after children suggests these CYP may have been disproportionately affected by the pandemic.
None Declared
Comments
No Comments have been published for this article.