“No. Not at all. And we have it totally under control. It’s 1 person coming in from China, and we have it under control. It’s - going to be just fine.” On January 22, 2020, President Trump responded to a question from the press if there was cause to worry about a pandemic following the emergence of SARS-CoV-2 in China. 1 What emerged was a deadly pandemic that had significant impact on human lives as well as economic and social stability. Reference Ciotti, Ciccozzi and Terrinoni2 Coronavirus Disease 2019 (COVID-19) emerged in Wuhan, China in late 2019 and spread throughout the world. Reference Hui, Azhar and Madani3 The interconnectivity of the world and the expansion of borders with international interdependence has led to an increase in easy world travel that made the spread of COVID-19 a global threat. Within 3 weeks, infections had begun to spread throughout Asia, Europe, and North America. Reference Brahma, Chakraborty and Menokee4 A limited diversity of supply chains for personal protective equipment and components to support adequate testing further damaged a successful containment and response to the virus. Reference Ranney, Griffeth and Jha5 The world has been at war with the novel coronavirus throughout the year 2020 and into the middle of 2021, with the pandemic continuing to linger. The missteps of top government leaders downplaying or covered up the crisis in the beginning allowed the pandemic to spread easily without any sophisticated mitigation measures. Reference Colglazier6 The vulnerabilities of our biodefense structure were highlighted by 2 major failures: (i) the Chinese government not alerting the world on time, and not quickly supplying diagnostic data, infection statistics, and access to the World Health Organization (WHO), and (ii) the United States government not taking timely mitigation action and employing early testing. This led to 34.4 million cases and 610,000 deaths in the United States as of July, 2021. Reference Colglazier6
The United States has a complicated history with biosecurity as policymaking, biodefense activities, and government transparency have historically been in contention. Reference Vogel, Lakoff and Collier7 The terror attacks of September 11, 2001 uncovered various weaknesses in the national public health infrastructure that have persisted into the current pandemic. The anthrax attacks which soon followed were the first domestic occurrences of bioterrorism and exposed additional deficiencies in the local, state, and federal response capabilities. Since only minor investments were made during the late 1900s into public health preparedness, awareness was only beginning to grow about the threats of emerging and reemerging infectious diseases along with the concerns about the intelligence about an extensive Soviet bioweapons program. Reference Lederberg8,Reference Alibek and Handelman9
Common themes in response gaps can be discovered by identifying, analyzing, and comparing the stated objectives, response focus and outcomes of the spread of COVID-19 within the United States. These themes can be compared to the goals and advancements of public health preparedness and the current biodefense structure, and can then be used to highlight the gaps that led to the significant impacts of the COVID-19 pandemic. Comparing the gaps in our preparedness for a novel event such as SARS-CoV-2 to the principles of public health emergency management can provide a platform through which we can discuss how public health emergency management is crucial to biodefense capacity building.
Key terms and concepts
Biodefense is any “action designed to counter biological threats, reduce risks, prepare for, respond to and recover from bioincidents.” 10 These actions include a wide variety of activities such as bio-surveillance, threat monitoring and awareness, biological arms control and nonproliferation, counterterrorism, biosafety, and biosecurity, the development of medical countermeasures, medical planning and preparedness, and response and recovery activities. Reference Alibek and Handelman9 The coordination of these activities across the federal government is outlined in the National Biodefense Strategy which calls upon the 4 vital national interests from the National Security Strategy, 2017 of “protecting the homeland, the American people and the American way of life, promoting American prosperity, preserving peace through strength, and advancing American influence.” 10
Similarly, biosecurity is the strategic and integrated approach to analyzing and managing relevant risks to human, animal, and plant life and health, and associated risks for the environment. 11 This focuses on the critical link that exists within different sectors, and the potential for hazards to move within and between sectors, with system-wide consequences. The goal is to prevent, control, and manage the risks to life and health in a similar scenario as the biodefense landscape.
Biodefense landscape within the United States
The 1990s brought an increased focus on combating biothreats amid proliferating fears of novel diseases and bioterrorism. The United States’ defense planners began to conceptualize a public health infrastructure that was a bulwark of national security. The established goal to counter bioterrorism required a strategy of public health surveillance, but the traditional policies and methods of countering the proliferation and deterrence of biological weapons became ineffective against the proliferation of nonstate actors and individuals. Reference Fearnley12 A surveillance system, meant to operate within the public health infrastructure, was designed to detect outbreaks, coordinate ameliorative responses and geographically locate release points for law enforcement. Reference Fearnley12 A dual use strategy was then suggested such that preparations for a biological attack could serve to enhance other public health activities. Reference Fearnley12 Syndromic surveillance was the functional apparatus that was turned from a local health department initiative to detect unexpected or unusual outbreaks of diseases into a security strategy. This method involved monitoring non-specific data sources such as emergency calls, pharmaceutical sales, and Emergency Room census, to find any concerning trends. Reference Fearnley12
The Department of Homeland Security was created following the terror attacks on September 11 to act “as a focal point regarding natural and manmade crises, and emergency planning.” 13 The anthrax attacks provided additional resources to coordinate and respond to bioterrorism leveraging the Department of Health and Human Services, and the operating divisions of the Centers for Disease Control and Prevention. Reference Katz, Attal-Juncqua and Fischer14 In 2002, the United States enacted the Public Health Security and Bioterrorism Preparedness and Response Act with nearly $1 billion appropriated annually to support local preparedness and response to address bioterrorism threats. Reference Heinrich15–17 While the funding in biodefense is in the order of millions of dollars, disease outbreaks are both lethal and costly. Between 1997 - 2009, the economic losses from 6 major outbreaks averaged $6.7 billion per year with the 2014 - 2016 Ebola epidemic costing around $53 billion. Reference Huber, Finelli and Stevens18
The biothreat and the current biodefense posture was influenced by actions that came long before the September 11 and anthrax attacks. During the first Gulf War, the United States military forces could detect chemical agents and warn its forces of an attack, but they had significant shortfalls in the ability to detect biological threats. 19 Several billions of dollars in funding for biodefense were exclusively the domain of military agencies with the primary focus of protecting troops against biological warfare programs from state actors while engaged in combat. Reference Enemark20 Funding was also placed into biological detection systems, such as Bio-Watch even though these systems “will remain imperfectly reliable, environmentally insensitive, slow, range-limited, and difficult to operate for the foreseeable future.” Reference Gregory, Howitt and Pangi21 In contrast to other systems, the United States created 8393 chemical detectors, 171 combined systems, and 453 biological detectors in fiscal year 2009. 22 The following year included 25454 chemical specific detectors, 843 combined chemical, biological, and radiological systems, but only 40 biological detectors. Reference Webber23 There is an inherent bias towards the military that exists within the biological defense program of the United States that is hindering the development of a more sustainable infrastructure to respond to any type of biological threat. Biological threats were steadily deprioritized in the years after September 11 because of the belief that they were not easily obtained and could not cause widespread impact along with the preference in the United States’ defense structure to focus on chemical, nuclear, radiological, and explosive threats. The emergence of SARS-CoV-2 and the COVID-19 pandemic necessitates a change in this posture to restore funding to protect against biological threats which have proven largescale consequences for health, economics, and social order.
Within the current response structure are 7 core capabilities of detection and diagnosis, attribution, communication, medical countermeasure development, medical countermeasure dispensing, medical management, and environmental cleanup. Each are essential for addressing naturally occurring diseases and man-made outbreaks, but for the United States’ focus on terrorist activities. There is still a lacking stockpile of medical countermeasures that would not be enough to address the needs after large-scale attacks and could not aid in an attack that utilizes resistant or novel pathogens. Reference England24 There is a large mismatch between public health and biodefense funding. Evaluating the resources available to counter both intentional and natural threats show an evidentiary gap between the number of deaths and illnesses from infectious diseases and those caused by bioterrorism in a contrast to the available funding to prepare for each type of event. Biodefense focused on terrorism has increased from less than a billion dollars to over $8 billion following the September 11 attacks even though only 5 people have been killed in bioterror attacks since 1900. Reference Hunger, Radosavljević and Belojevic25 This is in direct contrast with the $5 billion for tuberculosis control which killed 1.7 million people in 2009 worldwide and similarly 1.8 million died from AIDS-related illness with the United States support being $10 billion short of what is needed to address the threat. Reference Hunger, Radosavljević and Belojevic25
In 2007, the World Health Organization (WHO) released its annual World Health Report titled “A safe future: global public health security in the 21st Century.” Noting the success of public health measures in addressing microbial scourges like cholera and smallpox in the 20th century, the WHO issued a warning about the alarming shift in the delicate balance between humans and microbes. Reference Fearnley12 Listing a series of factors including demographic changes, economic development, global travel and commerce and conflict, the WHO suggested a heighted risk of disease outbreaks ranging from infectious diseases to bioterror attacks. Reference Fearnley12 The WHO proposed a new framework to address the changing threat landscape. ‘Public health security’ attempted to merge the previously segregated technical and political domains. Specifically, bioterrorism had traditionally been a focus of national security-oriented organizations within the national defense with infectious disease being problems of public health, although, infectious disease throughout history has not be unrelated to conflict and military affairs. Reference Fearnley12
Only recently has the military begun to focus more on health security as a general topic, including infectious diseases with the military beginning to play a role in the Global Health Security Agenda. Reference Webster26 The Global Health Security Agenda places a focus on the all-hazard approach to biodefense with effort to confront antibiotic resistance, epidemics, bioterrorism and disease outbreaks. The COVID-19 pandemic and the multitude of biodefense capabilities failures will likely increase the calls for an evaluation and overhaul of the current system to increase our defense measures for both intentional and natural biological threats.
Public health emergency management
Following the September 11 terror attacks, the federal government worked to reframe the roles and responsibilities of emergency preparedness and response. Initially, focus was placed on biological events after concerns prompted by the Amerithrax Attacks within the United States. The financial mechanisms, however, were not well aligned with the ability to prevent the spread of infectious agents or reduce the impact on public health. Reference Katz, Attal-Juncqua and Fischer14 A large part of the emergency preparedness and response efforts were left to the local levels which maintain organizations that lack the clear funding mechanisms or well-defined authorities for sustained preparedness activities to be able to deal with a biological threat. Following various national disasters including Hurricane Katrina, the ambiguities in the national guidance for ‘all-hazards,’ emergency preparedness and response, and the fear of the emergence of pandemic influenzas, caused the creation of the Assistant Secretary for Preparedness and Response within the Department of Health and Human Services. The Public Health and Medical Services Annex along with the Biological Index Annex highlight the Department of Health and Human Services as the coordinating agency for preparedness and coordination of public health events. 27
The funding for public health preparedness programs is generally completed through routine congressional appropriations. The appropriations for domestic health security fluctuate from year to year and do not frequently provide the necessary contingency funds to respond to biological incidents. Reference Katz, Attal-Juncqua and Fischer14 The Public Health Emergency fund was created in 1983, but no appropriations for the fund have been noted since fiscal year 1999 and the account maintained a 0 balance throughout the 2010’s. 28 While focus was immediately placed into building capacity of public health emergency preparedness following the September 11 and Anthrax attacks, due to non-existent capabilities before the attacks, there is still substantial room for improvement. Most federally funded public health emergency preparedness states reported increased capabilities from before September 11 through 2016, with the number of jurisdictions having increased capability functions including countermeasures and mitigation, increasing by nearly 200% by 2014. Reference Murthy, Molinari and LeBlanc29
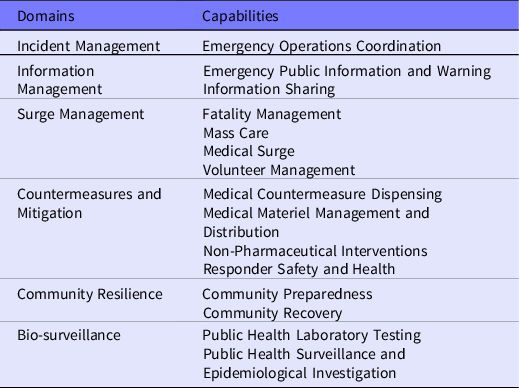
Public health emergency preparedness has 6 domains and 15 capabilities that are a part of the Centers for Disease Control and Prevention national standards. Each of these domains are crucial links in a chain that provides biosecurity that could help address both intentional and unintentional biological threats. Minimal research has been done to suggest public health emergency preparedness focuses to better improve biodefense capabilities.
While funding was initially allocated to public health emergency preparedness capacity building, beginning in 2003, the funding per capita has steadily declined. Reference Murthy, Molinari and LeBlanc29–Reference Davis, Bevc and Schenck31 As the funding started decreasing, states reported challenges in their overall capability functions in the 2010s. There were missing or incomplete plans, difficulties in securing trained personnel, and inadequate funding for recruitment. The gaps also included lack of supporting infrastructure, administrative barriers, and additional actions needed for the active function. Reference Murthy, Molinari and LeBlanc29 The decrease in funding for public health emergency preparedness has left states vulnerable to both intentional and natural biothreats. New York City’s Department of Health and Mental Hygiene reported an inability to offset the continuous decline in Public Health Emergency Preparedness (PHEP) funding. This led to a decrease in their surveillance and response capacity, public health emergency preparedness workforce staffing and development, and number of volunteers from Medical Reserve Corps. There was also a concern that limited resources would have a negative impact on the department’s ability to respond to real emergencies, train and exercise, and participate in regional collaborations. Reference Marquez, Patel and Raphael32 During the COVID-19 pandemic, New York city was 1 of the most impacted locations in the United States. Similar concerns with the lack of funding for public health emergency preparedness were suggested in North Carolina where there were reports of declines in their preparedness capabilities, especially with surveillance which would be crucial to identify any biothreat presence, either intentional or natural. Reference Davis, Bevc and Schenck31 The decrease in funding also impacted their planning and protocols, communication, and incident command which would limit the effectiveness in response to any type of public health threat.
Various examples in recent United States history have suggested the usefulness of preparedness and response capabilities for public health threats including the 2009 H1N1 influenza pandemic, 2014 Ebola virus outbreak, and 2016 Zika virus outbreak. Reference Oussayef, Pillai and Honein33–Reference Redd and Frieden35 The need for these capabilities is highlighted by the life safety considerations as well as the far-reaching political, economic, and social consequences that can result from a public health emergency. Reference Heymann, Chen and Takemi36,Reference Patel and Phillips37 The progress made since September 11 that developed, built, and started to create sustainable public health preparedness capabilities can serve as the foundation for public health preparedness and response systems that can build resiliency for biothreats, either intentional or natural, creating a truly bio defended nation. Reference Redd and Frieden35 There are important synergies between biodefense and public health which need to be leveraged in order to better protect the United States from likely natural diseases threats as well as the increasing likelihood of bioterrorism in the post COVID-19 era.
Statement of purpose
The current biodefense landscape within the United States has seemingly been inadequate to initially prevent the spread of an infectious disease within the United States and to effectively respond to an outbreak with adequate safety measures. There were catastrophic failures at the intersection of science and policy which has led to “disastrous outcomes for public health, the economy, and international collaboration.” Reference Colglazier6
This study explores the biodefense and public health preparedness landscape for trends in federal support and capacity building. The study investigates the applicability of public health emergency management principles to the biodefense structure.
Methodology
This study uses thematic analysis and mixed methods, and concurrent triangulation strategy methodologies applied to this quantitative and qualitative study in exploring the landscape of biodefense within the United States to inform the next generation of preparedness for biothreats. The benefits of these methods include the flexibility and accessibility for the researcher, usefulness in key points within large amounts of data, and the ability to illuminate insights for future policy development. Reference Braun and Clarke38,Reference Guest, MacQueen and Namey39 Many themes can arise from data, but these methods allow for the traceability of the identified themes to the original research questions which support the development of findings and recommendations. Reference Braun and Clarke38,Reference Braun and Clarke40 The failures of the COVID-19 pandemic response will serve as a platform from which to suggest an emerging role for public health in addressing the security threat of infectious diseases.
Process
A mixed method was utilized in this study to investigate the qualitative and quantitative factors of the research inquiry. Academic literature, news reports, and governmental documents were examined for applicable research and data that has contributed to identifying the problems with the current biodefense structure. The research was utilized to offer solutions that will enhance the coordination and utilization of public health emergency management in the face of evolving natural and intentional threats. Thematic analysis is “a method for systematically identifying, organizing, and offering insight into patterns of meaning (themes) across a dataset.” Reference Braun and Clarke40 Thematic analysis will allow for the discovery and description of themes within the data. Reference Guest, MacQueen and Namey39 The themes that are identified including concepts, ideas, and patterns will be collated and applied through conceptual tools. Reference Nisbett41 Braun and Clarke’s 6-phase framework, briefly described below in Table 1, for thematic analysis will assist with defining the important information from a review of the literature. The process has been suggested as comparable to other qualitative methods. Reference Braun and Clarke38,Reference Corbin and Strauss42–Reference Maguire and Delahunt44 The analysis will have feedback loops between the literature review steps. Reference Javadi and Zarea43,Reference Maguire and Delahunt44 The concurrent triangulation design permits that use of qualitative and quantitative data to more accurately define and analyze the relationship among the variables of interest (see Figure 1). Both quantitative and qualitative data are collected during the same stage and the design is theoretically driven to initiative social change and advocacy to provide support for various perspectives. Reference Creswell, Plano Clark and Gutmann45
Table 1. Braun & Clarke’s framework

Figure 1. Mixed methods concurrent triangulation. Reference Creswell, Plano Clark and Gutmann45
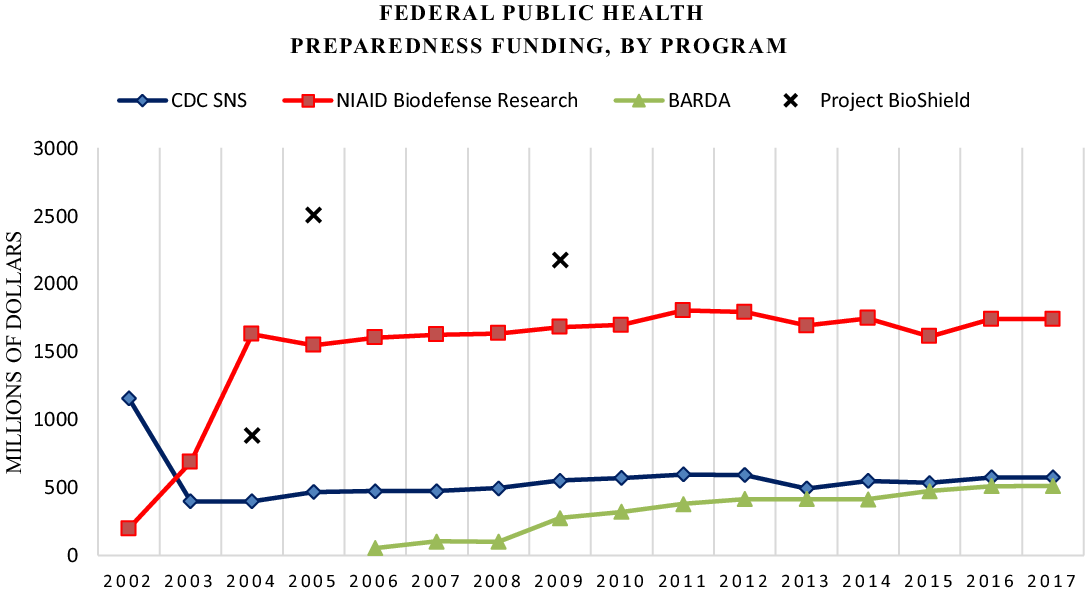
Figure 2. Federal pandemic preparedness financial support, 2003 – 2020. Source: Watson et al. 2017. Reference Watson, Watson and Sell46

Figure 3. Federal pandemic preparedness funding, by program, 2002 - 2017. Source: Watson et al. 2017. Reference Watson, Watson and Sell46

Figure 4. Department of Defense base budget, 2003 – 2020. Source: Office of the Under Secretary of Defense (Comptroller)/CFO.
These methods will provide the flexibility and accessibility of an inquiry into an emerging need in the biodefense infrastructure. The ability to find key points from large volumes of data within the case study is also a benefit of the analysis method which will provide insights for policy development. Reference Braun and Clarke38,Reference Guest, MacQueen and Namey39
Data collection
The data collected for this research comes from numerous documents that span government, non-governmental organizations, and academia. Due to the complexity of the research, the strategy selected for analysis allowed for smaller samples sizes for the deriving of meaningful material, rather than a generalized approach from large populations as expected of quantitative research.Reference Dworkin 47 In order to identify important common patterns, a maximum variation sampling strategy was used during analysis.Reference Creswell 48 All information was gathered from publicly available documents including reports from the United States Senate.
The open-sourced Global Terrorism Database was also used for evaluation of CBRN attacks from January 1970 to December 2019. The database includes events where there may be uncertainty as to whether an incident meets all the criteria for inclusion as a Global Terrorism Database terrorist incident. All events including those meeting partial criteria were included as well as attacks that were attempted, but not successfully carried out. The data base does not include any acts of state-based terrorism.
Validity and reliability
A major concern with a study of this nature is to determine what is needed to achieve validity and reliability within the context of research design based on the problem and objective.Reference Nardi 49 According to Nardi, “validity is about accuracy and whether the operationalization is correctly indicating what it’s supposed to.”Reference Nardi 49 The limitation of a heavily quantitative study for thematic analysis is rooted in the historical grounding of the analysis.Reference Guest, MacQueen and Namey 39 A surrogate mechanism is therefore needed to overcome these challenges in validity and reliability.Reference Guest, MacQueen and Namey 39 The use of a consistent process in this research will serve to address the validity and reliability challenges which is the purpose of the Braun and Clarke’s framework and the mixed methods concurrent triangulation. Reference Guest, MacQueen and Namey39,Reference Tobin and Begley50
Analysis and results
A total of 8 main failure themes were identified which ultimately relate to the public health preparedness capabilities that could be leveraged to ensure a bio-defended nation. Additional results suggested a decreasing funding posture for the public health preparedness and the security threat posed by infectious diseases.
Analysis
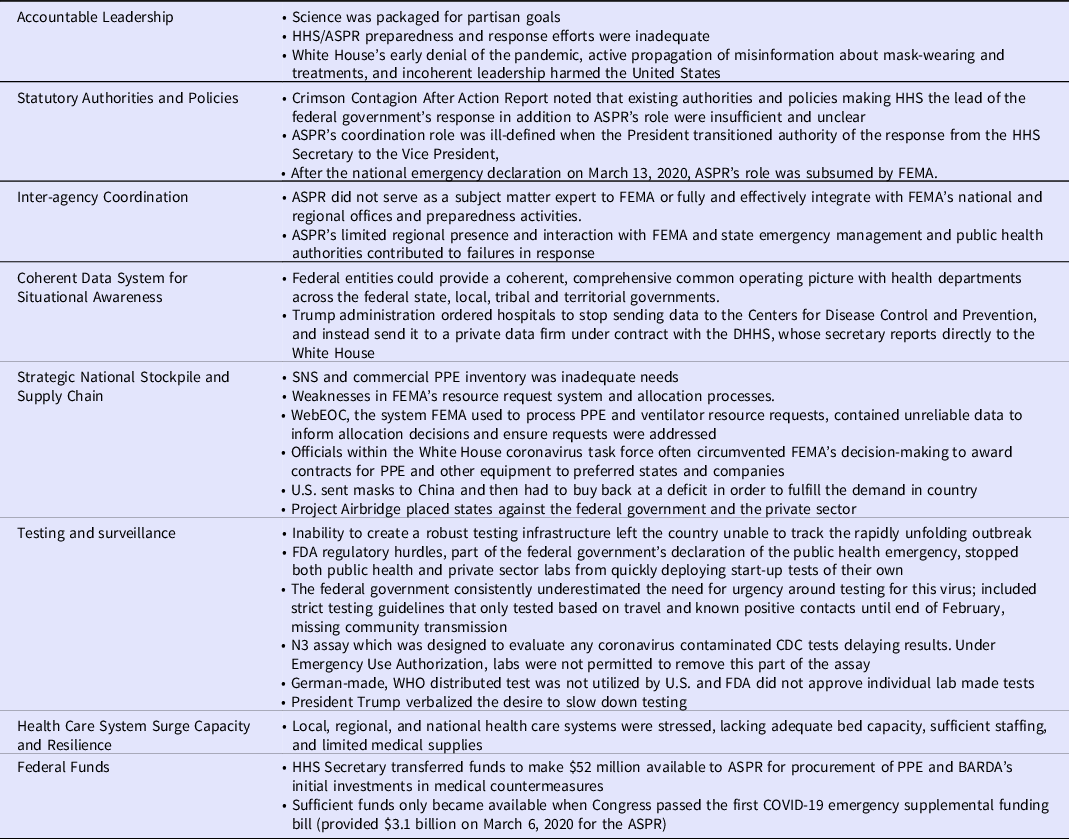
The qualitative and quantitative methods of analysis are employed conjointly to provide an overall evaluation of the research question. The employed integrated methods of data analysis provide more context to a complex infrastructure and a stronger basis for policy improvements. The themes of failures during the COVID-19 pandemic are patterns of meaning that exist across the dataset from both academia, governmental, and news resources. Reference Braun and Clarke40 The analysis of the breadth of literature yielded the 8 themes of failure during this pandemic (see Table 2). The thematic interpretations and additional analysis of the literature contributed to the foundational understanding of the current landscape and the areas for applicability of the evaluation of infectious disease as a security threat and the role of public health preparedness in biodefense.
Table 2. Key failure themes of the COVID-19 pandemic
Results
The results of this research are presented in various forms. The thematic analysis evaluating the failures of the COVID-19 pandemic found 8 main themes.
The CDC has provided significant funding for preparedness work by local health departments since 2001. The Public Health Emergency Preparedness cooperative agreement program enables these departments to conduct various necessary health surveillance and response tasks. The program funds the creation and sustainment of information and communication systems, routine surveillance efforts for infectious diseases, community education and risk communication, exercises, and efforts to address vulnerable populations. PHEP funding enabled public health laboratories to quickly address testing needs for the emergence of the Middle East Respiratory Syndrome (see Figure 2).
Private health systems get funding through a hospital preparedness program created by Health and Human Services Department and maintained by ASPR (see Figure 3). The program assists coalitions of local hospitals, public health agencies, and emergency managers prepare for sudden health threats. The funding also supports planning for health system surges, trainings, and exercises, and creating additional coalitions to bring together public health and healthcare to coordinate a response. The funding has supported responses to various disasters such as evacuation planning for hurricanes or establishing high-containment isolation units used to treat highly infectious or lethal diseases. The decrease in funding for these health preparedness programs are in direct contrast with the Department of Defense base budget (see Figure 4).
Discussion
Research question (RQ) 1
Is the current biodefense structure providing adequate core capabilities?
The analysis yielded 8 common themes of failure as noted throughout the literature; accountable leadership, statutory authorities and policies, interagency coordination, coherent data system for situational awareness, strategic national stockpile and supply chain, testing and surveillance, health care system surge capacity and resilience and federal funds. The commonalities of these themes from various forms of literature including media reports, academic journals and governmental documents suggest the importance of these failure themes that caused the devastation of the COVID-19 pandemic. While the debate about the true origins will likely never be resolved, the devastation from this virus shows the lack of biodefense capabilities within the United States against natural, accidental, or intentional threats. The failures in response lie within the key themes and state goals in the progress in public health preparedness (see Table 2). These failure themes would be consistent in the presence of either intentional or natural threats, although the United States benefited greatly from the lessened impact of the virus on younger and healthier populations, at least prior to the emergence of different variants. The bioterrorism focus of biodefense still did not provide the core capabilities necessary to combat what would be a weaponized biothreat, a potentially even more complex and dangerous than SARS-CoV-2. It is clear from the on-going response to COVID-19 that the United States has an inadequate biodefense system that lacks the core capabilities necessary to respond to the wide complex of potential biothreats.
Research questions (RQ) 2
Could public health emergency management principles be applied to the structure of biodefense in order to increase capabilities?
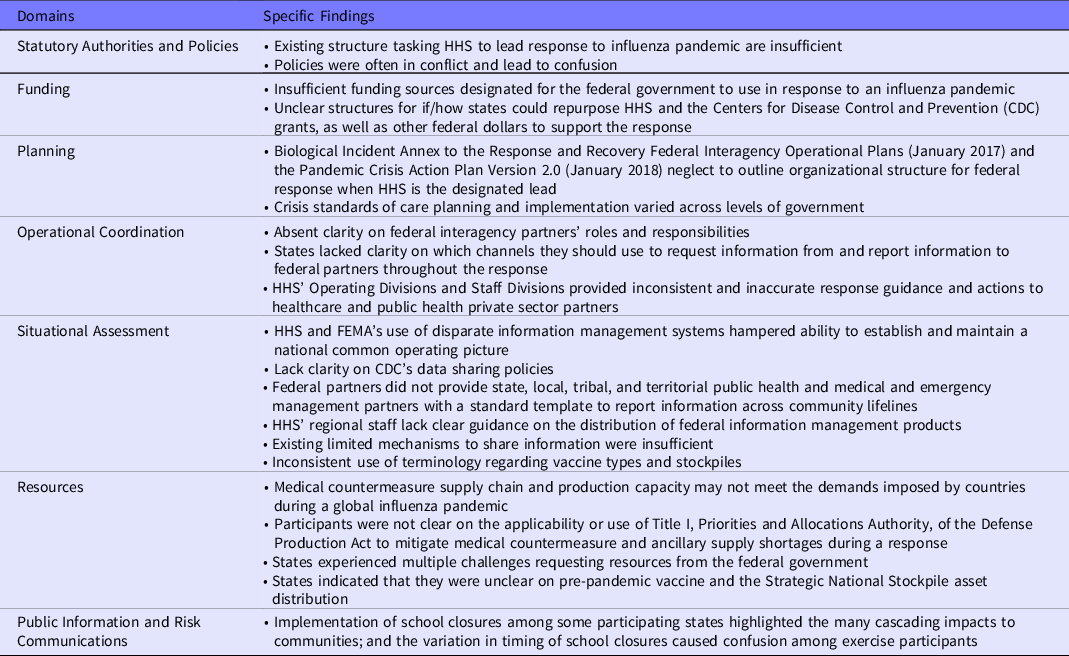
The current biodefense structure is inadequate and framing infectious disease as a security threat can improve preparedness efforts. The means by which this can be implemented are through the adoption of public health emergency management principles in the biodefense structure to increase capabilities. The main failures of the current pandemic response as outlined in Table 2 related to the public health preparedness capabilities which are outlined in Table 3. Failures in accountable leadership and interagency coordination can be addressed through the incident management and Emergency Operations Coordination framework. The coherent data systems are a core capability within information management as Emergency Public Information and Warning information sharing that is essential for public health work could improve identification and isolation of threats, either natural or intentional. It would also be an additional improvement to the testing and surveillance framework which falls under bio-surveillance. Increasing the abilities and Public Health Laboratories to test and analyze even novel samples along with the abilities and funding for public health surveillance and epidemiological investigation could additionally reduce the impact of the presence of any biothreat. The failures and limitations in the health care system surge capacity and resilience would be addressed through the support of the surge management, countermeasures and mitigation domains. Mass care, surge management, medical countermeasure dispensing and non-pharmaceutical interventions can not only increase the ability to save lives from biothreats, but in addition can deter the use of bioweapons due to their negated impact, still promoting the bioterror concerns of the current biodefense structure. Similarly addressing the strategic national stockpile and supply chain failures can increase our resilience to any threat, promoting a one health like approach to biodefense. This could address the weaknesses in FEMA’s resource request system and allocation processes and unreliable data which informs allocation decisions and ensures requests are accurately adjudicated.
Table 3. Public health preparedness capabilities 51
It is clear that the current biodefense infrastructure was incapable of addressing a biothreat and improvements are necessary to promote improve United States’ defense capabilities. Supporting public health emergency preparedness measures can not only improve our biodefense posture, but can also improve our resilience to a myriad of threats as public health preparedness funding has assisted in responses to SARS, the 2009 H1N1 influenza pandemic, the Ebola cases in the United States, and the Zika virus pandemic along with Hurricanes Katrina and Sandy, the 2011 Joplin, Missouri, tornado, the 2013 Boston Marathon bombing, and the 2014 West Virginia Elk River chemical spill.
Significance and recommendation
The COVID-19 pandemic has had major impact on the United States with consequences lingering for generations. The United States had the tools for success, but the implementation of these tools is a major failure. The 2019 Global Health Security Index which assessed levels of global health security across 195 countries, listed the United States as the number 1 most prepared nation for a pandemic. The United States needs to reinvest in the public health emergency preparedness infrastructure to improve its biodefense capabilities. The efforts to improve public health preparedness (see Table 4) have been inadequate. The biothreats will continue to be present, either in the form of a natural emerging or reemerging infectious disease, or a biological weapon. As suggested by Dr. Anne Schuchat of the CDC, the United States was unprepared for the coronavirus, the response “wasn’t a good performance,” and there’s still ‘a lot of work to do’ to get ready for the next pandemic when it comes. 52 There was a complex, systemwide assault that has highlighted the numerous vulnerabilities that are present in our ability to respond to a wide array of biothreats.
Outbreaks of SARS, Ebola, Zika, influenza, among others, have cost billions in lost productivity around the world. The risk of a catastrophic biological threat was evident prior to the emergence of SARS-CoV-2 due to the increasingly interconnected world and the heightened risk of spillover from animals to human. In this era of increased global travel, infectious disease outbreaks will only increase. As climate change worsens, catastrophic weather-related events will place enormous demands on health agencies to have the capacity to prepare for and mitigate such disasters. Leveraging on the health security components of the Global Health Security Index can help facilitate protection from various biological threats which can ensure a biosecurity strategy that integrates traditional threats with broader public health crises, merging the two governance structures for seamless operations in the face of a biothreat.
The results of this study are concerning due to their parallels to the findings of the 2019 Crimson Contagion Functional Exercise. The exercise was meant to determine the nation’s ability to respond to a large-scale outbreak of a novel avian influenza virus (H7N9) strain, a virus which spreads quickly amongst humans with high rates of morbidity and mortality. The After-Action Report following the 4-day exercise, which included 19 Federal Departments/Agencies, 12 states, 74 local health departments and coalition regions, 15 tribal nations and pueblos, 87 hospitals, over 100 healthcare and public health private sector partners, and the White House National Security Council, yielded stark similarities in failures of response to those identified in the thematic analysis (see Table 5).
Table 4. Progress in public health preparedness, 1999 - 2011
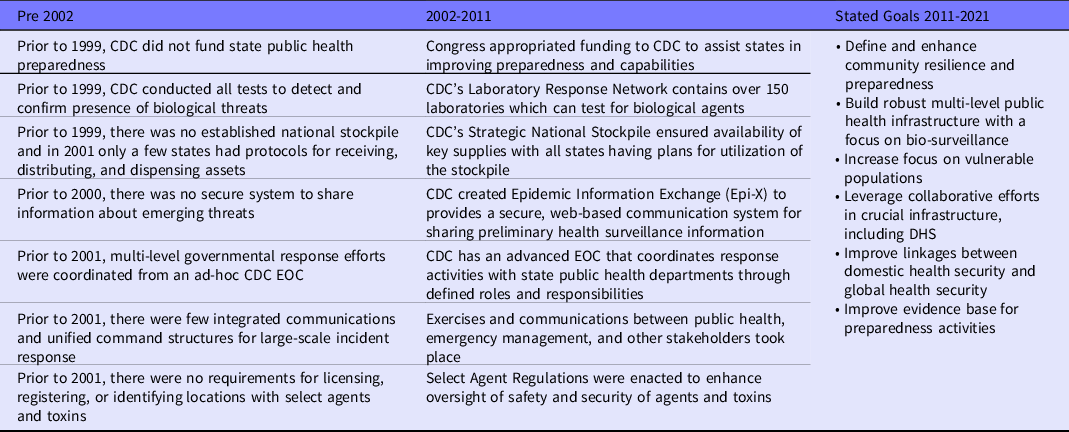
Table 5. Crimson contagion key failure findings and outcomes
The summarized recommendations for policy makers to counter the increasing prevalence of biothreats are as follows:
-
1. Promote strong, effective leadership and coordination: The United States must commit to a collaborative framework that integrated public health and its preparedness domains into the biodefense infrastructure that is currently heavily focused in law enforcement entities focused on preventing terrorism. Public health emergencies that are a result of an infectious disease outbreak or even a bioweapon, require national coordination since biological agents are not easily isolated. Effective coordination of response by state, local, tribal and territorial authorities are crucial to a successful response and mitigation of devastating impacts. Clear and effective leadership can assist with promoting all-hazard preparedness and operation response coordination during public health emergencies. This coordination must also focus on federal efforts an infectious disease outbreaks and bioweapons have the potential to span the nation. ASPR must integrate with FEMA to ensure coordination through the emergency management cycle, including the pre-incident phases. ASPR has a crucial role in coordinating the important resources of the Department of Health and Human Services along with other federal medical and public health expertise that will be necessary to support local and state departments. Coordination will allow for the adequate distribution of the right care to those in need, a major gap of the COVID-19 pandemic.
-
2. Strengthen public-private-government partnerships: Biothreats require a lot of government response in order to be successful. Expanding, strengthening, and sustaining partnerships between government agencies, the private sector, and academia will be critical for preparing and responding to the next threat. Operation Warp Speed and partnerships through the National Emerging Special Pathogen Training and Education Center and Regional Disaster Health Response System were vital to the expansion and mobilization of medical capacities and capabilities needed to address the gaps during the pandemic. Steady state agreements and cooperation can better improve our capabilities, capacities, and resources to prevent, mitigate, and respond to any biothreat no matter the source. These partnerships will help ensure a collaborative approach to response that does not place the federal government, state governments, and private entities in competition for the resources necessary to save lives.
-
3. Innovation, capacity, and capability improvements: A valuable lesson learned from the September 11 terror attacks was the lack of imagination of security professionals. The COVID-19 pandemic highlighted the failure of imagination of health and security professionals. It is necessary to support innovation to expand public health and medical preparedness and response capacity and capabilities. This is necessarily completed through the funding and support of public health emergency preparedness which will consequently support biodefense capabilities against all types of biothreats. Innovation to medical countermeasures, the health care system, and public health programs can improve our resilience to threats and deter any intention bioweapon uses.
Limitations
There are 5 significant limitations of this study: (1) focus on health security aspect of biodefense, (2) analysis of documents/artifacts only, (3) the constraints of an on-going pandemic, (4) the political discourse surrounding the topic, and (5) the domestic focus. The first limitation is necessary when utilizing COVID-19 as a case study, however future research would need to address the social and political aspects of global health security and counterproliferation of biological weapons. The second limitation is driven by the need to balance the depth of analysis with available time within a 12-month executive program during which this research was conceptualized and conducted. The third limitation considers the lack of available information and the conclusions that can be drawn as the pandemic continues with likely new information to be learned in the future. The political discourse surrounding the issue, even including the politicization of mask wearing made the analysis a difficult balance between highlighting the failures to recommend policy changes while trying to eliminate the politization of the findings. The final significant limitation is the focus on domestic policy and recommendations. Biodefense includes complex considerations of global health and international cooperation that would be too complex to discuss in this study but could be an important area for future research.
Conclusion
A redesigned biodefense framework is necessary to address the gaps and failures in response to the COVID-19 pandemic. Biothreats will remain an increasingly complex and dangerous threat to the United States and its interests abroad. Biological threats, whether natural occurring, intentional, or accidental have the potential to cause loss of life, sustained economic damage, societal instability, and disruptions to global security. Disruptions to the natural equilibrium of the interlinked systems of the world can lead to system failures that have unpredictable damaging impact. The United States cannot afford to shortchange the critical public health infrastructure the nation needs to be prepared for the next pandemic or public health crisis which include bioterrorism. The current pandemic has cost the United States $16 trillion dollars with no immediate end to the pandemic on the horizon, however the cost of preparedness would only be a tiny fraction of the price of the next disaster. As Congress debated President Biden’s $30 billion plan to prevent pandemics as part of the $3.5 trillion reconciliation bill, attempts were made to immensely cut the funding for pandemic preparedness, even as the pandemic continues to devastate the United States. Bio-preparedness is complex puzzle that requires the flawless integration of public health, security and infrastructure in coordination with a consideration of the sociocultural environments, legislative authorities, communications, and behaviors and agency capabilities that exist within the United States.
To reduce the vulnerabilities within the United States, a multidisciplinary approach must address certain steady state disparities such as the urban-rural healthcare divide, health outcomes based on racial and ethnicity, rising prescription drug prices, and other on-going health epidemics within the country. Strengthening our biodefense and health security is essential to protect the United States from diverse biothreats. It is essential to adopt public health emergency preparedness capability domains to share data, knowledge and resources and collaborate an effective response to any threat through accountability in reducing threats. The recommendations in this study require building upon the current biodefense framework and leveraging biosecurity leadership to address the vulnerabilities by funding public health capacities through bipartisan support to better prepare the United States for future threats. A honest, comprehensive review of the failures of the COVID-19 pandemic is necessary to pool expertise to adequately invest in planning, training, mitigation, response, and recovery capabilities.
The United States certainly does not have biodefense totally under control. Preparing for public health crises will directly increase our capabilities for bioterrorism preparedness and vice versa, necessitating the interlinking of these 2 previously distinct focuses. There are no easy answers, only tough trades offs when investing in the biodefense infrastructure. The pandemic revealed fundamental problems with our biodefense preparedness. The United States will have to deal with more biothreats in the future along with other existential natural threats, all on the account of man-made problems. The solution to these threats lies in the ability to incorporate multidisciplinary perspectives to solve the complex web of problems. The ability to address the gaps and failures will necessitate learning from this pandemic. When we are finally able to remove our masks, we must be ready to fix all that is broken together.
Conflict of interest
The authors certify that they have no affiliations or involvement with any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.











