Background
In January 2020, a primary and middle school in Berlin reported a cluster of 12 cases of scarlet fever and illness absenteeism amongst pupils of 32% (58/184) to the local health authority. Scarlet fever is a bacterial disease, caused by toxigenic group A streptococcus, and spreads through droplets or direct contact. It is readily treated by antibiotics, although untreated can cause serious long-term sequelae [Reference Rodriguez-Iturbe, Haas, Ferretti, Stevens and Fischetti1]. Concerns about the uncontrolled spread of scarlet fever were raised and an outbreak investigation was initiated. Here, we aim to describe the outbreak investigation and lessons learnt, with a focus on case ascertainment and risk communication.
Case definitions
We defined a probable case as a clinical diagnosis of scarlet fever according to the German national guidelines [2], in a pupil or school staff member or their close contacts, after 1 January 2020. A confirmed case was defined as a probable case with a group A streptococcus detected on a throat swab or other biological sample [2]. A close contact was defined as any individual who has been in a shared environment, within a distance of 2 m for a duration of at least 15 min.
Notification system for scarlet fever in Germany
Mandatory reporting of scarlet fever by local health authorities (LHA) to the German infectious disease surveillance system is not required. However, schools, nurseries or hospitals are obliged to report potential infectious disease clusters, including scarlet fever, to LHAs, which can initiate outbreak investigations and disease control measures [2]. Schools rely on parents to inform them of any illnesses among their students.
Description of the outbreak
Epidemiology of the outbreak
At the time of the outbreak investigation, the school had reported 18 cases of scarlet fever between 6 January 2020 and 13 February 2020 (Fig. 1). Due to the German infectious disease notification system, the outbreak response team did not have direct access to the medical records of cases. Therefore, the outbreak team attempted to contact parents of all notified cases via telephone interviews using a standardised questionnaire to assess reported symptoms and gain more information on the transmission, potential origin of infection and perception of the illness. During the telephone interviews one additional probable case was identified, a sibling of a recently notified pupil, who had not yet been reported to the school administration. Therefore, we considered 19 cases, of which parents of 16 (84%, 16/19) could be reached after a maximum of three attempts. Verbal consent was provided by the parents for the telephone interviews and institutional review board approval was not necessary as the LHA has the authority to investigate disease outbreaks.

Fig. 1. Epidemiological curve. Number of scarlet fever cases notified by the school by date of symptom onset, Berlin, 2020.
Table 1 describes the characteristics of the total study population (i.e. students notified as having scarlet fever by the school and contacted) and the study population stratified by having scarlet fever according to the German national guidelines following an in-depth interview (i.e. being a probable case). These 16 notified cases had a mean age of 9 years (range: 6–15) and 5 (31%) were female. All visited a physician and 13 (81%) parents reported that the physician diagnosed their child as having scarlet fever. However, only seven (7/16, 44%) met the probable case definition, as they reported fever and at least one typical clinical symptom, of which five (5/16, 31%) met the confirmed case definition, as they also reported the presence of group A streptococcus using a rapid diagnostic test.
Table 1. Characteristics of the study population and probable cases and non-cases, scarlet fever outbreak, Berlin, 2020
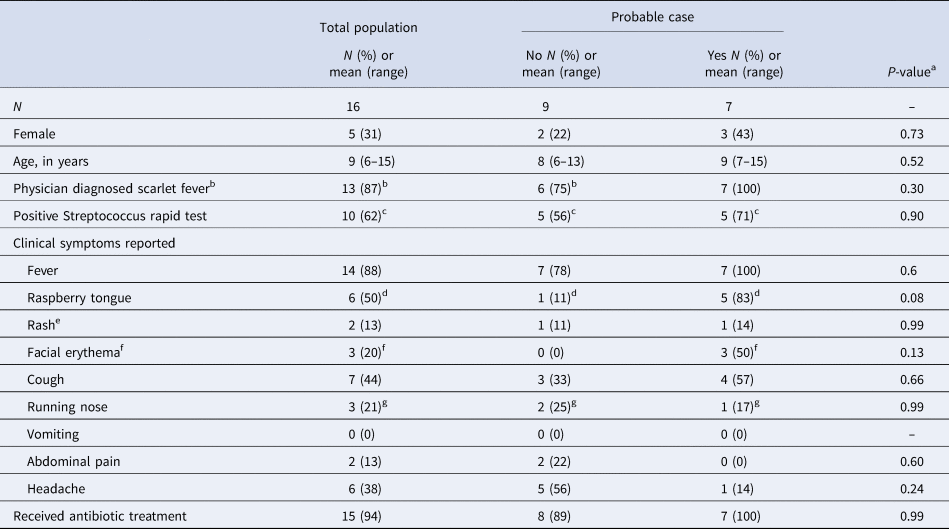
Probable cases were defined according to the German national guidelines for the clinical diagnosis of scarlet fever, which is fever and at least one other typical symptom of scarlet fever (i.e. either raspberry tongue or facial erythema or rash) [2].
a Differences between probable and non-probable cases were assessed using Fisher's exact test or the Wilcoxon rank-sum test, as appropriate.
b Other diagnoses included tonsillitis (n = 1), flu (n = 1) and one who did not recall.
c Of the probable cases, one tested negative and one tested inconclusive. Of the non-probable cases, three parents did not recall the test result and one was not tested as the differential diagnosis was deemed to be flu.
d Among probable cases, one parent did not recall and among non-probable cases, three parents did not recall.
e Defined as redness and/or sandpaper feeling of trunk and/or limb skin.
f Defined as red cheeks with the pale area around the mouth. One missing among probable cases.
g Among probable cases, one parent did not recall and among non-cases one parent did not respond.
Non-cases were more likely to have symptoms consistent with the common cold and, as a result of the case definition, facial erythema and raspberry tongue were more common among probable cases. However, due to the small sample size, there were no statistically significant differences in reported clinical symptoms between probable cases and non-cases (P-value > 0.05, Fisher's exact test or Wilcoxon rank-sum test, as appropriate). Interestingly, having a raspberry tongue, a relatively unique and typical clinical scarlet fever symptom, was not commonly recalled; 25% of parents (4/16) did not know if this occurred.
We did not discern any clear clustering of cases in the school; of the seven probable cases two groups of two cases were in the same class and three cases were each in different classes, spread across the primary and middle school. There was no direct relation between cases other than being in the same school or class, except for the two siblings, who were in different classes.
Communication and control measures taken by the school
The school communicated with the parents during the outbreak (Fig. 2). Parents of all pupils were informed of the cluster of cases. Children with illness were asked to stay at home, consult a physician and not to return to school unless scarlet fever was excluded or treated.

Fig. 2. Timeline of actions by the school, scarlet fever outbreak, Berlin, 2020.
Parents' attitudes and beliefs
Fifteen parents answered questions on their perception of the illness their child experienced. Of these, four (4/15, 27%) stated that they had only consulted a doctor because the school had asked parents to seek medical care for any sick child. All four parents, of which three were parents of the probable case, explained that their child's disease was mild, no more severe than a common infection of the upper airways.
Overall, the majority of parents (>60%) did not perceive the illness to be severe. None reported it as very severe, only four (4/15, 27%) as severe, five (5/15, 30%) as intermediate, five (5/15, 30%) as mild and one (1/15, 7%) as very mild.
Similarly, when parents were asked how concerned they were with the outbreak in the school, only one (1/11, 9%) was very concerned (four of the 15 refused to answer this question). The rest of the parents were moderately concerned (1/11, 9%), a little concerned (3/11, 27%) or not concerned (6/11, 55%).
Physicians' perception
To better comprehend how paediatricians viewed scarlet fever, we contacted five paediatricians in the catchment area of the school. All paediatricians confirmed that the differentiation of scarlet fever from streptococcal tonsillitis or other feverish diseases is based on clinical symptoms and rarely poses a diagnostic challenge. Three out of five physicians experienced difficulties in making parents understand the difference between tonsillitis and a systemic disease, such as scarlet fever.
Discussion and conclusion
Scarlet fever, formerly a leading cause of death in children until the beginning of the 20th century [Reference Katz and Morens3], has re-emerged in the last decade in several countries, including Germany and the United Kingdom [Reference Lamagni4–Reference Liu6]. Here, the reported outbreak appeared potentially large early on, with possible unreported cases among those children who had not come to school due to illness. The outbreak investigations concluded that the outbreak was far smaller than reported. We found seven probable cases, of which five were considered confirmed cases. Therefore, we did not pursue further case finding activities and recommended that the school continue with infection prevention and control efforts.
We believe the current notification system played an important role in this outbreak. Neither the school responsible for the outbreak notification nor the LHA responsible for the outbreak investigation had access to medical records. The LHA was not able to contact the treating physicians directly for confirmation of diagnosis, as they did not know who the treating physician was. Thus, the initial reporting by the school solely relied on the medical situation as understood by the pupils' parents. As our investigation revealed, there was a considerable difference between the number of scarlet fever cases as (1) reported by the parents, who reported 13 cases, (2) notified by the school to the local public health authority, which notified 18 cases, and (3) defined by the outbreak investigation team based on the clinical presentation reported by the parents during interviews, which concluded there were seven probable cases.
Factors that could facilitate the misclassification of scarlet fever cases pertain to the diagnosis of scarlet fever. Scarlet fever is characterised by clinical symptoms of systemic inflammation. In contrast, streptococcal tonsillitis, caused by non-toxin-mediated Streptococcus pyogenes, leads to a local infection of the upper respiratory tract and mostly presents with only mild systemic inflammation [Reference Tewfik and Al Garni7]. As both diseases share some similarities, including a common pathogen and some common symptoms, it might be difficult for lay people to understand the difference between the two diseases. Second, the available point of care testing (POCT) revealing the presence of streptococcal antigen shows a positive result for both illnesses. However, available POCTs do not show the specific feature of toxin-production, differentiating scarlet fever from non-toxigenic infections [Reference Hübner and Jansson8]. Third, antibiotic treatment for the two diseases is the same [Reference Spencer9, 10]. Indeed physicians corroborated that these factors all played a role when diagnosing scarlet fever cases. They stated that there were communication issues; parents commonly misinterpret the streptococcus rapid test as a test for scarlet fever and felt that parents had difficulty distinguishing between streptococcus tonsillitis and scarlet fever.
It is always possible that there were more probable scarlet fever cases, as it can present in an atypical form [Reference Phillips, Martin-Bates and Withnall11]. However, this does not preclude the potential bias in the transmission of information, as evidenced when communicating information from physicians to parents to schools to LHA.
Justifiably, the school administration was highly concerned initially about a large scarlet fever outbreak and had initiated several infection prevention and control measures, prior to the outbreak investigation. The school responded strongly in the communications to the parents and LHA, and in the measures, it was considering, i.e. temporary school closure. It is impossible to ascertain whether the school measures would have prevented a larger outbreak but given that the outbreak was smaller than initially reported, some of the measures might not have been necessary.
In this outbreak investigation, we reaffirmed the importance of case definitions and ascertainment when investigating an outbreak. Moreover, we emphasise the importance of communication; regarding the reporting of scarlet fever and the communication of the school's measures from the school to the parents. The system of notifying scarlet fever cases, from physicians, to parents, to the school administration, and the local health authority, could be improved to avoid reporting of spurious cases. An evaluation of the current system, in which schools notify suspected clusters of cases to LHAs in Germany, would be useful to identify areas of improvement. This will also aid schools and LHAs in determining the appropriate response and communication strategy.
In a time of crisis, accurate and timely information is among the most valuable commodities. Improvements in these will help better tackle future outbreaks in school settings.
Acknowledgements
We would like to thank the school administration and parents for their cooperation with the outbreak investigation.
Authors' contributions
NM and NJS investigated the outbreak. They communicated with the school, parents, conducted data collection and data analysis. They wrote the first draft and revised the manuscript. LM and JW supervised the outbreak investigation and were involved in the manuscript revision. All authors reviewed and approved the final version.
Declaration of interest
None.
Data availability
Data are available from the corresponding author upon reasonable request and in accordance with German data protection law.






