EDITOR:
Cardiac surgery often involves the opening of the heart and great vessels, whereupon these structures inevitably are filled with air. Once the air gets trapped it tends to accumulate at the highest part of the heart, i.e. it is often found in the left ventricular apex, the pulmonary veins, the left atrial appendage and the upper wall of the left atrium. Today de-airing manoeuvres are part of surgical routine and include a multitude of techniques such as venting of the left ventricle and the ascending aorta, manual compression of the heart with the patient alternating between Trendelenburg and reverse-Trendelenburg position, shaking of the heart or venting the left atrium through the right pulmonary vein vent. Unfortunately, manual de-airing techniques are unable to completely and reliably eliminate all retained air [Reference Dalmas, Eker and Girard1] and it has been shown that even if the aforementioned techniques are meticulously applied, a large number of microemboli may still occur [Reference Dalmas, Eker and Girard1,Reference Tingleff, Joyce and Pettersson2]. Recently, different minimal invasive open-heart surgery techniques have been applied to correct intracardiac lesions with excellent results [Reference Cremer, Boning and Anssar3]. However, the limited surgical access in these procedures prevents manual heart massage as well as aortic venting, thus increasing the likelihood of retained intracardiac air and subsequent air embolism.
The authors report a case of retained air after minimal invasive atrial-septal-defect closure and although not new, an alternative approach of de-airing accompanied by transoesophageal echocardiography (TOE). A 20-yr-old female was referred to our institution with a haemodynamically significant secundum atrial septal defect (ASD II). Defect closure with an Amplatzer Septal Occluder (AGA Medical Corporation, Plymouth, MN, USA) had failed a few days before. Preoperative transthoracic echocardiography showed an ASD II (2.5 × 2.3 cm) with left-to-right shunting across the defect and a distinct enlargement of the right atrium and the right ventricle due to volume overload. A preoperative chest X-ray revealed a slight enlargement of the right side of heart. The patient reported a 5 to 6 month history of abnormal fatigue without signs of shortness of breath.
After induction of anaesthesia, haemodynamic monitoring was established and TOE examination was performed, confirming the aforementioned diagnosis. The surgical approach favoured at our institution is based on a modified right antero-lateral thoracotomy via a submammary mini-incision [Reference Cremer, Boning and Anssar3]. Extracorporeal circulation is then established via cannulation of a femoral artery and percutaneous cannulation of the right internal jugular vein and thereafter cannulation of the inferior vena cava. The ASD was closed during electrically induced fibrillation of the heart. Throughout the procedure meticulous care was taken to avoid air entrainment in the left atrium and in the left ventricle by leaving the left side of heart in a dependent position. Additionally, air in the left atrium was carefully evacuated by rotating the operating table and inflating the lungs immediately before the atriotomy was completely closed. However, before final defibrillation and right after the de-airing manoeuvres TOE examination revealed pooled air both in the right and in the left atrium and also in the right upper pulmonary vein (Fig. 1). Even after repeating the aforementioned routine de-airing manoeuvres, TOE displayed a distinct amount of entrapped air, especially in the right upper pulmonary vein leading to an alternative, unorthodox approach of de-airing: a 22G venting needle was inserted three times into the right upper pulmonary vein at the highest position of the left atrium while the patient was kept in a left semidecubitus position. Approximately 10 mL of residual air was evacuated and after sinus rhythm was achieved and weaning from cardio-pulmonary bypass was completed, several repeated TOE examinations did not reveal any retained air or residual shunting. Postoperatively the young patient recovered rapidly and was discharged five days after operation without any complications.
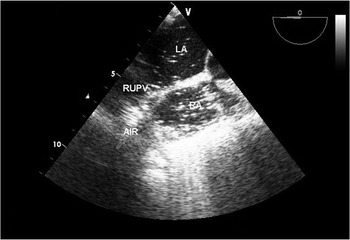
Figure 1 View of the left atrium (LA), the right atrium (RA) and the right upper pulmonary vein (RUPV) obtained from the mid-oesophageal view by slightly withdrawing and turning the probe to the right. Note the retained air in the RA, LA and the marked area in the RUPV.
During the last decade, several authors have reported on different approaches of minimal invasive closure of ASDs with excellent results [Reference Cremer, Boning and Anssar3]. However, one important problem of minimal invasive cardiac surgery is air embolism and this can occur because manual heart massage is limited and aortic root suction in cases of femoral cannulation is not possible [Reference Schneider, Onnasch and Falk4]. Pooled air is a common occurrence in open-heart surgery and is related to several neuropsychological or myocardial adverse events including cerebral ischaemia and/or neurologic dysfunction, ST segment elevation, conduction disturbances and regional wall motion abnormalities. Despite thorough surgical de-airing, microemboli continued to appear in the left atrium even up to 20 min after end of cardio-pulmonary bypass [Reference Svenarud, Persson and van der Linden5]. Although most of these events are transient [Reference Orihashi, Matsuura and Sueda6], routine use of intraoperative TOE is essential for detecting retained air, guiding the procedure to eliminate it and assessing the thoroughness of the de-airing procedure.
In the case presented, accurate and ongoing TOE examination was able to reveal pooled air even after meticulous de-airing and, moreover, TOE led to an alternative approach of de-airing, which should be kept in mind.



