Introduction
Middle East respiratory syndrome coronavirus (MERS-CoV) is an international public health challenge with considerable differences in methods of reporting death-related within and between countries [Reference Feikin1–Reference Kim, Tandi, Choi, Moon and Kim7]. The case fatality rate accounted for 30–63% in Saudi Arabia [Reference Feikin1–Reference Mohd, Memish, Alfaraj, McClish, Altuwaijri, Alanazi, Aloqiel, Alenzi, Bafaqeeh, Mohamed and Aldosari4] and 20–63% in the Republic of Korea [Reference Mizumoto, Saitoh, Chowell, Miyamatsu and Nishiura5–Reference Kim, Tandi, Choi, Moon and Kim7].
Recently, several epidemiological investigations have been published that assessed the factors associated with mortality in MERS patients [Reference Almekhlafi, Albarrak, Mandourah, Hassan, Alwan, Abudayah, Altayyar, Mustafa, Aldaghestani, Alghamedi and Talag8–Reference Rivers, Majumder and Lofgren13]. However, the findings of most of these studies either represent a specific population group such as intensive care unit [Reference Almekhlafi, Albarrak, Mandourah, Hassan, Alwan, Abudayah, Altayyar, Mustafa, Aldaghestani, Alghamedi and Talag8], a single medical centre [Reference Saad, Omrani, Baig, Bahloul, Elzein, Matin, Selim, Al Mutairi, Al Nakhli, Al Aidaroos and Al Sherbeeni9] or outbreak infection in the Republic of Korea [Reference Mizumoto, Endo, Chowell, Miyamatsu, Saitoh and Nishiura10, Reference Majumder, Kluberg, Mekaru and Brownstein11].
One study analysed publicly available data through the Saudi Ministry of Health webpage to identify the factors associated with mortality in Saudi Arabian patients [Reference Banik, Alqahtani, Booy and Rashid12]. One limitation of this study was lack of multivariate risk modelling. Rivers et al. [Reference Rivers, Majumder and Lofgren13] used a multivariate Poisson regression model to identify factors associated with a high incidence of mortality, but their study excluded all cases (186) from the Republic of Korea. A recent study by Chen et al. compared the risk factors and disease characteristics in South Korean and Saudi Arabian populations, but did not assess the survival rate in these cases [Reference Chen, Chughtai, Dyda and MacIntyre14].
The authors of all previously published studies of MERS-CoV were not able to assess survival rate in MERS cases from various countries that were reported to the World Health Organization (WHO). Although the mentioned studies provided valuable information in terms of mortality risk in MERS patients, a common limitation was noted in these previous studies: no global data were used, such as the associations between different geographical regions and mortality. The findings in these reports were made using data on specific populations or regions. Per the author's knowledge, at this time there is no large cross-country comparison study of MERS-CoV-related mortality, and it is not yet clear whether the mortality rate of MERS-CoV can be identified by countries and regions.
It is important to understand and compare MERS-CoV patients according to their clinical outcomes between multi-countries. Such a study may provide a useful multi-country work to reduce the mortality in the MERS-CoV population worldwide. The current study may provide multivariate risk models to identify patients at high risk of death in order to manage MERS-CoV patient clinical outcomes. This may improve public health plans by establishing effective programmes to prevent serious outcomes. These programmes can be addressed by the healthcare system or public health policies.
The goal of this study was to estimate and compare the variations in the risk-standardised mortality rates by regions and by patients’ characteristics among different countries across the world, specifically comparing regions that had the largest number of MERS-CoV cases. The author hypothesised that people of older age, with underlying medical conditions and from Saudi Arabia or other Middle East countries are at high risk of death related to MERS-CoV.
Methods
The study utilised a publicly available MERS-CoV database of case reports retrieved from the WHO: http://www.who.int/csr/don/archive/disease/coronavirus_infections/en/. The WHO receives situational reports of confirmed MERS-CoV cases from all countries across the globe. The WHO provides a routine update through its website on new cases, deaths and current developments. Prior to 26 January 2017, all reports were presented in a narrative format, describing case by case the disease characteristics of each patient. The author and research assistant accessed each of these narrative reports, and converted the patient information and disease characteristics into a line listing for analysis. Beginning with the reporting period of 2–7 January, WHO enhanced their reporting practices, including an excel document with patient and disease characteristic data which can be easily analysed.
The latest line listing update of MERS cases was on April 2017 in a report from Qatar. Globally, the WHO report on 4 April 2017 indicated that the overall case fatality rate was 35.6% (690 deaths of 1936 cumulative laboratory-confirmed MERS cases) in 27 countries (WHO, 2017). The author did not include all MERS cases reported to the WHO because the early reports of MERS used unstandardised case presentation that lacked important details. This study included MERS cases reported to the WHO between 5 January 2015 and 10 March 2017. Another reason for choosing this period to study is that in 2015, the WHO started reporting cases by the country where the confirmed case has occurred. The author performed quality control checks to detect invalid or missing data. The author excluded some cases from the Republic of Korea that were reported between 12 June and 21 July 2015, as no patient case report was used. They reported a summary of the updated cases (total cases and deaths) instead of case-by-case details. Case #3 reported on 23 March 2016 has been excluded from Saudi Arabia due to the wrong date of symptom onset stated in his case report.
The total cases included in the analysis were 883. The author obtained information on age, gender, date of notification, date of onset of MERS symptoms, date of outcome or death, whether a patient or healthcare worker, symptomatic, underlying medical conditions, source of infection and the reported country. In order to assess the impact of older age on mortality among MERS patients, patient age was classified into four groups: age <30, 30–59, 60–65 and >65 years. The data retrieved were from 14 countries. The author classified countries into three regions according to the geographical location and the number of cases: (1) Saudi Arabia 766 (86.7%), (2) Middle East, but excluding Saudi Arabia 44 (5%), and (3) Republic of Korea or other countries 73 (8.3%). The Republic of Korea 65 (7.4) and other countries 8 (0.9%) were combined due to the small number of cases in the latter group. Saudi Arabia was analysed separately from the Middle East countries because Saudi Arabia has a unique situation and recorded the largest number of MERS cases.
Outcomes
Two primary end points were assessed: 14- and 45-day mortality related to MERS – after developing symptoms. The study author estimated the survival rates using the time of symptom onset to outcome. MERS-CoV has an incubation period of 2–14 days, by which time symptoms usually occur. Survival rates at the 14-day mark are medically significant as they demonstrate survival at the point at which patients most typically experience symptoms. The 45-day mark was selected to demonstrate the progression of the disease for an advanced period. There were 83 patients with no symptoms; the author used date of laboratory confirmation instead of date of symptom onset for these patients. Survival rates can be interpreted by the portion of MERS patients who were still alive at 14 and 45 days after they experienced symptoms.
Statistical analysis
Statistical analyses were performed with SAS version 9.4 software. Data from 883 MERS-CoV patients who reported to the WHO between 5 January 2015 and 10 March 2017 were retrieved and analysed. Descriptive statistics were used to describe the study population (Table 1). Unadjusted Cox proportional hazards models (CPHMs) were used to estimate hazard risk (HR) and a 95% confidence interval (95% CI) for 14- and 45-day mortality (Tables 2 and 3). Multivariable CPHMs were used to estimate adjusted hazard risk (aHR) and 95% CI for 14- and 45-day mortality adjusting for gender, age, region, whether healthcare worker, having comorbidity, being asymptomatic and the source of infection (Tables 2 and 3). The log-rank tests were used to compare survival curves for demographic and disease characteristics (Figs 1–4). The 14- and 45-day survival rates were estimated using the Kaplan–Meier estimator.
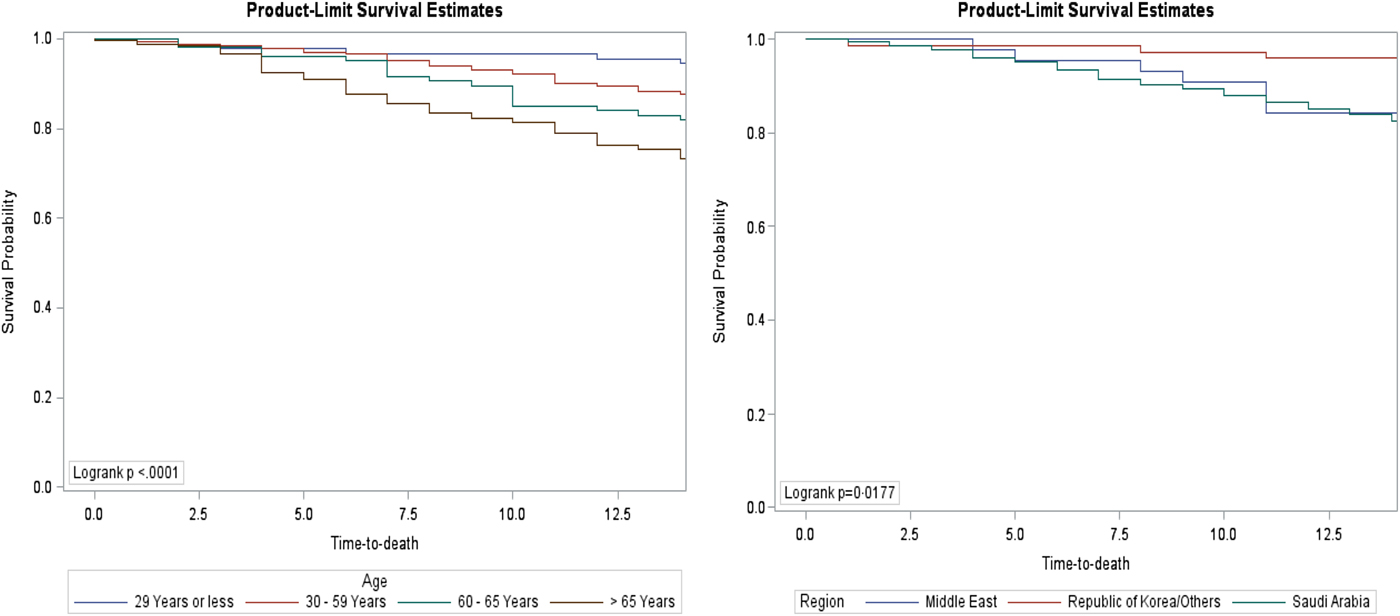
Fig. 1. Fourteen-day survival rate of confirmed MERS cases by age groups and regions.
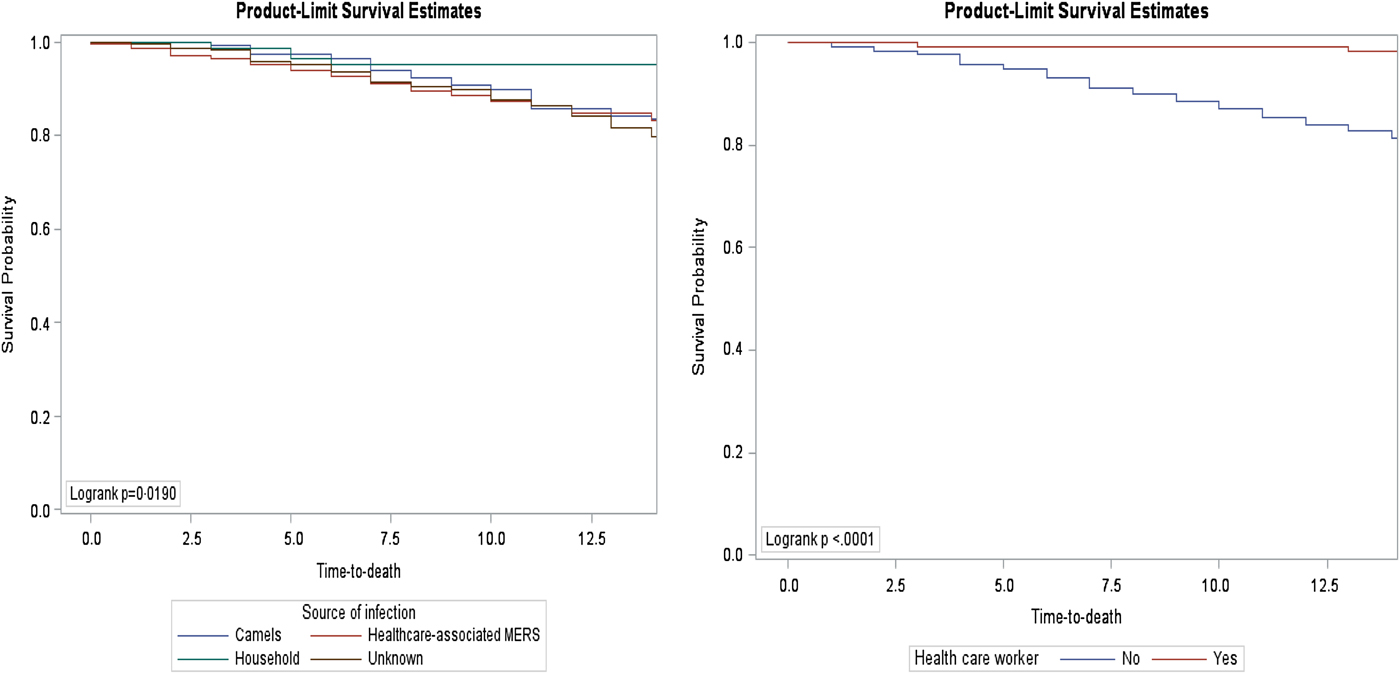
Fig. 2. Fourteen-day survival rate of confirmed MERS cases by source of infection and healthcare worker.
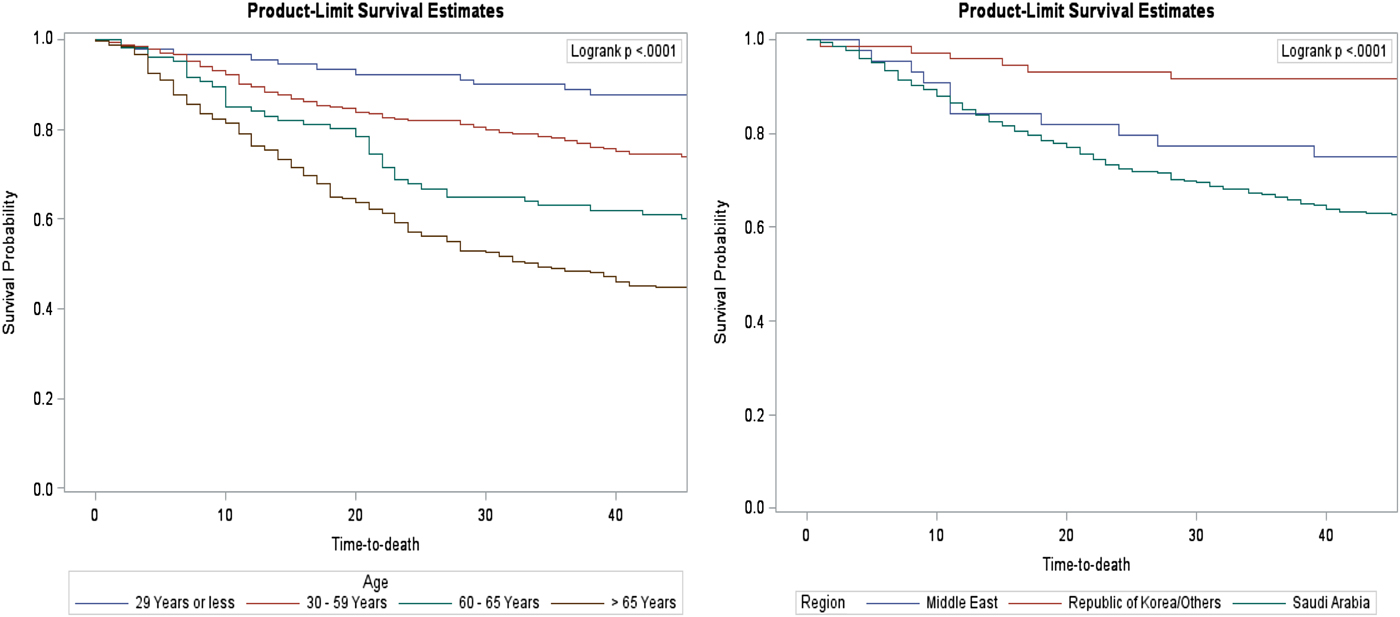
Fig. 3. Forty-five-day survival rate of confirmed MERS cases by age groups and regions.
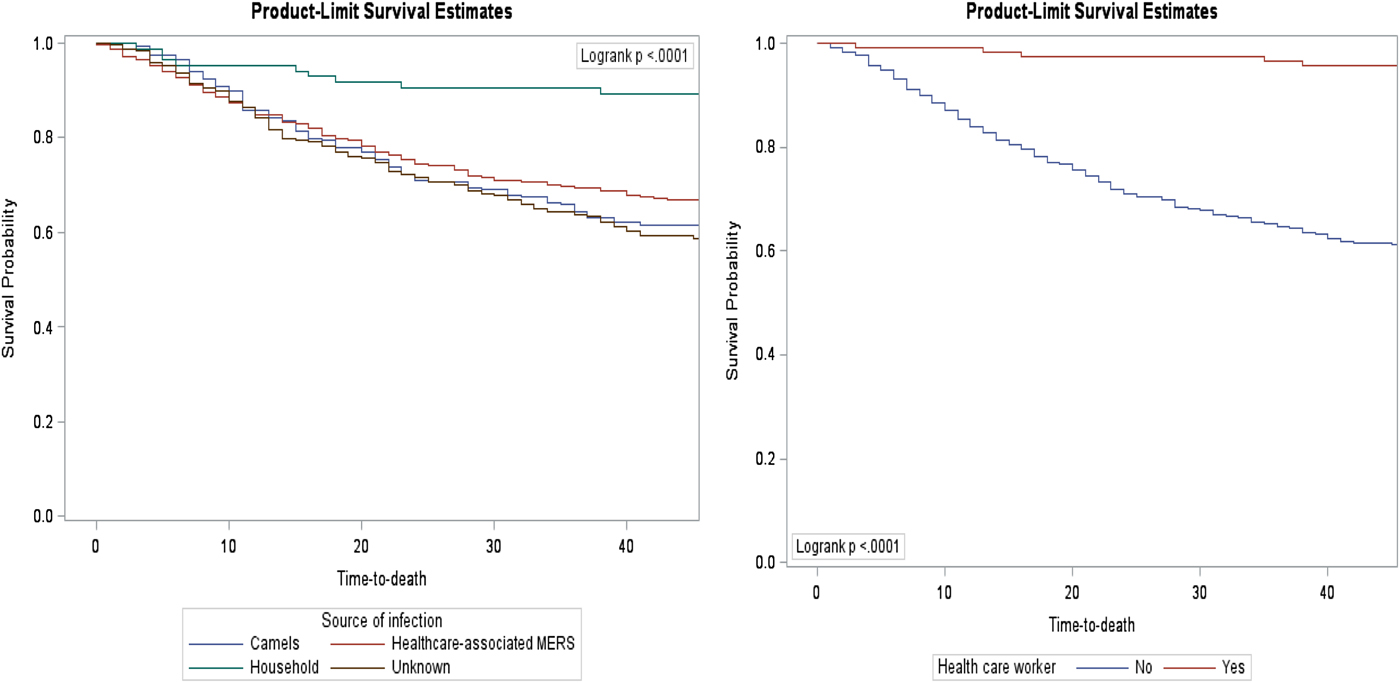
Fig. 4. Forty-five-day survival rate of confirmed MERS cases by source of infection and healthcare worker.
Table 1. Sample characteristics of 883 MERS patients

Table 2. Factors associated with 14-day mortality in MERS patients
*Significant at α = 0.05; HR, unadjusted hazard ratios; aHR, adjusted hazard ratios.
Table 3. Factors associated with 45-day mortality in MERS patients
*Significant at α = 0.05; HR, unadjusted hazard ratios; aHR, adjusted hazard ratios.
Results
A total of 883 patients with confirmed MERS-CoV infection were included in the analysis. The characteristics of the population can be found in Table 1. The population was relatively older with a mean age of 54.3 (±s.d. 17.6 years) with an age range between 2 and 109 years. MERS-CoV symptoms were present in 799 (90.4%), and 226 (72.6%) had a comorbidity. Healthcare-associated MERS-CoV infection was the greatest source of infection 368 (41.7%), then unknown source of infection 235 (26.6%) and camels 195 (22.1%). Most of the cases were reported from Saudi Arabia 766 (86.7%). The overall mortality rate in MERS-CoV patients included in this study was 323 of 883 (36.6%), the 14-day mortality rate was 144 of 883 (16.3%) and the 45-day mortality rate was 301 of 883 (34.1%).
Table 2 illustrates unadjusted and adjusted 14-day hazard risks for all-cause mortality. The unadjusted 14-day analysis shows that age groups 60–65 and >65 years, Saudi Arabia, Middle East, non-healthcare worker, comorbidity, symptomatic, camel-acquired infections, hospital-acquired infections and unknown sources of infection were associated with higher elevated 14-day mortality. The adjusted 14-day analysis shows a Saudi Arabia aHR 4.1; 95% CI 1.012–16.921, Middle East (aHR 5.3; 95% CI 1.070–25.902), non-healthcare worker (aHR 5.3; 95% CI 1.246–22.581), comorbidity (aHR 3.4; 95% CI 1.627–7.000), hospital-acquired infections (aHR 3.4; 95% CI 1.222–9.541) and unknown source of infection (aHR 2.9; 95% CI 1.051–8.221) were independently associated with a higher 14-day mortality.
Table 3 shows unadjusted and adjusted 45-day hazard risks for mortality. In the 45-day unadjusted analysis, the likelihood of 45-day mortality was higher in age groups 30–59, 60–65 and >65 years; Saudi Arabia; Middle East; non-healthcare worker; comorbidity; symptomatic; camel-acquired infections; hospital-acquired infections; and unknown source of infection. The adjusted 45-day analysis shows older age (>65 years) (aHR 2.3; 95% CI 1.187–4.280), Saudi Arabia (aHR 5.0; 95% CI 1.856–13.581), non-healthcare worker (aHR 5.2; 95% CI 2.056–13.025), comorbidity (aHR 2.7; 95% CI 1.710–4.273), symptomatic (aHR 3.2; 95% CI 1.306–7.730), camel-acquired infections (aHR 2.5; 95% CI 1.245–5.091), hospital-acquired infections (aHR 3.6; 95% CI 1.790–7.078) and unknown source of infection (aHR 3.0; 95% CI 1.502–5.943) were independently associated with a higher 45-day mortality.
Discussion
The study was conducted to estimate the survival rates in MERS patients, specifically 14 and 45 days after experiencing MERS-CoV symptoms and to determine whether there is a significant difference in survival rates by demographic data, disease characteristics and regions using global MERS data that were reported to WHO. The author used the CPHMs and the Kaplan–Meier estimator to calculate survival rates.
According to the data, the estimated overall survival rate was 63.4% (95% CI 60.15–66.60%). The study estimated 14- and 45-day survival rates were 83.67% (95% CI 81.09–86.07%) and 65.9% (95% CI 62.68–69.04%), respectively. The author calculated region-specific 14- and 45-day survival rates (Figs 1 and 3). For the MERS patients studied, the Republic of Korea or other countries (95.83% and 91.67%) had much higher 14- and 45-day survival rates than the Middle East (84.09% and 75.00%) and Saudi Arabia (82.51% and 62.92%), respectively. The differences in the region-specific survival rates remain significant after accounting for patient and disease factors such as gender, age, comorbidity, symptoms, healthcare worker and source of infection. For instance, the hazard of death on 45-day post-symptoms was 4.1 and 5.0 times higher in the Middle East and Saudi Arabia compared with the Republic of Korea or other countries, respectively. The disparities in survival rates between regions are probably explained by the delay in reporting MERS symptoms, and consequently delay its diagnosis [Reference Ahmed15]. The median time from date of onset of symptoms to death was lower in the Republic of Korea or other countries than in the Middle East and Saudi Arabia. More research studies are required to assess whether diagnostic delay [Reference Ahmed15] and disease characteristics can explain the differences in survival rate by geographical regions.
Those aged 60 years and older represent a large portion of the MERS population (39.5%) and they predominantly contribute a high portion of deaths as well. The findings of this study showed that 14- and 45-day survival rates tend to rise with increasing age (Figs 1 and 3) and were similar in women compared with men. The estimate of the 45-day survival rate in patients older than 65 years was 44.86%, in patients aged 60–65 years it was 60.38%, in patients aged 30–50 years it was 74.27% and in young patients aged 29 years or less it was 87.78%. These results support various epidemiological cohorts from Saudi Arabia and the Republic of Korea, which stated that older age is a risk factor for death in MERS patients [Reference Almekhlafi, Albarrak, Mandourah, Hassan, Alwan, Abudayah, Altayyar, Mustafa, Aldaghestani, Alghamedi and Talag8–Reference Chen, Chughtai, Dyda and MacIntyre14]. The high death rate among the older age group could be attributable to the greater number of patients with comorbidities in this group. The prevalence of comorbidities increases with age: 28.6% in the young age group <30 years, 62.7% in 30–59 years, 93% in 60–65 years and 97% in older than 65 years. Thus, comorbidities may be associated with both age and mortality.
Several studies [Reference Mizumoto, Endo, Chowell, Miyamatsu, Saitoh and Nishiura10–Reference Rivers, Majumder and Lofgren13], including the current study, suggest that the presence of underlying conditions was associated with an increase in the hazard of death in MERS patients. More details on underlying conditions are needed to estimate underlying condition-specific survival rates and would be useful to identify which underlying conditions were associated with the lower survival rates. Moreover, prevention and disease management strategies should be assessed as interventions in MERS patients with underlying conditions to reduce the mortality rate in this group.
In concordance with other studies [Reference Saad, Omrani, Baig, Bahloul, Elzein, Matin, Selim, Al Mutairi, Al Nakhli, Al Aidaroos and Al Sherbeeni9, Reference Rivers, Majumder and Lofgren13], being a non-healthcare worker was associated with lower survival rates (Figs 2 and 4). The study included 116 (13.1%) who were healthcare workers, of which five died. The higher survival rates within the healthcare workers group could be attributed to educating healthcare workers on preparedness, access to healthcare or following proper infection control standards. An explanation for lower survival rates in the non-healthcare workers group is the large gaps in public awareness of the clinical symptoms of MERS-CoV [Reference Assiri, Al-Tawfiq, Al-Rabeeah, Al-Rabiah, Al-Hajjar, Al-Barrak, Flemban, Al-Nassir, Balkhy and Al-Hakeem16, Reference Pavli, Tsiodras and Maltezou17]. Public health and health system interventions are needed to reduce the spread of the MERS by raising public awareness in identifying the clinical symptoms and by early screening and diagnosis. This could reduce the high rate of mortality in non-healthcare workers.
Patients who had acquired the infection from camels, hospitals and unknown sources of infections exhibited 2.5, 3.6 and 3 times higher mortality risk compared with patients who had acquired the infection from a household member, respectively (Figs 2 and 4). The healthcare system may use this information to properly develop a support care plan to improve patients’ outcomes.
This study has several limitations. The study used available data on the public source with no details on the underlying conditions. This information could be important to identify which underlying condition is associated with death. Patient condition and clinical outcomes may not be final as data are updated routinely. Another potential confounding factor was not available, such as access to healthcare, and it may be considered a modifiable factor to account for. Finally, an inverse-probability Kaplan–Meier curve may also be appropriate to model this dataset, as it may provide perspective into the data and a visual way to show adjusted survival rates. Despite these limitations, the study author was able to use the estimated 14- and 45-day survival rates, measuring the time from symptom onset to outcome. To date, no study has provided survival estimates and links to regions. The study provided information on region-specific 14- and 45-day survival rates, which are found to account for the differences in mortality. The large sample size used was also the main strength of this study. Future study could investigate diagnostic delay, which can be defined by the difference between date of symptom onset and the time of diagnosis. This may reduce poor outcomes.
Conclusions
The study estimated 14- and 45-day survival rates after initial onset of symptoms: 83.67% and 65.9%, respectively. The results demonstrated a link between mortality and geography, disease and patient factors such as regions, symptoms, source of infections, underlying medical conditions, modes of transmission, non-healthcare workers and older age. Educational programmes, access to healthcare and early diagnosis could be implemented as modifiable factors to reduce the higher mortality rates in MERS patients.
Additional files
None.
Ethical approval and consent to participate
Not applicable.
Consent for publication
The author read and approved the final manuscript.
Availability of supporting data
The data used for the analysis can be obtained from the study author.
Declaration of Interest
None declared.
Acknowledgements
The author acknowledges the WHO for making MERS-CoV data publicly available. No funding was provided for this study.
Authors’ information
College of Public Health and Health Informatics, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.










