Introduction
Stigma and discrimination can have a negative impact on help-seeking behaviour, treatment adherence and the recovery of people with mental disorders (Perlick et al. Reference Perlick, Rosenheck, Clarkin, Sirey, Salahi, Struening and Link2001; Barney et al. Reference Barney, Griffiths, Jorm and Christensen2006; Gulliver et al. Reference Gulliver, Griffiths and Christensen2010). For purposes of cross country and cross LIMC and HIC comparisons, the Discrimination and Stigma Scale (DISC-12) was developed as a tool to measure discrimination as experienced by people with mental disorders in four main domains: perceived unfair (negative) treatment by others because of mental illness; stopping oneself from socio-economic participation; efforts to overcome stigma; and positive treatment by others (Thornicroft et al. Reference Thornicroft, Brohan, Rose, Sartorius, Leese and Group2009; Brohan et al. Reference Brohan, Clement, Rose, Sartorius, Slade and Thornicroft2013; Koschorke et al. Reference Koschorke, Padmavati, Kumar, Cohen, Weiss, Chatterjee, Pereira, Naik, John and Dabholkar2014).
A meta-analysis of randomised controlled trials (Griffiths et al. Reference Griffiths, Carron-Arthur, Parsons and Reid2014) found educational interventions and contact (face-to-face) were effective in reducing stigma (p < 0.001) while there was no difference between face-to-face contact and internet programs. A global literature review (Thornicroft et al. Reference Thornicroft, Mehta, Clement, Evans-Lacko, Doherty, Rose, Koschorke, Shidhaye, O'Reilly and Henderson2016), concluded that social contact was the most effective type of intervention to improve stigma-related knowledge and attitudes in the short-term and also concluded that the evidence for the long-term benefit of such social contact was largely absent.
The World Health Organization (W.H.O), with a focus on LMICs has called for strategies to reduce stigma toward mental illnesses (Saxena et al. Reference Saxena, Funk and Chisholm2014) while the mhGAP-IG (W.H.O., 2010) provides practical steps for face-to-face contacts in addressing stigma. This Kenyan pilot study aimed to determine the feasibility of the WHO mhGAP-IG to reduce stigma in face-to-face contacts during interventions for specific DSM-IV/ICD 10 diagnoses over a 6-month period.
Methods
The study site
This study was conducted in Makueni County, one of the 47 counties in Kenya. It has one of the poorest economies in Kenya (Government of Makueni County, 2017). It has no psychiatrist or clinical psychologist. It has the following health facilities: one referral hospital, six sub-county hospitals, 21 health centers, 113 dispensaries and 11 private clinics (Makueni County, 2018). In consultation with the county officials, five dispensaries, nine health centers, five sub-county hospitals and the county referral hospital were selected as study sites. Clinicians (nurses and clinical officers), Community health workers (CHWs) attached to those facilities and Faith healers (FHs) or Traditional healers (THs) operating in the study catchment areas were approached and recruited by the research team. Community members, families and friends were engaged at community meetings, religious gatherings and in line at the health facilities. The engagements were interactive, with dialogue on benefits of good mental health, existing barriers and potential solutions to access mental health services and how to increase their access to mental health services.
Assessment tools
1. A researcher-designed socio- demographic and a wealth index questionnaire adopted from the World Bank International wealth index (Smits & Steendijk, Reference Smits and Steendijk2015) was administered at baseline. For the purposes of this study, we used factor scores derived from Principal Component Analysis (PCA) as the weights of items in its asset index (Vyas & Kumaranayake, Reference Vyas and Kumaranayake2006). The availability of electricity in the home, ownership of items (refrigerator, TV, bicycle, motorcycle, mobile phone, radio and motor vehicle); how food is cooked in their house (gas stove, kerosene stove, electric stove, charcoal and wood) the type of residence (tenant, own house, stay with family and other) and the wall material in their residence (mud, plastered mud, iron sheets, wood and brick/stone) were used in constructing each participant's wealth index. The wealth index is divided into 5 quintiles to reflect relative levels of economic status.
2. The MINI-Plus: This is a researcher administered instrument for DSM-IV/ICD10 diagnoses. It can be administered by a trained lay person, who reads the questions up to 3 times and records the answers. It has good psychometric properties (Sheehan et al. Reference Sheehan, Lecrubier, Sheehan, Janavs, Weiller, Keskiner, Schinka, Knapp, Sheehan and Dunbar1997) and has been validated and used in LMICs (Akena et al. Reference Akena, Joska, Obuku, Amos, Musisi and Stein2012; Nakimuli-Mpungu et al. Reference Nakimuli-Mpungu, Bass, Alexandre, Mills, Musisi, Ram, Katabira and Nachega2012; van Heyningen et al. Reference van Heyningen, Myer, Onah, Tomlinson, Field and Honikman2016) including Kenya by the same authors (Mutiso et al. Reference Mutiso, Musyimi, Tomita, Loeffen, Burns and Ndetei2017). We used it as a confirmatory diagnosis on those participants who were referred on screening positive on mhGAP-IG.
3. The Discrimination and Stigma Scale (DISC): The DISC-12 is a 34 item interview-based measure with good psychometric properties including inter-rater reliability (weighted kappa range: 0.62–0.95), internal consistency (α = 0.78) and test-retest reliability (weighted kappa range: 0.56–0.89) (Brohan et al. Reference Brohan, Clement, Rose, Sartorius, Slade and Thornicroft2013) with both quantitative and qualitative measures and has been used in LMICs (Brohan et al. Reference Brohan, Clement, Rose, Sartorius, Slade and Thornicroft2013; Koschorke et al. Reference Koschorke, Padmavati, Kumar, Cohen, Weiss, Chatterjee, Pereira, Naik, John and Dabholkar2014). The qualitative aspect asks respondents to give an example in each of the areas examined. The DISC was administered by a trained research assistant on a face-to-face basis immediately before the WHO mhGAP-IG clinical intervention and repeated 6 months later.
The instruments were adapted for Makueni County by convening a meeting of key stakeholders and individuals with relevant experience. The meeting comprised a psychiatrist, clinical psychologists, a public health physician, nurses, medical anthropologists, sociologists and residents from Makueni County who were conversant and fluent in the Kamba language. The team went through each tool, ensuring terminologies used were culturally appropriate. The mental health specialists ensured the meaning was not changed. The adaptation was through the dialogue until a consensus emerged.
Participants
Patients in the 20 study catchment areas who had been screened by trained traditional healers, faith healers, nurses, clinical officers, community health workers, family and friends; and referred to the nearest health facility where they underwent confirmatory diagnosis for DSM-IV/ICD 10 using the MINI-Plus. The MINI-Plus was administered by independent trained research assistants. Those who screened positive were approached for this study and those who gave informed consent were recruited for the confirmatory diagnosis.
The intervention
We used the WHO mhGAP-IG manual for intervention. This was done using the following steps: (i) The mhGAP-IG was adapted to fit the local context (See the appendix for details of the adaptation process). (ii) Several 1-hour community education sessions were conducted to enhance mental health knowledge and awareness in the catchment communities of the 20 facilities. These sessions were based on the adapted mhGAP-IG and covered the eight priority MNS conditions. The talks were designed to create awareness of the symptoms of the selected mental and neurological conditions, provide information on where they could get treatment for the disorders and educate on stigma and discrimination. The process was interactive with sessions on mental illnesses, specific symptomatology, causes and available treatments and prognoses. We informed them to go to their primary health care providers if they suspected they had a mental disorder based on the awareness talks. The awareness sessions were conducted by a team from Africa Mental Health Foundation (AMHF) composed of a clinical psychologist as the team leader in the field, two graduate nurses and a family physician. They all had been trained for this study by a psychiatrist (DMN) at AMHF.(iii) The adapted mhGAP-IG manual provided the framework for 5 full days of residential training for three subgroups: (1) FHs and THs, (2) CHWs and interested community members and (3) clinicians. The training was conducted by a clinical psychologist, a primary care physician and a nurse. The training covered each of the symptoms of the adult disorders from the mhGAP-IG. Teaching methods included PowerPoint presentations, case discussions combined with small group activities, mock screenings and referral processes. Providers were also trained in using the mhGAP-IG as a screening tool, going through the checklist of symptoms with patients who agreed to be screened. Patients who screened positive were referred to one of the 20 study sites. Overall, 40 clinicians, 60 CHWs, 51 FHs and 59 THs (total N = 210) were trained.(iv) Clinicians received additional training on using mhGAP-IG to offer psychosocial and biological interventions to participants who had screened positive for any of the priority mental illnesses. These illnesses are; depression, schizophrenia and other psychotic disorders, suicide, epilepsy, dementia, disorders due to use of alcohol and disorders due to use of illicit drugs. Our study only involved adults and therefore mental disorders in children were excluded. The interventions were delivered based on the mhGAP-IG manual which included pharmacological, psychological and psychosocial or both depending on the condition. Psychosocial and psychosocial interventions were interpersonal, informational activities which included psychoeducation on symptom recognition, prevention and coping strategies and stigma reduction. They also involved life skills training and better health-seeking behaviours. Pharmacological interventions involved giving the psychotropic medications. These interventions targeted biological, behavioural, cognitive, emotional and environmental factors with the aim of improving the psychological health and overall well-being. On average the mhGAP-IG prescribed intervention took between 10 and 20 minutes. Alongside treatment and care, every intervention, irrespective of the condition the participant had screened positive for, included psychoeducation and mental health advocacy. Advocacy is the use of information in deliberate and strategic ways to influence others to create change. It involves the promotion of the needs and rights of people with mental disorders, as well as that of the general population.
Data analysis
Descriptive statistics were generated for all the variables in the dataset. Paired sample t-test was used to determine whether there was a significant difference between the pre- and post-intervention on each of the four sub-scales as well as the total scores. The nature of associations between discrimination and stigma scores and the independent variables was analysed using the generalised linear mixed model. To study the adjusted associations between risk factors and discrimination/stigma scores, we developed multivariate-adjusted linear mixed models with socio-demographic characteristics as fixed effects and time as both fixed and random effect. Scores of participants who were lost to follow-ups were imputed using five randomly generated scores based on their baseline DISC scores, gender, age, marital status, level of education, employment status, wealth index and the type diagnosis at baseline. Sensitivity analysis was done using complete cases only. All the analysis were done by STATA version 14.
Results
All 2305 patients who consented to participate in the study completed the pre-intervention survey. Of these 2305 participants, 1372 completed the post-intervention survey 6 months after the intervention The follow-up rates ranged from 46.2 to 69%, with an average of 59.5%, depending on various socio-demographic characteristics and clinical diagnoses as summarised in Table 1.
Table 1. Socio-demographic characteristics of the participants
Table 2 summarises the outcomes of the items on DISC-12 and Table 3 summarises the outcomes of the DISC-12 domains while Figs 1 and 2 gives a graphic visualisation of Table 2.
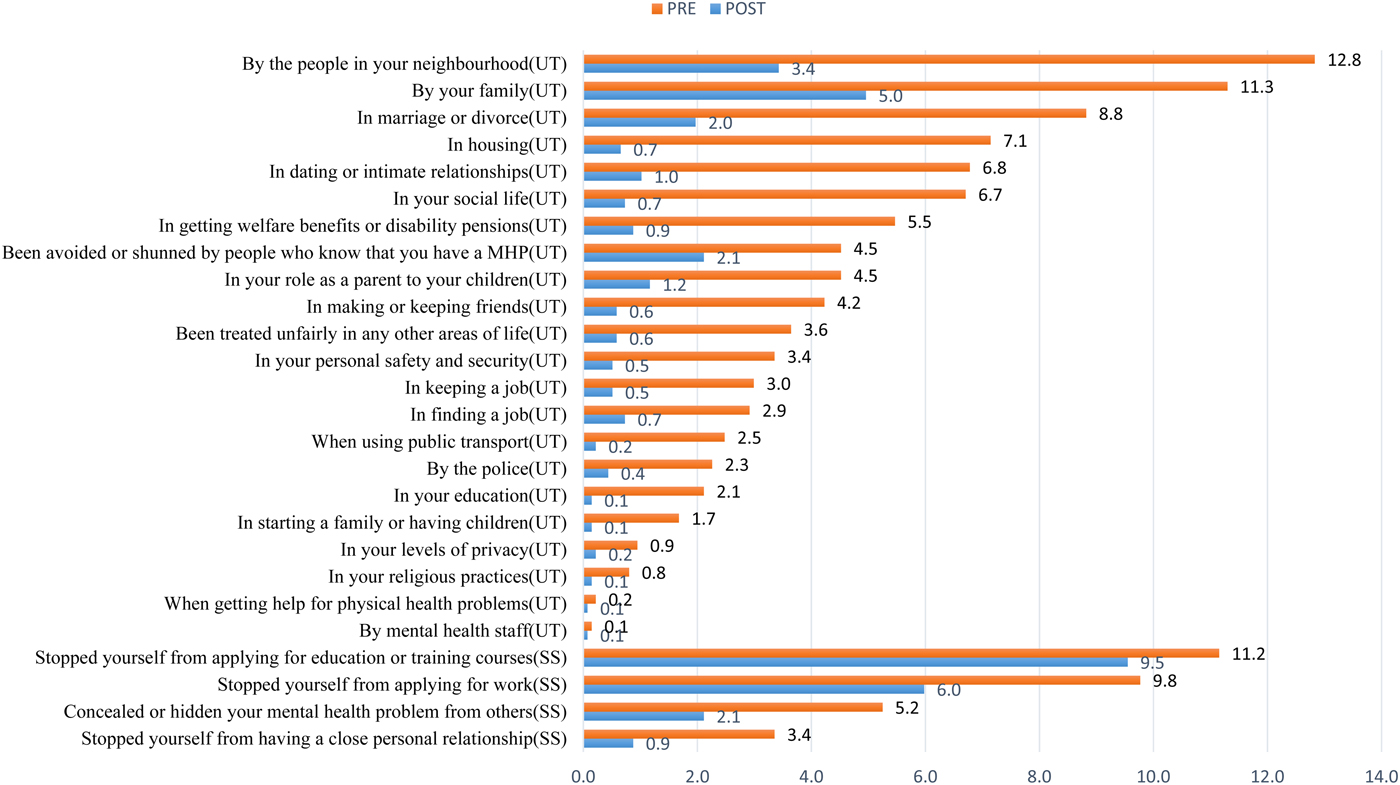
Fig. 1. Negative discrimination and stopping self-item percentages; Note-UT-unfair treatment ‘Have you ever been treated unfairly…….’; SS-stopping self ‘Have You…..’MHP-mental health problem.
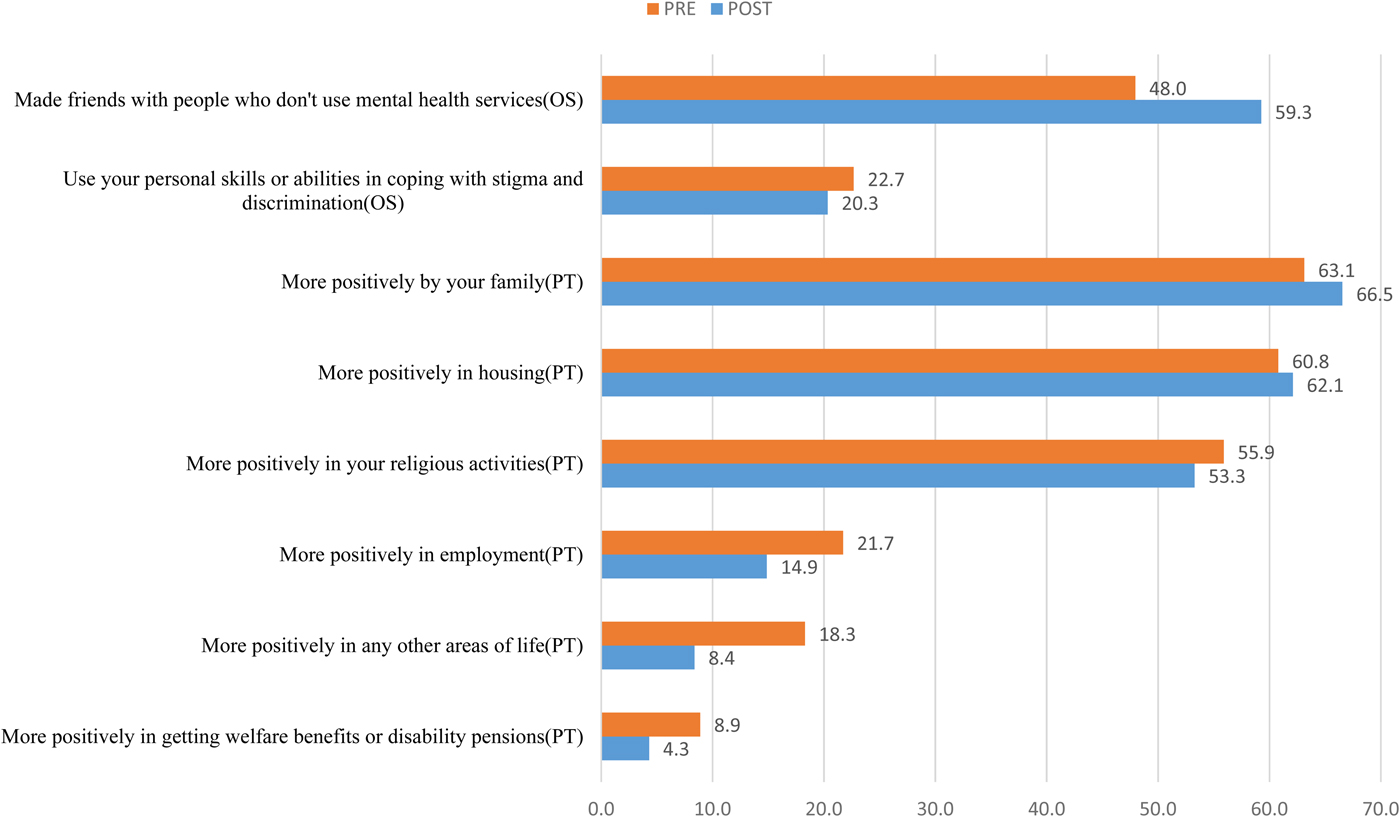
Fig. 2. Overcoming stigma (OS)‘Have you ….’and positive treatment (PT) item Percentages ‘Have you been treated……’.
Table 2. Proportion of agree responses for DISC items before and after intervention
UT, unfair treatment subscale; SS, stopping self subscale; OS, overcoming stigma subscale; PT, positive treatment; MHP, mental health problem.
***p < 0.001; **p < 0.01; p < 0.05n/snot significant.
a Complete cases, Pre and post DISC.
Table 3. Changes in DISC scores before intervention and after intervention
a Cohen's d.
b Paired samples t-test.
c DISC total count is the count of the number of items endorsed in the DISC scale or subscale.
d DISC total mean is the mean DISC scale or a subscale score.
e Sensitivity analysis for complete cases only.
In general, there was a reduction in the proportion of those participants reporting unfair treatment in all the 22 items of the domain (Table 2). The higher percentage was recorded on discrimination stemming from sources closer to the participants (e.g. by neighbours, family, housing). There was a significant reduction in unfair treatment scores after the intervention (mean difference 0.62; p < 0.001 (Table 3).
Table 4 summarises the outcomes after adjusting for other covariates. Participants who were either widowed/separated or divorced had significantly worse outcomes as compared with those who were married (p < 0.001). Those with no formal education had better outcomes as compared with those with primary education, secondary education and tertiary education; as the level of education increased, participants had worse outcomes as compared with those with no formal education (p < 0.001).
Table 4. Socio-demographic factors associated with the change in DISC domains counts after interventions
a Reference category; Est., estimate; s.e., standard error.
b Divorced/Widowed/Separated.
Those who were self-employed had better outcomes as compared with those who with formal employment and unemployed (p < 0.001). Participants aged 20 years and below had better outcomes as compared with those aged above 20 years. Participants who were grouped in the higher wealth index (quintiles 4 and 5) had better outcomes as compared with those in quintile 1. Figure 1 displays changes in individual questions on “stopping self” domain before and after the intervention. Overall there was a reduction in all the items after the intervention. With regard to score, there was a significant decrease in stopping self-scores after intervention (Table 3; mean difference 0.08, p < 0.001). Controlling for other variables, females had better outcomes as compared with males. Those who were married had better outcomes as compared with those who were single. Participants who were unemployed had worse outcomes as compared with those who were self-employed. Participants who were aged 20 years and below had better outcomes as compared with those aged 21 years and above. Those in the lowest wealth index quintile had better outcomes as compared with those in quintile 3. Participants diagnosed with major depression had better outcomes as compared with those diagnosed with epilepsy, psychosis, mania/hypomania, alcohol abuse and suicidality. No significant differences were found between depression and dementia, substance abuse and co-morbid disorders.
Figure 2 displays changes in individual questions on ‘overcoming discrimination’ domain before and after the intervention. Overall there was a significant increase in overcoming stigma scores after the intervention (Table 3; mean difference = 0.17; p < 0.001). Males had better outcomes as compared with females. Those with a primary level of education and higher had better outcomes than those with no formal education. Those who were employed had better outcomes as compared with those who were self-employed. Those who had wealth index of quintile 3 and above had better outcomes than those with wealth index of quintile 1. There were no significant differences between wealth index quintiles 1 and 2. The participants who were diagnosed with hypomania/mania, psychosis and epilepsy had better outcomes as compared with those diagnosed with the major depressive disorder, however, those diagnosed with substance abuse and dementia had worse outcomes as compared with those diagnosed with the major depressive disorder.
The changes in positive treatment items before and after intervention are shown in Fig. 2. There was an increase in the proportion of the participants who reported to have been treated more positively by their family members from 63.1 to 66.5% and more positively in housing from 60.8 to 62.1%; however, there was a reduction in the proportion of participants reporting being treated more positively in religious activities, employment, other areas of life and in getting welfare benefits or disability pensions after the intervention. Overall, there was a significant decrease in positive treatment scores after the intervention (Table 3; mean difference = 0.11; p < 0.001).
Participants who were diagnosed with major depression had better outcomes in negative discrimination domain (unfair treatment) as compared with those diagnosed with suicide, psychosis and a comorbid disorder. They also had better outcomes in the stopping-self domain as compared with those diagnosed with epilepsy, psychosis, mania/hypomania, alcohol abuse and suicide. However, the participants who were diagnosed with mania/hypomania, psychosis, and epilepsy had better outcomes in the overcoming stigma domain as compared with those diagnosed with the major depressive disorder. In contrast, those diagnosed with substance abuse and cognitive defects had overall worse outcomes as compared with those diagnosed with the major depressive disorder in the overcoming stigma domain. Even though there was a significant reduction in the positive treatment domain, participants who were diagnosed with alcohol abuse, substance abuse, cognitive defects and comorbid disorders had better outcomes as compared with those diagnosed with depression. However, those diagnosed with epilepsy and psychosis had worse outcomes as compared with those diagnosed with depression.
Discussion
Socio-demographics
The age structure found in this study does not reflect the pyramid structure typical of Kenyan demographics (Kenya National Bureau of Statistics, 2010). This study included adults aged 18 and above and therefore the very low percentage for age group 20 and below. Those 60 and above constituted a third of the respondents. We speculate that this age group took the highest interest in our study because they would be relatively available post-retirement. It is not surprising therefore that dementia/cognitive deficits were the second single common diagnosis after the depression.
Follow-up rates
We have plausible explanations based on our clinical experiences and past research findings for the observed follow-up rates. In one of our studies (Mendenhall et al. Reference Mendenhall, Kohrt, Norris, Ndetei and Prabhakaran2017), we have demonstrated that for different people ‘recovery’ is defined by several contextual and individual considerations. If the symptoms reduce to a level where they are not a priority compared with other life priorities such as pursuing economic activities to earn a living, saving the money used to travel to hospital, attend to other social activities or go for treatment concurrent physical illness etc., then they will consider themselves adequately recovered to pursue other more pressing life priorities (Mendenhall et al. Reference Mendenhall, Kohrt, Norris, Ndetei and Prabhakaran2017). This could partly explain the observed follow-up rates for different socio-demographic variables and diagnoses.
By and large, this study supports previous studies that found that contact (here defined as face to face) based interventions are effective. The effect size of the intervention ranged from 0.18 to 0.46 which is comparable with previous literature reviews (Corrigan et al. Reference Corrigan, Morris, Michaels, Rafacz and Rüsch2012; Griffiths et al. Reference Griffiths, Carron-Arthur, Parsons and Reid2014; Thornicroft et al. Reference Thornicroft, Mehta, Clement, Evans-Lacko, Doherty, Rose, Koschorke, Shidhaye, O'Reilly and Henderson2016); the effect sizes of stigma reduction programs involving contact are between small to medium (0.29 and 0.47) (Cohen, Reference Cohen1988) which is similar to what we found in our study.
The risk and protective factors
We speculate several dynamics in the overall change across the several domains of the DISC-12. Post-intervention the participants perceived less barrier between themselves and other people with no mental disorders; a positive reciprocal response from other people who saw improvement in them and therefore a gain in self-esteem; a better understanding of mental illness as biological conditions like any other conditions and less of cultural stigmatising explanations for their mental illness; and appreciation of their human rights like any other person; the clinical improvements about their conditions which enhanced their self-esteem. However, there were some unique responses that can be explained. Positive increase rather than decrease was reported in item 28 (p < 0.001); and decrease rather increase was reported in items 30, 32, 33 & 34 29 (p < 0.01). We speculate this was a reciprocal reaction of people who noticed a change in these people since the participants in this study were also receiving the clinical intervention. It is noteworthy that items 15, 16, 24 and 31 were not associated with significant change (p > 0.05) between pre and post-test. We speculate that because these items did not involve a close emotional relationship with the stigmatised people and therefore stigma was felt less at a personal level.
When comparing changes in the sub-domains before after intervention, unfair treatment was particularly decreased, demonstrated by greater mean changes and effect size. This may indicate that negative discrimination/experiences of negative reactions play a major role in discrimination and stigma among people with mental illness in our study population.
Out of the 22 items of the unfair treatment domain the items with the greatest change was being treated unfairly in their neighbourhood, in marriage or divorce, in housing, by your family, in social life, in dating or intimate relationship and in getting welfare benefits or disability pensions. This suggests that stigma was most felt if it was associated with people who would otherwise be considered emotionally close and expected to play a greater role in being least discriminating and most accommodating.
Our findings across the four DISC-12 domains suggest overall significant improvement except in one: total mean for DISC stopping self. This is in agreement with what has been found in other studies that did not use mhGAP-IG (Corrigan et al. Reference Corrigan, Morris, Michaels, Rafacz and Rüsch2012; Griffiths et al. Reference Griffiths, Carron-Arthur, Parsons and Reid2014; Thornicroft et al. Reference Thornicroft, Mehta, Clement, Evans-Lacko, Doherty, Rose, Koschorke, Shidhaye, O'Reilly and Henderson2016). The reduction in unfair treatment scores after the intervention was strongly associated with marital status. Those who were married had better outcomes as compared with those who are either divorced/separated or widowed confirming what was mentioned earlier that ongoing close relationships were critical to stigma reduction. Those with higher education experienced a lesser degree of decrease at post-test probably because they had a better understanding of mental illness (as described above) even before the interventions. Given that those with higher education had less scores at pre-test, these participants had less room to improve their scores at post-test.
We attribute our finding that older adults had better outcomes as compared with younger adults to better reporting, which is in agreement with other studies (Ali et al. Reference Ali, King, Strydom and Hassiotis2016). However, it is important to note that older patients may demonstrate other needs or risk factors for stigma and discrimination that may lessen the efficacy of psychosocial interventions (Rejeski & Mihalko, Reference Rejeski and Mihalko2001).
In our findings, we found out that participants with a higher wealth index had more improvement in anticipated stigma and discrimination compared with those with a wealth index. This is consistent with other studies (Perese, Reference Perese2007). We speculate it is a reflection of better resources for coping with stigma.
On anticipated discrimination, our findings agree with another study (Ali et al. Reference Ali, King, Strydom and Hassiotis2016) that gender modified the relationship between severity of Intellectual Disability (ID) and self-reported stigma in that male participants who had moderate ID were more likely to report stigma compared with females with moderate ID. This might explain why females were more likely to have higher improvements on the scores on ‘stopping self’ domain as compared with males. In addition, females display a greater response to psychotherapy than males, similar to what was found by Thornicroft et al. Reference Thornicroft, Mehta, Clement, Evans-Lacko, Doherty, Rose, Koschorke, Shidhaye, O'Reilly and Henderson2016). The reduction in stopping self-scores after the intervention was strongly associated with marital status with those who were married having better outcomes as compared with those who are single. We have already discussed the plausible explanation on the role of marital status.
The reduction in ‘overcoming discrimination’ was associated with employment status. Participants who are self-employed had more improvement in ‘stopping self’ scores compared with those that are unemployed. This may be partially explained by the fact that they have more resources than those unemployed. It can also be argued that being self-employed demonstrates possession of skills and that they can also apply in confronting stigma.
Being young was also associated with more improvement in ‘stopping self’ scores as explained above from the literature that older adults are likely to report more stigmatising experiences (Ali et al. Reference Ali, King, Strydom and Hassiotis2016). In addition, older people may have other needs or risk factors for stigma and discrimination that may lessen the efficacy of psychosocial interventions (Rejeski & Mihalko, Reference Rejeski and Mihalko2001), which are part of mhGAP-IG. We have already demonstrated in the Kenyan setting young people demonstrated a significant reduction in stigma post-intervention (Ndetei et al. Reference Ndetei, Mutiso, Maraj, Anderson, Musyimi and McKenzie2016).
On ‘overcoming discrimination’, just like ‘stopping self’, being female, being married, being employed and being young was associated with better outcomes, however those with low wealth index had better outcomes as compared with those with higher wealth index.
The pattern of the different diagnoses reflect the clinical epidemiology of the cases identified for screening using mhGAP-IG, subsequently confirmed using the MINI-Plus. Overall, depression had better outcomes than all other conditions in all the domains except in treatment domain and for reasons explained below. It is not surprising that participants who were diagnosed with mania, psychosis, and epilepsy had better outcomes on the treatment domain as compared with those diagnosed with major depressive disorder since, unlike depression, the management of these conditions was symptom-oriented and best managed with psychotropics which have a faster effect than psychosocial intervention. Substance abuse and dementia which tend to take a chronic course with less indications for psychotropics and requiring much longer psychosocial intervention had worse outcomes compared with depression.
On the domain of ‘unfair treatment’, participants who were diagnosed with major depression had better outcomes as compared with those diagnosed with epilepsy, psychosis, mania/hypomania, alcohol abuse and suicide, for the same reasons already discussed above under the domain on unfair treatment. This is similar to the findings of Griffiths et al. (Griffiths et al. Reference Griffiths, Carron-Arthur, Parsons and Reid2014) who found a better outcome for depression than for schizophrenia and overwhelming cultural stigma towards suicide and the complexity of treating more than one condition.
Limitations
(i) There were no control groups and therefore we cannot precisely tell whether the observed differences before and after intervention were due to mhGAP-IG interventions or other factors that affect the outcome. To mitigate this, we adjusted for all the measurable factors in the generalised linear mixed models during analysis. We recommend future studies with comparison groups. (ii) The participating centres were purposively sampled to suit the priorities of the County Government while at the same time representing all the levels of health care in the County. In mitigation, this was essentially a pilot study on the feasibility of WHO mhGAP-Intervention Guide in reducing experienced discrimination in mental disorders in a rural Kenyan setting.
Conclusion
The mhGAP-IG may be an effective tool for reduction of discrimination in clinical situations presided over by trained but supervised and supported clinicians in LIMCs. The 6-month's period between pre and post-tests is long enough to avoid recency (Oberauer, Reference Oberauer2003; Morrison et al. Reference Morrison, Conway and Chein2014). However, we would recommend longer follow up in future studies to determine the longest possible time the outcomes would be sustained and what factors are at play. Outcomes are moderated by socio-demographic and economic characteristics, type of mental disorder, particular domains of stigma and emotional relationships especially within family members and possibly friends and workmates. To the best of our knowledge, this is the first study to report the use of mhGAP-IG to reduce discrimination in people living with mental disorders.
Data sharing
The data for this study will be made available upon written request to the corresponding author detailing the specific parts of the data to be shared and the intended purpose.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796018000264
Ethical standards
Ethical approval for this study was obtained from Maseno University Ethics Review Committee (MU-ERC).
Acknowledgements
The Government of Makueni County for providing the necessary logistics for successful implementation of the study.
Financial support
This work was supported by Grand Challenges Canada (GCC), Grant #0739-05
Conflict of interest
None.








