INTRODUCTION
Percutaneous injuries (PIs) resulting from skin breaks by needles or sharp objects contaminated with blood or body fluids represent serious occupational hazards to healthcare workers (HCWs) [Reference Adams1, Reference Shiao2]. Over 20 blood-borne pathogens have been documented to be transmitted following PIs, most commonly hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV) [Reference Adams1].
The World Health Organization has estimated that more than 3000000 HCWs may experience some degree of stress as a result of PIs with potentially contaminated sharp objects annually [Reference Prüss-Ustün, Rapiti and Hutin3, 4]. Several reports have noted that a large proportion of PIs (39–75%) go unreported [Reference Ghofranipour5, Reference Wicker6]; the corresponding rate in an earlier study in Taiwan was 79–82% [Reference Shiao7, Reference Shiao8]. Such rates may pose a serious risk of exposure to blood-borne pathogens for HCWs.
Taiwan is a high endemic area for HBV and HCV [9]. A large-scale community screening study in 2005 reported that the hepatitis B surface antigen (HbsAg)-positive prevalence rate was 17·3%, and estimated the total number of HBV carriers in the population aged >20 years to be approaching three million [Reference Chen10]. In addition, ~4% of the general public were seropositive for HCV [Reference Chen10]. HIV transmission has become an alarming threat in Taiwan, evidenced by the 29 475 seropositive patients and 12 593 acquired immunodeficiency syndrome (AIDS) cases reported through the surveillance system for HIV infection since its activation in 1984 [11].
The overall prevalence rate in hospital inpatients for blood-borne infectious diseases such as HBV and HCV has been shown to be higher than in the general public [Reference Shiao, Guo and McLaws12, Reference Wicker13]. It therefore follows as a consequence of the high population prevalence of blood-borne viruses such as HBV and HCV in Taiwan that HCWs in this country may be facing higher seroconversion occupational risks stemming from PIs compared to such workers in other developed countries [Reference Shiao2, Reference Chen10]. From the beginning of 2011, the Taiwan Ministry of Labour mandated that public hospitals and medical centres (tertiary referral hospitals) report their PIs to the Chinese Exposure Prevention Information Network (EPINet). As this mandatory policy led to an increased number of hospitals being required to report to the system, it was expected that a better safety climate in healthcare settings had been created since the implementation of the new regulation.
The first study to estimate the national incidence of PIs with the purpose of identifying the real risk of contaminated PIs for full-time HCWs in Taiwan [Reference Shiao2] used the reported PI data from 14 hospitals to the Chinese EPINet in 2004. Three denominators were used, the number of full-time HCWs, number of hospital beds, and number of inpatient days. These denominators were judged to be directly related to patient care activities and the national incidences estimated by using these denominators were also close to one another, reflecting that these estimates reliably estimated the chance of encountering PIs for HCWs.
As the earlier study was based on voluntary reports from participating hospitals [Reference Shiao2] it was considered to be of interest to determine the national incidence of PIs in HCWs in the period following the initiation of mandatory reporting in Taiwan using the same denominators as above to estimate the number of device-specific incidents, mechanisms of injuries and potential exposure to contaminated sharps used for patients with HBV, HCV or HIV
METHODS
The study was designed using a retrospective secondary data analysis approach to analyse 2011 data from the Chinese EPINet. Ethical issues of the study were approved by the institutional review board of the National Taiwan University Hospital (201403027W). There were 507 hospitals with accreditation from the Department of Health in Taiwan in 2011, of which 249 participated in reporting PIs to the Chinese EPINet but only 81 hospitals had actively reported cases since 2004. The following criteria were used to shortlist these 81 medical institutions for the research study sample: (1) those in January 2011 which had already joined the Chinese EPINet for at least 3 months, and (2) those which had reported PI surveillance data throughout 2011. Moreover, in order to perform trend analysis with the earlier results of Shiao et al. [Reference Shiao2], we excluded cases reported by psychiatric hospitals and non-hospital clinics, nursing homes, and blood centres. In addition, since the numbers of HCWs from each hospital and from the nationwide data were not adjusted for part-time or casual medical staff, only full-time staff were included in the final analysis.
Measurements
The EPINet, established by the University of Virginia, has been recognized as an efficient surveillance programme for occupational exposures to blood pathogens through PIs [Reference Jagger14, Reference Jagger, Bently and Juillet15]. It also provides comprehensive and detailed information on needles and sharps injury events and possible exposures to pathogens and aids the prevention of such incidents; it is used in over 80 countries to date to report incidents [16, Reference Jagger and Perry17]. The Chinese version of the EPINet surveillance software was translated and launched in 2004 in Taiwan. In addition, real-time reporting measures were first introduced in Taiwan, making it the world's first country to use the Internet to report needlestick and infection exposure events. The data used in this study were gathered from the Chinese version of EPINet through which the hospitals in Taiwan report their PIs.
Data analysis
Data from the Chinese EPINet (1 January 2011 to 31 December 2011) were imported into Microsoft Excel, and analysed using the JMP 5·0 statistical package [18]. The average incidence and 95% confidence intervals (CIs) of annual PIs from each participating hospital was calculated, based on the number of hospital beds, full-time HCWs, and days of inpatient care. In Taiwan, the number of beds reflects the size of the hospital and not necessarily the actual number of patients cared for due to various bed occupancy rates in each hospital. The number of inpatient days indicates the actual patients cared for by HCWs. The national number of PIs was estimated by multiplying mean incidence by nationwide numbers of hospital beds, full-time HCWs, and total inpatient days [reimbursed payment by the National Health Insurance Administration (NHIA), which reflects the actual figure of the nation's annual hospitalization days]. The annual mean PI incidence/10000 inpatient days for each of the 49 participating hospitals was multiplied by the nationwide number of inpatient days (per 10000) in 2011 published by the NHIA to give an estimated national incidence rate with 95% CIs. Regression analysis was used to test the relationship between three denominators and the number of PIs reported. The same measure was used to estimate the number of PIs for each job category, contaminated sharps encountered, and exposure to blood-borne viruses, by total inpatient days in Taiwan.
RESULTS
A total of 49 hospitals met the inclusion criteria for the study and eight of these were classed as tertiary hospitals, the others being approximately equally divided between primary and secondary establishments (Table 1). The number of PI incidents was highest in tertiary (65.1%) and lowest in primary (6·4%) centres and this distribution mirrored the numbers of beds and full-time HCWs. In total, the analysis covered 665492 monthly inpatient days, 1837 reported PIs, and 44939 full-time HCWs (Table 1).
Table 1. Hospital type, numbers of PIs, beds, full-time HCWs, and average inpatient days in 49 study hospitals in 2011
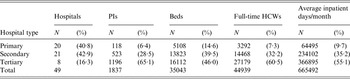
PIs, Percutaneous injuries; HCWs, healthcare workers.
There was a similarly high proportion of PIs in the study hospitals when analysed/10000 beds (418·1) or 10000 full-time HCWs (393·6) compared to the low rate/10000 outpatient days (Table 2). When these data were extrapolated to all hospitals in Taiwan the corresponding projected annual numbers of injuries analysed by hospital beds, full-time HCWs and inpatient days, were 6710 [standard error (s.e.) = 593], 8319 (s.e. = 762), and 7828 (s.e. = 1290), respectively (Table 2). Regression analysis showed that the number of PIs was highly correlated with full-time HCWs (R 2 = 0·79, P < 0·001), inpatient-days (R 2 = 0·74, P < 0·001), and number of beds (R 2 = 0·69, P < 0·001).
Table 2. Number of PIs in the 49 participating hospitals and the estimated total number of PIs in Taiwan in 2011

PIs, Percutaneous injuries; CI, confidence intervals; HCWs, healthcare workers.
* Number of hospital beds, full-time HCWs, and inpatient days were obtained from the National Health Insurance Administration Annual Report of Taiwan.
Table 3 shows that the highest incidence of PIs in the study hospitals was found in physicians (654/9236, 7·1%), followed by registered nurses (1019/23416, 4·4%). However, this order was reversed for the projected annual number of PIs/10000 inpatient days with the highest rate for registered nurses (5690, 95% CI 3207–8176), followed by physicians (1476, 95% CI 921–2030).
Table 3. Number of PIs in the HCWs of the 49 participating hospitals and the estimated total number of PIs by inpatient days in Taiwan in 2011

PIs, Percutaneous injuries; HCWs, healthcare workers; CI, confidence intervals.
* Estimation is based on a total of 30805680 inpatient days/year.
† 0·03–0·22.
On an annual basis, the estimated numbers were twice as high for injuries due to hollow-bore needles (5915, 95% CI 3419–8441) compared to sharps injuries (2787, 95% CI 1874–3670) (Table 4). The leading cause of PIs was disposable syringes (620, 33·8%), and these accounted for 50·8% of hollow-bore needles. Intravenous (IV) catheters (108, 5·9%), needles on IV lines (54, 2·9%), hypodermic needles (46, 2·5%), and vacuum tube blood collection needles (39, 2·1%) were the next most common devices identified. Of the solid sharp devices, suture needles were the most common type (259, 14·0%), followed by lancets (98, 5·3%) and disposable scalpels (47, 2·6%) (Table 4). Both physicians and nursing staff showed significant differences between device associated injuries (χ 2 = 369·8, P < 0·001). The top three devices associated with injuries for physicians were disposable syringes (202/654, 30·9%), suture needles (185/654, 28·3%), and disposable scalpels (30/654, 4·6%); those for nurses were disposable syringes (325/1019, 31·9%), IV catheter (91/1019, 9·0%), and lancets (87/1019, 8·5%).
Table 4. Device-specific injuries by inpatient days and estimated total annual number of injuries in Taiwan in 2011
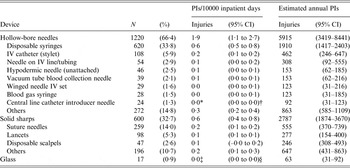
PIs, Percutaneous injuries; CI, confidence intervals; IV, intravenous.
* 0·03.
† 0·01–0·04.
‡ 0·02.
§ 0.01–0·03.
Table 5 outlines the various mechanisms reported by which PIs occurred. The most common were ‘between steps of a multi-step procedure’ (425, 23·1%) followed by ‘during use of an item’ (281, 15·3%), and ‘after use, before disposal’ (206, 11·2%). A similar number of incidents occurred when ‘disassembling device or equipment’ (176, 9·6%), or ‘recapping’ (170, 9·3%) with ‘placing sharps into collectors' (100, 5·4%) being the least common. There was a significant difference between physician and nursing staff (χ 2 = 231·1, P < 0·001) with ‘between steps of a multi-step procedure’ and ‘during use of an item’ accounting for around 60% of reported PIs by physicians. For nurses, the most common situation was also ‘between steps of a multi-step procedure’, with most other mechanisms contributing to similar numbers of incidents (Table 5).
Table 5. Top six mechanisms of PIs reported to the Chinese EPINet in Taiwan in 2011
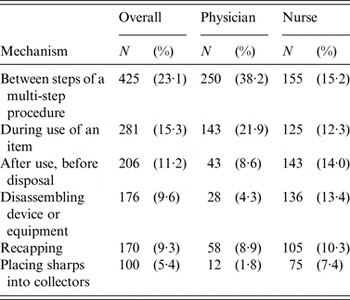
PIs, Percutaneous injuries; EPINet, Exposure Prevention Information Network.
About 13·0% of the source patients were seropositive for HBsAg and HBeAg was identified in 0·7% of the patients. Antibodies to HCV were detected in 13·8% of patients, and 1·1% were HIV positive. From national data based on 30805680 inpatient days/year, it is estimated that for full-time HCWs 970 would be exposed to HBV, 1094 to HCV, and 99 to HIV annually (Table 6).
Table 6. Numbers of HCW contacts with contaminated sharps from patients with HBV, HCV, and HIV by inpatient days and the estimated annual PIs in Taiwan in 2011
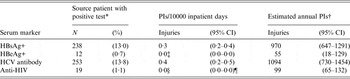
PIs, Percutaneous injuries; CI, confidence intervals; HBsAg, hepatitis B surface antigen; HBeAg, hepatitis B e antigen; HCV, hepatitis C virus;HIV, human immunodeficiency virus.
* If the source patient could not be identified, the average positive rate was used to estimate the positive serology.
† Estimation is based on a total of 30805680 inpatient days/year.
‡ 0·02.
§ 0·03.
¶ 0·02–0·04.
DISCUSSION
Based on reporting data from the study hospitals in 2011, the projected annual number of PIs in Taiwan hospitals ranged from 6710 to 8319 which corresponds quite closely (8058–8286) with our earlier study in 2004 [Reference Shiao2]. Regression analysis indicated that the three denominators used in both the earlier [Reference Shiao2] and the present study all had good predictive value for PIs. However, the ‘total number of full-time HCWs' and the ‘total inpatient days' serve as better predictors than the ‘total number of hospital beds', possibly because the former two represent the actual medical services used and the manpower required to provide such services, while the latter does not. These results indicate that the selected predictors are appropriate irrespective of the sample size and the time period covered.
The finding that PIs were most associated with physicians is consistent with the report of Gańczak et al. [Reference Gańczak19]. Compared with the study using the 2004 EPINet data [Reference Shiao2], it is striking that the estimated national number of PIs in physicians increased from 594 in 2004 to 1476 in 2011, whereas the number declined in the other HCW categories. By contrast, several other studies have found that physicians tend to have the lowest reported PI rate [Reference Shiao7, Reference Shiao8, Reference Wicker13, Reference Beltagy20, Reference Winchester21]. Since 2011, the Chinese EPINet has been the reporting system nominated by Taiwan's Ministry of Labour through which medical centres (tertiary hospitals) and public hospitals are mandated to report PI cases. It is possible that this mandatory reporting requirement has raised the awareness of, and attention to, PIs in medical centres, where there are more resident doctors than in smaller hospitals, thereby increasing the physician reporting rate.
It is widely accepted that implementation of safety devices and adequate training of staff will lead to a reduction of PIs [Reference Hoffmann, Buchholz and Schnitzler22]. In terms of device-specific injuries, ‘disposable syringes' remain the main mechanism of injury for both physicians and nurses but the next most common device for physicians was ‘suture needles' and ‘IV catheters' for nurses. We suggest that in the future, in addition to the use of hollow needles, safety suture needles should be considered to further reduce the incidence of PIs.
In the 2004 study [Reference Shiao2], where ‘recapping’ was the leading cause of PIs, accounting for 16·5% of the PIs, the present study found that recapping had fallen to the fifth most common cause, or 9·3% of incidents. A possible explanation could be the increased use of sharps collection containers and safety needles [Reference Hoffmann, Buchholz and Schnitzler22, Reference Yao23] and improved needle safety education and training [Reference Beltagy20, 23, Reference Balkhy24]. As to why ‘between steps of a multi-step procedure’ such as between the injection process and equipment delivery, became the most common PI mechanism, we consider this may be related to Taiwan's National Health Insurance payment system. After the implementation of the Diagnosis Related Groups (DRGs) payment system in 2010 in Taiwan, the average length of inpatient days has consequently shortened [Reference Cheng, Chen and Tsai25, Reference Wilburn26]. In addition, the clinical condition of the average patient is generally more critical now, requiring more medical procedures and interventions [Reference Yang27].
Although HBV and HCV are a more significant threat to staff through PIs, compared to the 2004 study the number of seropositive patients has slightly decreased while HIV cases have largely increased in recent years. The need to pay attention to increasing occupational exposure to HIV in Taiwan's HCWs is even more apparent and urgent from this study compared to the 2004 data [Reference Shiao2], given that the estimated number of HCWs with PIs from needles used by HIV-positive patients has grown 1·7-fold, from 59 cases in 2004 to 99 cases in 2011. Although the prevalence of HIV-positive patients is considered to be low in Taiwan, the actual cumulative number of HIV-positive cases nationwide increased from 6762 in December 2004 to 22 020 in 2011 [11], indicative of a rapidly rising threat of HIV seroconversion for HCWs. We suggest that all HCWs should be retrained on the importance of the use of personal protective equipment to mitigate HIV infection risks.
The previous study results on the incidence of PIs [Reference Shiao2] in HCWs were presented to the Taiwan Occupational Safety and Health Agency (OSHA) and legislators, and served to increase safety awareness of PIs. Subsequently in 2011 the Taiwan OSHA mandated all public and tertiary hospitals to report their PIs to the Chinese EPINet which led to an increase in reported incidents. Moreover, as PI data are consolidated and integrated into a single system, it has enabled us to have a better understanding of the mechanisms contributing to risk of injury in HCWs and to formulate and strengthen detection and preventative interventions to reduce such risks in the future.
A variety of factors contribute to risk of PIs, such as the types of devices used, procedures undertaken, insufficient provision of sharps containers, inappropriate training on the use and disposal of needles and sharps, and inadequate knowledge of the potential consequences of such injuries [Reference Prüss-Ustün, Rapiti and Hutin3]. A hierarchy of control for reducing hazards should begin with the elimination of unnecessary sharps and injections combined with engineering solutions to prevent operator errors. In addition, administrative controls (e.g. policies, procedures), work-practice alterations that result in safer behaviours (e.g. not recapping) and correct use of personal protective equipment can prevent exposure [Reference Wilburn26]. These measures as well as decreasing the use of invasive procedures, promoting the use of safer devices and procedures, managing exposures, and on-the-job education of risks and personal protection should be reinforced and audited to ensure compliance [Reference Prüss-Ustün, Rapiti and Hutin3].
Although accounting for only 9·7% of the total number of hospitals in Taiwan in 2011, the 49 study hospitals contributed 21·8% of the total number of hospital beds, 21·3% of the total number of HCWs, and over a quarter (25·9%) of the total number of inpatient days nationally. As all public and tertiary hospitals are now required to report their PIs to the Chinese EPINet under the Taiwan Ministry of Labour's mandatory policy, it should lead to a growing awareness of needle safety and an increased willingness to report such injuries. This study may also reflect the outcome of PI prevention education programmes over time [Reference Phillips28]. Nevertheless, the interpreted results presented here cannot be generalized to all hospitals in Taiwan, especially to small-sized hospitals and clinics, which tend to have less patient-related needle and sharps usage but also tend not to report their PIs due to lack of resources or awareness. An additional limitation of the study is that part-time employed HCWs were not included in the analysis and it is possible that their practices may impact to a greater or lesser degree on the incidence of PIs in their hospitals.
In conclusion, our data indicate that ‘between steps' of a multistep procedure was the most common mechanism contributing to PIs in the study population. In contrast to our earlier survey the practice of ‘recapping’ has become a less frequent mechanism for PIs as a result of the increased use of safety devices and improved education and training. About 13% of the source patients in the study were seropositive for HBV or HCV and thus pose a significant risk to health practitioners. Moreover, although HIV seroconversion was relatively low at 1·1% in source patients the cumulative national HIV incidence data suggest that HCWs in Taiwan are now facing an increasing threat from HIV infection. Finally, the Taiwan Safety Needle Act requires that all HCWs must be provided with safety needles by 2017. This study therefore serves as a comparison base representative of the period prior to the implementation of the Act and going forward, it will be necessary to determine the impact of the Act on occupational health in HCWs.
ACKNOWLEDGEMENTS
The project was founded by the Taiwan Institute of Occupational Safety and Health (IOSH).
DECLARATION OF INTEREST
None.









