1. Introduction
Psychotic disorders are among the most frequent causes of disability-adjusted life years in adults [Reference Collins, Patel, Joestl, March, Insel and Daar1] and adolescents [Reference Gore, Bloem, Patton, Ferguson, Joseph and Coffey2] and rate second in resulting costs [Reference Olesen, Gustavsson, Svensson, Wittchen and Jönsson3]. Psychotic episodes are mostly preceded by a prodromal phase, in which the onset of clinical high-risk (CHR) symptoms, other mental health (MH) problems, and deficits in psychosocial functioning often leads to help-seeking [Reference Schaffner, Schimmelmann, Niedersteberg and Schultze-Lutter4–Reference von Reventlow, Krüger-Özgürdal, Ruhrmann, Schultze-Lutter, Heinz and Patterson6]. Longer duration of an inadequately treated prodromal phase is associated with negative outcomes of first-episode psychosis (FEP) [Reference Gore, Bloem, Patton, Ferguson, Joseph and Coffey2, Reference Charlson, Ferrari, Santomauro, Diminic, Stockings and Scott7–Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jönsson9]. Therefore, this phase offers a unique point of intervention for an indicated prevention, aimed at reducing CHR symptoms and distress, thereby postponing or preventing manifest psychosis [Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas and Riecher-Rössler10].
Despite direct associations of CHR symptoms with distress and an increased risk for psychosis [Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas and Riecher-Rössler10–Reference Fusar-Poli, Salazar de Pablo, Correll, Meyer-Lindenberg, Millan and Borgwardt13], relative declines in transition rates and high rates of onset and persistence of non-psychotic disorders in CHR populations have been observed [Reference Lin, Yung, Nelson, Brewer, Riley and Simmons11, Reference Fusar-Poli, Bonoldi, Yung, Borgwardt, Kempton and Valmaggia14–Reference Hartmann, Yuen, McGorry, Yung, Lin and Wood16]. This has generated debate regarding diagnostic specificity of CHR in predicting psychosis, with suggestions that it might be pluripotential, indicating risk for developing a range of different psychiatric conditions [Reference McGorry17, Reference McGorry18]. Consequently, it was proposed that the CHR state be redefined as a transdiagnostic at-risk mental state (e.g., Clinical At-Risk Mental State; CHARMS [Reference Hartmann, Nelson, Spooner, Paul Amminger, Chanen and Davey19]), allowing for the identification of early signs of multiple severe mental disorders. However, other studies [Reference Woods, Powers, Taylor, Davidson, Johannesen and Addington20–Reference Schultze-Lutter, Walger, Franscini, Traber-Walker, Osman and Walger23] support the diagnostic specificity of CHR symptoms, indicating that only emergent psychotic disorders significantly differentiate between CHR patients and non-CHR help-seeking controls [Reference Webb, Addington, Perkins, Bearden, Cadenhead and Cannon21], and that the onset and persistence of non-psychotic disorders occur at a similar frequency in both groups, suggesting that a CHR status does not specifically represent a risk factor for non-psychotic disorders [Reference Webb, Addington, Perkins, Bearden, Cadenhead and Cannon21, Reference Fusar-Poli, Rutigliano, Stahl, Davies, De Micheli and Ramella-Cravaro22].
Therefore, while the question of the diagnostic specificity of CHR status remains open, the clinical significance of CHR – for example, psychological burden, independent of conversion to a full-blown mental disorder, and negative impact on functioning – is undisputed [Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas and Riecher-Rössler10–Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter12, Reference Hartmann, Nelson, Spooner, Paul Amminger, Chanen and Davey19, Reference Woods, Powers, Taylor, Davidson, Johannesen and Addington20, Reference Schultze-Lutter, Walger, Franscini, Traber-Walker, Osman and Walger23], and the inclusion of Attenuated Psychosis Syndrome in Section III of DSM-5 supports its diagnostic and psychopathological relevance [Reference Salazar De Pablo, Catalan and Fusar-Poli24], highlighting the need to focus on offering CHR patients effective interventions. Moreover, irrespective of the debate regarding pluripotentiality of the CHR state, evidence indicates some transdiagnostic relevance of the CHR state (or symptoms) in terms of (at least) comorbidity with other psychiatric disorders and syndromes [Reference Lim, Rekhi, Rapisarda, Lam, Kraus and Keefe25–Reference Raballo, Poletti and Preti27]. This is reflected in new broader transdiagnostic and dimensional psychiatric taxonomies wherein efforts are currently being made to determine the most appropriate way to map CHR for psychosis into these models [Reference Cowan and Mittal28].
Relatedly, other relevant intervention targets for this population include transdiagnostic factors of core beliefs – consisting of locus of control (LOC) and competence beliefs – and coping, demonstrating dysfunctional patterns in CHR [Reference Schmidt, Grunert, Schimmelmann, Schultze-Lutter and Michel29], FEP [Reference Schmidt, Grunert, Schimmelmann, Schultze-Lutter and Michel29, Reference Riera‐López de Aguileta, Vila‐Badia, Usall, Butjosa and Ochoa30], and schizophrenia patients alike [Reference Harrow, Hansford and Astrachan-Fletcher31, Reference Horan, Ventura, Mintz, Kopelowicz, Wirshing and Christian-Herman32], and are regarded as possible predictors of psychosis [Reference Schmidt, Grunert, Schimmelmann, Schultze-Lutter and Michel29]. That is, the hypothesis that typical psychotic symptoms, for example, delusions and hallucinations, result from the use of dysfunctional coping and core beliefs in response to basic symptoms (BS; self-experienced subclinical disturbances in thinking, speech, and perception) [Reference Schultze-Lutter, Ruhrmann, Michel, Kindler, Schimmelmann and Schmidt33] and stressful stimuli [Reference Schultze-Lutter, Debbané, Theodoridou, Wood, Raballo and Michel34].
Beyond their role in CHR, coping and core beliefs are also relevant for general MH quality [Reference Taylor and Stanton35–Reference Mann, Hosman, Schaalma and de Vries37], as reflected by multiple outcomes, including psychopathology, psychosocial functioning, and self-assessment of one’s own health status [38]. Coping is an especially important predictor of MH quality [Reference Taylor and Stanton35, Reference Compas, Jaser, Bettis, Watson, Gruhn and Dunbar39, Reference Kavčič, Avsec and Zager Kocjan40], particularly regarding stress [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36] and representing either a risk (maladaptive coping, including avoidant and emotion-oriented strategies [Reference Richardson, Magson, Fardouly, Oar, Forbes and Johnco41–Reference Wingenfeld, Mensebach, Rullkoetter, Schlosser, Schaffrath and Beblo43]) or protective factor (adaptive coping, including problem-focused and active strategies [Reference Griva and Anagnostopoulos44, Reference Moret-Tatay, Beneyto-Arrojo, Laborde-Bois, Martínez-Rubio and Senent-Capuz45]). LOC is another predictor for MH [Reference Harrow, Hansford and Astrachan-Fletcher31, Reference Hovenkamp-Hermelink, Jeronimus, van der Veen, Spinhoven, Penninx and Schoevers46]: internal LOC (attributing positive events to internal causes and negative ones to external factors such as chance or others) is linked to better MH outcomes and greater resilience [Reference Buddelmeyer and Powdthavee47], while external LOC (the opposite tendency) is associated with psychiatric disorders, including depression and schizophrenia as well as generally poorer functioning [Reference Harrow, Hansford and Astrachan-Fletcher31, Reference Hovenkamp-Hermelink, Jeronimus, van der Veen, Spinhoven, Penninx and Schoevers46, Reference Buddelmeyer and Powdthavee47]. Thus, they can be conceptualized as adaptive and maladaptive, respectively. Finally, competence beliefs, including self-efficacy and self-esteem [Reference Muris, Schmidt, Lambrichs and Meesters48, Reference Thorne, Andrews and Nordstokke49], are strongly associated with MH quality [Reference Mann, Hosman, Schaalma and de Vries37, Reference Schönfeld, Brailovskaia, Bieda, Zhang and Margraf50], with higher competence beliefs being related to better psychosocial functioning [Reference Mann, Hosman, Schaalma and de Vries37, Reference Bandura, Caprara, Barbaranelli, Gerbino and Pastorelli51].
Investigations into the interactions between coping, core beliefs, and MH, involving mainly community samples but also including a minority of clinical samples, have led to contradictory findings in both populations, indicating a mediating role of coping [Reference Backer-Fulghum, Patock-Peckham, King, Roufa and Hagen52–Reference Dieserud, Røysamb, Ekeberg and Kraft54] or of core beliefs [Reference Thorne, Andrews and Nordstokke49, Reference Fryer, Waller and Kroese55, Reference Paterson, Power, Collin, Greirson, Yellowlees and Park56]. A recent meta-analysis [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36] – also mostly, but not exclusively, using community samples – supported a mediation by coping on the influence of core beliefs on MH. Specifically, maladaptive coping mediated the relationship between maladaptive LOC and MH problems. Moreover, both adaptive and maladaptive LOC showed a direct influence on MH problems, independent of coping.
In the present study, we extended the meta-analytical and mediation model [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36] that had mixed community and clinical samples by first exploring alternative structural equation models (SEM) in a community sample and then examining their validity in a clinical sample. In addition to general psychopathology, we focused on CHR symptoms, in virtue of their association with MH quality [Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas and Riecher-Rössler10–Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter12] as well as coping and core beliefs [Reference Schmidt, Grunert, Schimmelmann, Schultze-Lutter and Michel29]. The aims of the present study were:
-
1. To explore the association between core beliefs and MH outcomes, in both a community and a clinical sample, assuming a mediation by coping. Specifically, based on the metanalytical model [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36], we anticipated that the effect of competence beliefs and adaptive LOC on MH outcomes would be mediated by adaptive coping, and that the effect of maladaptive LOC would be mediated by maladaptive coping.
-
2. To investigate the specific placement of CHR symptoms in these interactions.
Based on the metanalytical model [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36], we did not expect relationships between competence beliefs and adaptive LOC, and maladaptive coping or between maladaptive LOC and adaptive coping, and therefore we did not include these relationships in the models.
2. Methods
2.1. Participants and recruitment procedure
Cross-sectional data from a community and a clinical sample were used in the current study. The former comprised 523 participants in the first follow-up assessment of the Bern Epidemiological At-Risk (BEAR) study [Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann57, Reference Schultze-Lutter, Schimmelmann and Michel58], whose core beliefs and coping strategies were evaluated in an add-on study (Supplementary eFigure 1, Supplementary eText 1). Inclusion criteria were absence of a psychotic disorder and fluency in German.
The second sample included 378 patients of the Bern Early Recognition and Intervention Centre for mental crisis (FETZ Bern), assessed between November 2009 and July 2022. Inclusion criteria were informed consent to the use of collected data for scientific purposes, age above 13 years (to allow for the assessment of all BS), and sufficient German-language skills. For more information regarding recruitment and assessment procedures in the BEAR study [Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann57] or FETZ Bern [Reference Michel, Kaess, Flückiger, Büetiger, Schultze‐Lutter and Schimmelmann59], see Supplementary eTexts 1–4.
2.2. Assessments
2.2.1. Mental disorders
The Mini-International Neuropsychiatric Interview (MINI) [Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller60] was used to assess current presence of Axis-I mental disorders according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [61]. The presence of each disorder was indicated by a score of 1 in the corresponding scale; their sum score (0–36) was used in analyses.
2.2.2. CHR symptoms
Two approaches are used for the assessment of CHR states: (i) ultra-high-risk (UHR) criteria and (ii) BS criteria (Supplementary eTable 1). The Structured Interview for Psychosis Risk Syndromes (SIPS) [Reference McGlashan, Walsh and Woods62] was used to assess the presence of UHR symptoms (attenuated (APS) or brief intermittent psychotic symptoms (BIPS)). For each of the positive items (P1–P5; Supplementary eTable1), participants received a score of 1 if they presented symptoms rated between 3 and 5 (APS) or equal to 6 (BIPS), irrespective of whether or not the APS/BIPS in question met requirements for onset/worsening and frequency of the UHR criteria that are very infrequent in the general population [Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann57, Reference McGlashan, Walsh and Woods62]. Scores were then added in a sum score (0–5).
The presence of the BS criteria, cognitive disturbances (COGDIS), and cognitive-perceptive basic symptoms (COPER) was assessed with the Schizophrenia Proneness Instrument–Adult [Reference Schultze-Lutter, Addington, Ruhrmann and Klosterkötter63] and Child and Youth [Reference Marshall, Schultze-Lutter, Marshall and Koch64] versions. Irrespective of the frequency and novelty requirements for BS criteria that are also infrequent in the community [Reference Schultze-Lutter, Ruhrmann, Michel, Kindler, Schimmelmann and Schmidt33], the presence of each criterion-relevant BS (Supplementary eTable1) was indicated by a score of 1, and a sum score (0–14) was obtained.
2.2.3. Self-rated health
Self-rated health was evaluated via the EuroQoL-5D, three-level version (EQ-5D-3L) [Reference Brooks and Group65], assessing three degrees of severity across five dimensions of health, from which we obtained a sum score (0–100) [Reference Hinz, Klaiberg, Brähler and König66, Reference Michel, Schmidt, Schnyder, Flückiger, Käufeler and Schimmelmann67]. Participants’ self-rating of their current health state on the EQ-5D-3L analog scale (0–100, “worst” to “best imaginable health state”) was also included in our models.
2.2.4. Global, social, and occupational functioning
Functioning was assessed with both the Global Assessment of Functioning (GAF) scale, in which psychiatric symptoms are considered, and the Social and Occupational Functioning Assessment Scale (SOFAS) for the evaluation of functioning independently from symptoms [61].
2.2.5. Core beliefs
The German Competence and Control Beliefs Questionnaire (FKK) [Reference Krampen68] was used to evaluate these constructs by means of Self-Concept (FKK-SK; 8 items), Internality (FKK-I; 8 items), and Externality (FKK-PC; 16 items) scales. These were conceptualized in our models as competence beliefs (FKK-SK; as recommended in [Reference Krampen68], see also [Reference Schmidt, Schultze-Lutter, Bendall, Groth, Michel and Inderbitzin69]), adaptive (FKK-I), and maladaptive LOC (FKK-PC; “internality” and “externality” are synonyms for internal, that is, adaptive, and external, that is, maladaptive, LOC, respectively [Reference Harrow, Hansford and Astrachan-Fletcher31, Reference Rotter70]). Analyses were conducted with the normative T-values of each scale’s sum score, obtained from ratings in their respective items on a bipolar six-level scale.
2.2.6. Coping strategies
Positive and negative coping was assessed via the German Stress Coping Questionnaire, adult (SVF-120) [Reference Janke, Erdmann and Kallus71] and children/adolescents (SVF-KJ) [Reference Hampel, Petermann and Dickow72] versions. In each item, the frequency of use of different coping strategies can be rated on a 0–4 Likert scale (“not at all”–“in any case”). In our analyses, we used the relative normative T-values to the sum scores of the global scales Positive and Negative Coping Strategies to represent adaptive and maladaptive coping, respectively.
2.2.7. Sociodemographic variables
Age, level of education, and sex were included in the models as possible confounding variables, the latter only at a later stage during a sensitivity analysis.
Further details regarding instruments can be found in Supplementary eText 5.
2.3. Statistical analyses
Data analyses were performed in RStudio, version 4.1.1, using the lavaan package for preliminary exploratory and confirmatory factor analyses (EFA, CFA) and testing alternative SEMs, and the sempower package for power analysis. The community sample served as the model generation; the clinical sample as model validation sample.
First, an EFA was conducted using variables pertaining to participants’ MH (presence of Axis-I mental disorders and self-rated health) based on Spearman correlation matrices and using Oblimin rotation, allowing intercorrelation of factors. Pairwise deletion was applied, excluding one participant who was missing 20% of the data. Based on EFA results, we proceeded with a two-factor CFA.
Finally, six alternative SEMs were computed using the maximum likelihood estimator [Reference Brown73]. After a pairwise deletion of five observations with missing data, the analysis was conducted on 518 participants from the community sample. Along with the EFA/CFA factors, variables included age, education, standard T-values for competence beliefs (FKK-SK), maladaptive LOC (FKK-PC), adaptive LOC (FKK-I), adaptive and maladaptive coping, presence of BS and APS/BIPS, or alternatively presence of either of CHR symptoms. A Tucker-Lewis index (TLI) ≥0.90, a comparative fit index (CFI) ≥0.95, a standardized root mean square residual (SRMR) ≤0.08, a root mean square error of approximation (RMSEA) ≤0.06, as well as a 90% confidence interval (CI) not containing 0.08 indicate excellent model fit [Reference Bollen74]. As the Chi-squared test is sensitive to sample size and often results in model rejection when working with large samples [Reference Bentler and Bonett75], we focused on the aforementioned indices in evaluating model fit. After comparing the models’ Akaike Information Criterion (AIC) [Reference Akaike, Petrov and Csaki76] and Bayesian Information Criterion (BIC) [Reference Schwarz77], one model was selected as fitting the data best; this was validated in the clinical sample.
The clinical sample (N = 371) presented higher amounts of missing data (9.58%). After applying listwise deletion to 51 participants missing >50% [Reference Madley-Dowd, Hughes, Tilling and Heron78] of their data, we used a multiple imputation method on data missing from the remaining 327 subjects [Reference Patrician79].
To control for sex differences, we conducted a sensitivity analysis by including sex in the chosen model and testing it again in both samples. Here the introduction of a categorical variable in the model required the use of the Weighted least squares and variance-adjusted estimator [Reference Brown73]. We chose this procedure instead of directly including sex in the six alternative SEMs because using this estimator would not have allowed a statistically valid selection of one best-fitting model. Finally, in all samples, we tested all possible mediation pathways indicated in the selected model for significance and calculated their respective 95% bias-corrected bootstrap CIs.
3. Results
3.1. Sample characteristics
The two samples differed in sex (more males in the clinical sample), age, and highest educational level (both lower in the clinical sample), as well as in clinical and functional variables, with lower functioning and more severe psychopathology in the clinical sample (Table 1).
Table 1. Sample characteristics and group comparison
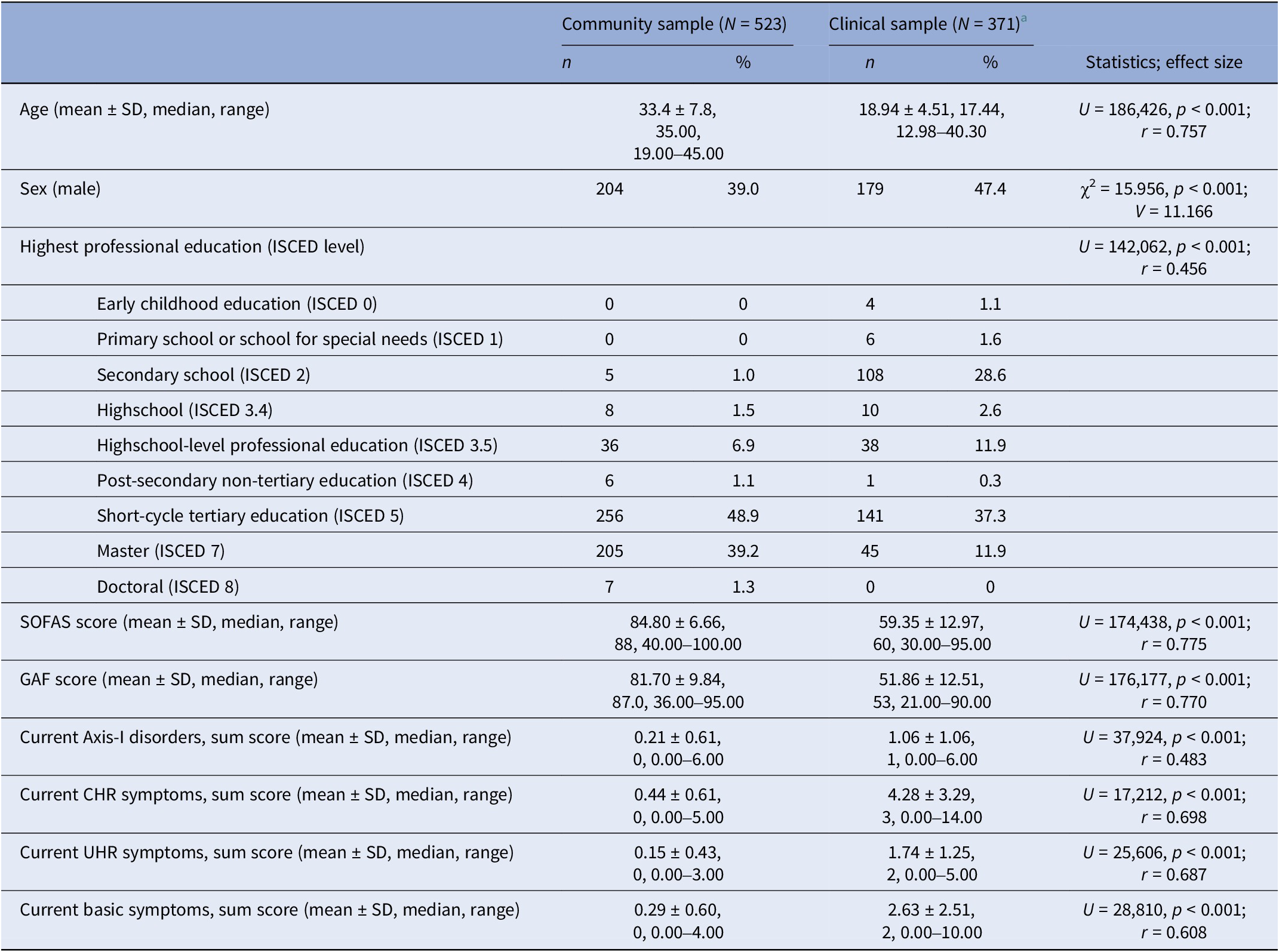
Abbreviations: CHR, clinical high risk; r, Pearson’s r; SOFAS, Social and Occupational Functioning Assessment Scale; UHR, ultra high risk; U, Mann-Whitney U test, V, Cramer’s V; χ2, Chi-squared.
a In the FETZ sample, 18 participants (4.8%) were missing data about their education level (ISCED), 30 participants (7.9%) were missing data about their SOFAS score, 26 participants (6.9%) were missing data about their GAF score, 85 participants (6.9%) were missing data about their current Axis-I disorders, 46 participants (12.2%) were missing data about their current CHR symptoms, 26 participants (6.9%) were missing data about their current UHR symptoms, 45 participants (11.9%) were missing data about their current basic symptoms.
3.2. EFA and CFA in the community sample
Results of the EFA (Supplementary eTable 2) indicate two correlated latent factors (factor correlation 0.34): (i) psychopathology (PP) and (ii) self-rated health (SRH). The model’s fit to the community sample data was excellent overall (RMSR = 0.01, TLI = 0.98, RMSEA = 0.059). The CFA (N = 522) confirmed the two-factor structure (Supplementary eTable 3), showing very good model fit (CFI = 0.996, TLI = 0.990, RMSEA = 0.062, SRMR = 0.032).
3.3. SEM models in the community sample
The resulting latent factors were included in six alternative SEM models (Supplementary eText 6). In all models, positive and negative coping strategies mediated the effect of competence beliefs and adaptive and maladaptive LOC on the latent MH factors PP and SRH.
Fit indices and power ranged from acceptable to excellent, except for TLI, which was equally poor for all models (Supplementary eTable 4). Comparison of their AIC and BIC indices, with emphasis on AIC, indicated model 1.2 (Figure 1, Table 2, Supplementary eTable 5) as best fitting the BEAR data (CFI = 0.923, TLI = 0.863, RMSEA = 0.086, 90% CIs = 0.075, 0.098, SRMR = 0.055, power >0.999, AIC = 39,484.669, BIC = 39,684.418), although model 3.2, with CHR symptoms as an outcome of SHR and PP, had lower BIC (BIC = 39,677.074, AIC = 39,485.825). Though the two models had a similarly good fit to the data, AIC was emphasized in model selection, being more relevant to our testing of a complex system of interactions with unknown underlying structure [Reference Aho, Derryberry and Peterson80], and since BIC can lead to underfitting when working with large samples, non-nested models, and data not following a multivariate normal distribution [Reference Kuha81].

Figure 1. Model 1.2 in the community sample. Rectangles represent observed variables; ovals represent unobserved latent variables; black lines with double-ended arrows represent covariances; black lines with single-ended arrows represent significant paths; dashed gray lines with double- or single-ended arrows represent non-significant covariances or regression paths, respectively; numbers next to the lines indicate coefficients of significant standardized regressions and covariances, or factor loadings; the coefficients of non-significant covariances and regressions are not reported here to facilitate the figure’s interpretation; see Table 2 and Supplementary eTable 5 for further details. CHR: clinical high risk; EQ-5 (100): score on the 0–100 analog scale of the EuroQoL-5D, three-level version (EQ-5D-3L); EQ-5 (sum): sum score on EQ-5D-3L – see Supplementary eText 5 for details; GAF, Global Assessment of Functioning; MINI, Mini-International Neuropsychiatric Interview; SOFAS, Social and Occupational Functioning Scale.
Table 2. Standardized regression coefficients (β) and p values for relevant paths in model 1.2
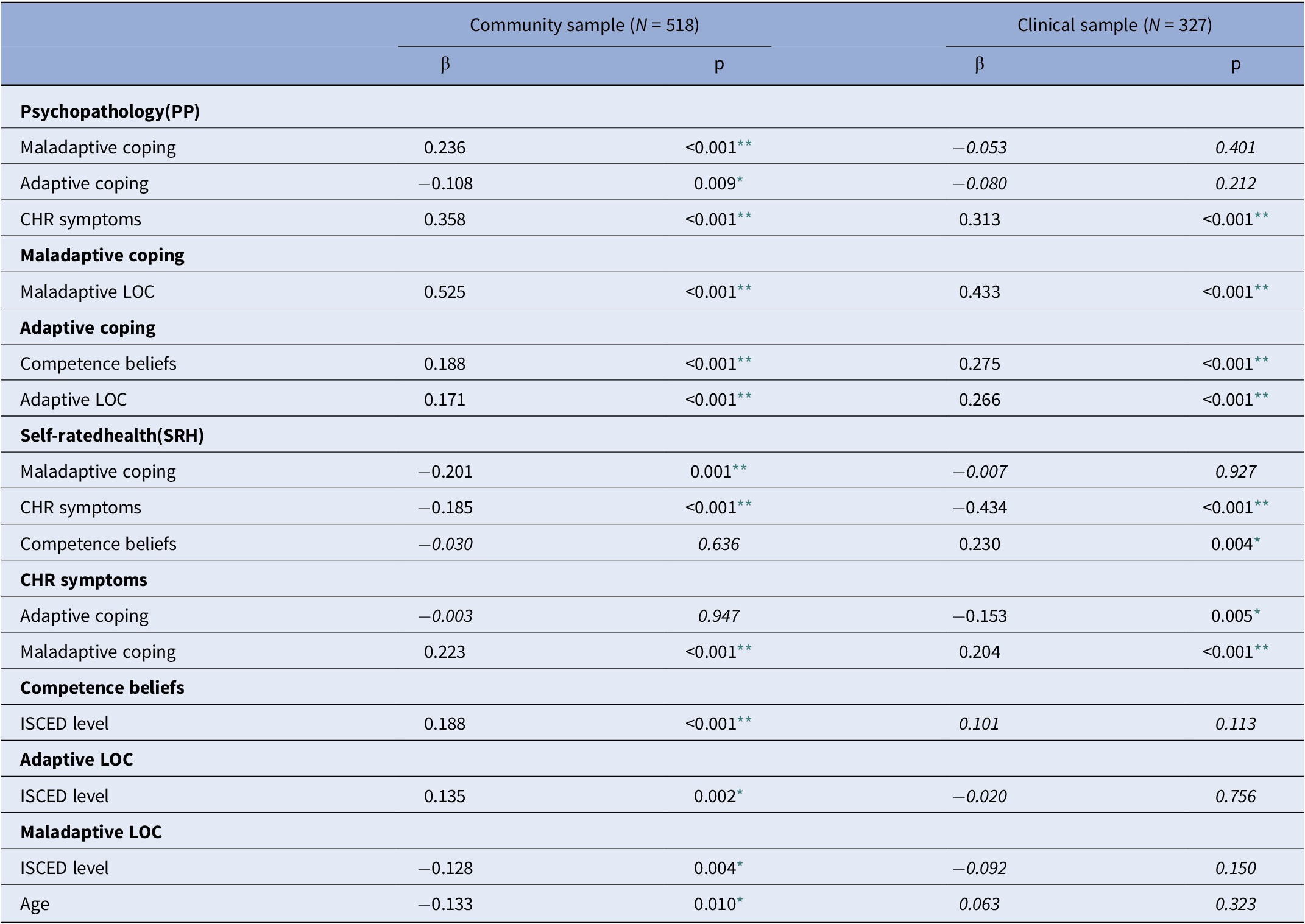
Note: italics, not significant, significant in the other sample.
** p < 0.001;
* p < 0.05.
In the community sample, maladaptive coping completely mediated the effect of maladaptive LOC on PP, SRH, and CHR symptoms (Table 3), and adaptive coping mediated the impact of competence beliefs, but not of adaptive LOC, on PP. Additionally, CHR symptoms partially mediated the effect of maladaptive coping on PP and SRH. No significant direct effects of competence beliefs and LOC on PP or SRH were detected.
Table 3. Mediation effect analyses, 95% bias-corrected bootstrap confidence intervals
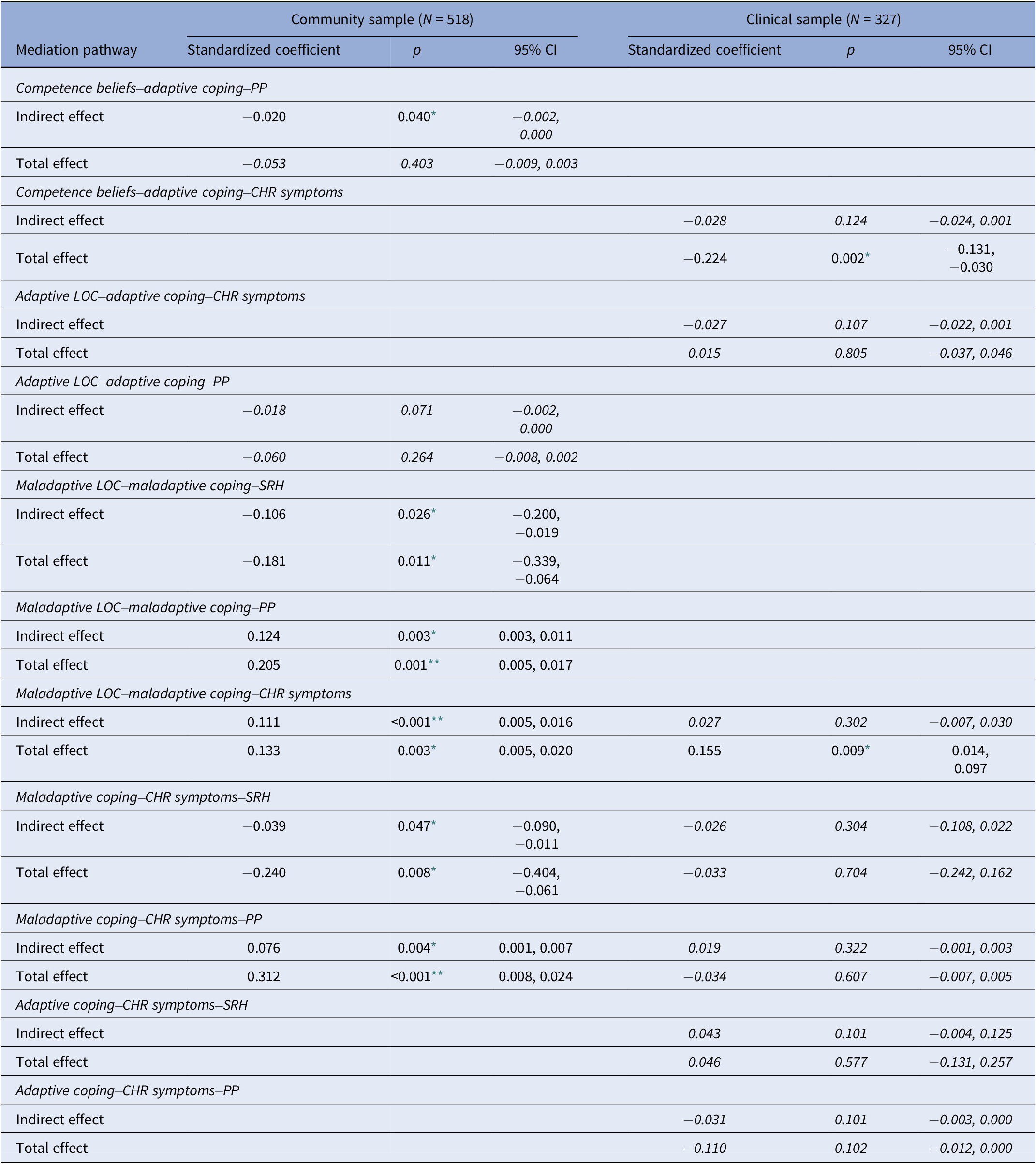
Note: italics, not significant; value missing, indirect effect was not analyzed in the corresponding sample.
** p < 0.001;
* p < 0.05.
In the sensitivity analysis, introducing sex as an exogenous variable in model 1.2 (Supplementary eFigure 8, Supplementary eTable 6) fit to the community sample data and power were excellent across all indices (CFI = 0.989, TLI = 0.982, RMSEA = 0.04, 90% CIs = 0.027, 0.045, SRMR = 0.045, power >0.999). Direct paths between the variables remained unaltered, but all mediation effects were insignificant. Competence beliefs newly showed a direct effect on PP.
3.4. SEM model 1.2 in the clinical sample
Next, we tested model 1.2 in the clinical sample (Figure 2). Compared to the community sample, model fit decreased, with CFI (0.865) and TLI (0.761) indicating poor fit, while RMSEA (0.099, 90% CIs = 0.085, 0.114) remained acceptable and SRMR (0.073) and power (0.986) excellent (Table 2, Supplementary eTable 5).
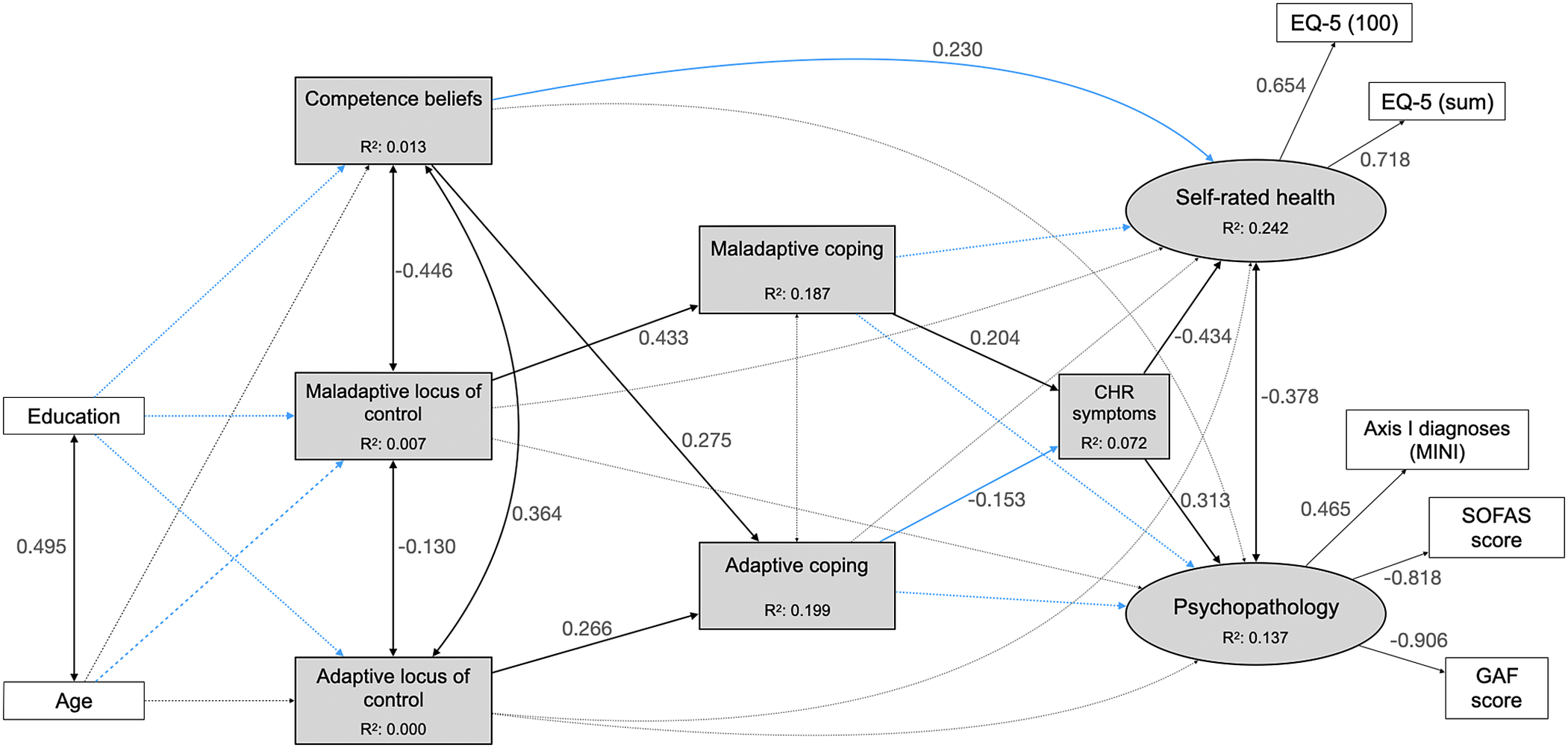
Figure 2. Model 1.2 in the clinical sample. Rectangles represent observed variables; ovals represent unobserved latent variables; black lines with double-ended arrows represent covariances; black lines with single-ended arrows represent significant paths; gray lines with double- or single-ended dashed arrows represent non-significant covariances or regression paths, respectively; numbers next to the lines indicate coefficients of significant standardized regressions and covariances, or factor loadings; the coefficients of non-significant covariances and regressions are not reported here to facilitate the figure’s interpretation; see Table 2 and Supplementary eTable 5 for further details. Blue lines indicate differences from results of testing in the community sample. CHR: clinical high risk; EQ-5 (100): score on the 0–100 analog scale of the EuroQoL-5D, three-level version (EQ-5D-3L); EQ-5 (sum): sum score on EQ-5D-3L – see Supplementary eText 5 for details; GAF, Global Assessment of Functioning; MINI, Mini-International Neuropsychiatric Interview; SOFAS, Social and Occupational Functioning Scale.
Maladaptive and adaptive coping no longer impacted SRH or PP directly, and neither adaptive nor maladaptive LOC significantly affected the MH outcome variables. Competence beliefs, however, newly directly impacted SRH, which, compared to the community sample model, was more strongly associated with CHR symptoms. Mediation analyses (Table 3), however, revealed no significant mediation by CHR symptoms in the effect of both adaptive and maladaptive coping on SRH and PP. Furthermore, no significant mediation of coping in the relationship of competence beliefs and LOC, and CHR symptoms was found.
The sensitivity analysis (Supplementary eFigure 9, Supplementary eTable 7) led to an increase in goodness of fit and power after including sex in the model. All indices except TLI (0.898) showed values ranging from good to excellent (CFI = 0.942, RMSEA = 0.068, 90% CIs = 0.053, 0.083, SRMR = 0.068, power = 0.994).
Results did not vary except for a newly significant direct effect of competence beliefs on PP and a significant covariation between adaptive and maladaptive coping (s = −0.136, p < 0.001). No mediation effect was significant.
4. Discussion
4.1. Association between core beliefs and MH outcomes
Our first hypothesis of a mediation by coping in the association between core beliefs and MH was partially supported by findings in the community sample. Aligning with the metanalytical model mostly generated on community samples [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36], maladaptive coping completely mediated the effect of maladaptive LOC on CHR symptoms, PP, and SRH, while adaptive coping only mediated the association between competence beliefs and PP. While this suggests that treating maladaptive LOC and coping may promote MH in the community, the lack of mediation effects in the sensitivity model, that is, after the inclusion of sex, calls for more research into the role of sex in these associations.
Unexpectedly, but aligning with conflicting results in the two clinical samples of the metanalytical model [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36], coping did not mediate the impact of core beliefs on MH in the clinical sample. Rather, adaptive and maladaptive beliefs were associated with their coping counterparts. Coping had direct effects on CHR symptoms, which were directly associated with MH outcomes. Newly, the total effects of maladaptive LOC and competence beliefs on CHR symptoms became significant, and competence beliefs were directly linked to SRH. A possible reason is that in clinical populations, both adaptive and maladaptive coping might specifically focus on CHR symptoms, rather than overall MH quality, as our results in the community sample suggest with lower rates of CHR symptoms. Therefore, treatment targeting coping strategies in these populations might help manage and reduce CHR symptoms, preventing maladaptive coping from acting as a trigger for CHR symptoms, exacerbating them, or worsening their outcome [Reference Jalbrzikowski, Sugar, Zinberg, Bachman, Cannon and Bearden82]. Further, in light of our findings indicating a direct effect of competence beliefs on SRH, and of competence beliefs and LOC on coping, challenging maladaptive core beliefs may also have a positive impact on MH quality. In contrast to the metanalytical model [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36], we found no direct effects of LOC on MH outcomes. Possible explanations relate to differences in our study, including added complexity of our model with three MH variables and differing conceptualizations of MH (e.g., including measures of functioning in our study).
Results indicate the need for more group-dependent research on the impact of the severity of psychopathology – and possibly type and operationalization of psychopathology – on the association and potential mediation effects of core beliefs and coping strategies with MH, as different levels of engagement with the mental healthcare system might act as an additional mediator or moderator. Such future studies will shed light on the most relevant targets for promoting MH, that is, core beliefs, coping, or both.
4.2. Role of CHR symptoms
To our knowledge, the present study was the first to explore CHR symptoms in the context of the interactions between core beliefs, coping, and MH, in both community and clinical samples. In the model selected as the best fit for the data, CHR symptoms were included as a contributor of MH outcome. However, the alternative model with CHR symptoms as an outcome of PP and SRH performed similarly well, indicating a strong association (albeit with unclear direction/placement) between MH variables and CHR in both samples, even after controlling for sex differences. Significant mediation effects of CHR symptoms in the relationship between coping and PP and SHR were found only in the community sample model disregarding sex but in no other model, possibly related to the cross-sectional nature of our study, preventing the drawing of definitive causal conclusions. Further factors that might help explain the differences between the community and clinical samples are (i) the differences in prevalence of CHR symptoms in the two samples, which may influence their role in relation to the other variables in our model as well as the results of our analyses; (ii) the impact of the additional burden of higher psychopathology and more severe functioning deficits in the clinical sample, which is generally more unwell compared to the community sample. Regardless, findings support some transdiagnostic relevance of CHR (regarding broader psychopathology and in relation to transdiagnostic factors) while simultaneously highlighting the challenge of accurately mapping CHR into broader psychopathological systems.
Aligning with earlier research on patients meeting UHR criteria [Reference Jalbrzikowski, Sugar, Zinberg, Bachman, Cannon and Bearden82, Reference Mian, Lattanzi and Tognin83], maladaptive coping was more strongly and frequently significantly associated with CHR symptoms compared to adaptive coping. Whereas adaptive coping styles were stable in UHR patients, maladaptive coping more likely changed over time and was related to corresponding changes in UHR symptoms in a UHR sample [Reference Jalbrzikowski, Sugar, Zinberg, Bachman, Cannon and Bearden82] and, in a community sample, was bidirectionally related over time to psychotic-like experiences [Reference Lin, Wigman, Nelson, Vollebergh, van Os and Baksheev84], which, however, may be a poor estimate of clinician-assessed CHR symptoms [Reference Schultze-Lutter, Renner, Paruch, Julkowski, Klosterkötter and Ruhrmann85]. With maladaptive coping also negatively impacting functioning and likely other clinical factors such as severity of symptomatology, including depression or personality traits, interventions that challenge coping strategies – and core beliefs – might be most appropriate for populations in early stages of mental disorders or with subclinical MH problems [Reference Mian, Lattanzi and Tognin83].
4.3. Strengths and limitations
The large size of both the community and clinical samples in this study and their separate analysis provide a comprehensive view of CHR symptoms and their associations with important transdiagnostic factors related to MH and some important first insights into the potential differences between community and clinical samples. Further, the assessment of MH variables in clinical interviews conducted by highly trained psychologists, and the comprehensive definition of CHR symptoms not only by UHR but also BS, adds to data validity.
The lack of control for ongoing psychotherapeutic treatment, which might have affected several variables, may be regarded as a limitation that our study shares with most comparable studies [Reference Groth, Schnyder, Kaess, Markovic, Rietschel and Moser36]. Moreover, despite growing evidence regarding their impact on CHR outcomes, especially on psychosocial functioning [Reference Strauss, Pelletier-Baldelli, Visser, Walker and Mittal86–Reference Carrión, Demmin, Auther, McLaughlin, Olsen and Lencz88], we did not include negative CHR symptoms in our models, as they were only assessed in the clinical sample and, therefore, a meaningful comparison with the community sample would not have been possible. The role of psychotherapy and negative symptoms should be explored in future research.
Additionally, for reasons of sample size and power, we opted against recommendations [Reference Buchanan89] to only impute on variables missing <5% of data but applied multiple imputation to the missing data to the SVF 120/KJ and EQ-5D-3L in the clinical sample as well, potentially constituting a statistical limitation. Furthermore, especially for the low number of participants meeting CHR criteria in the community sample (4.97%), we could not perform sensitivity analyses in CHR persons, limiting comparability with studies on CHR samples [Reference Jalbrzikowski, Sugar, Zinberg, Bachman, Cannon and Bearden82, Reference Mian, Lattanzi and Tognin83]. Lastly, as only the model with the lowest AIC – an index that penalizes models less for free parameters and favors more saturated models compared to BIC – was further processed; other possible relevant mediations, in particular PP and SRH in model 3.2 with the lowest BIC, remained unexplored.
4.4. Future directions and conclusion
Our findings support evidence of community studies of a mediation role of coping in the relationship of MH variables with core beliefs, although this role might differ between sexes and may decrease with increasing MH problems. Results in the clinical sample suggest a more complex interplay of the examined variables compared to the community sample, thus indicating the need for more group-specific analyses in future studies. Considering this and the higher severity of psychopathology and functioning deficits, treatment in this population may need to be more comprehensive and tailored to target multiple factors influencing MH outcomes, including coping strategies and core beliefs, to address the specific challenges faced by help-seeking individuals. Regarding CHR symptoms, a clear association with PP and, especially, SRH became evident in all models, with inconclusive results about their constellation. Future prospective studies should further examine the transdiagnostic factors coping and core beliefs, their relationship with CHR symptoms, and their emergence of manifest mental disorders. Overall, our results contribute to existing evidence that coping strategies, competence beliefs, and LOC represent worthwhile targets for the promotion of MH and shed further light on their complex interactions.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1192/j.eurpsy.2023.2457.
Acknowledgments
We thank our colleague Ms Madelyn Thomson (MSc) for the detailed and careful English-language editing.
Financial support
The BEAR study was supported by two project-funding grants from the Swiss National Science Foundation (SNFS) (F.S.-L., grant number 32003B_155951; F.S.-L. and B.G.S., grant number 32003B_135381).
Competing interest
Drs Kaess, Kindler, Michel, and Schultze-Lutter, Ms Rinaldi (MSc), and Mr Osman (MSc) have declared that they have no conflict of interest in relation to the subject of this study. Dr Schimmelmann has been a consultant and/or advisor to, or has received honoraria from, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, Novartis, and Shire.








Comments
No Comments have been published for this article.