Frontline healthcare workers (HCWs) are at risk of developing psychological problems during the COVID 19 pandemic which are determined by certain bio-psycho-social factors.Reference Gupta and Sahoo1 However, literature concerning this risk is scarce from India, particularly from Central India, which has higher population density and poorer health infrastructure than other parts of the country. Having such literature may act as a guide to policymakers and hospital administrations in order to take appropriate preventive and therapeutic measures with which to ameliorate the psychological concerns of the HCWs. Hence, this study aimed at assessing the magnitude of psychological problems among frontline HCWs as well as their psychosocial determinants amidst the first wave of the COVID-19 pandemic. An online survey was conducted from April, 2020 till July, 2020 involving the HCWs: specialists, junior doctors, nursing staff, and supporting staff (housekeepers and security personals), in a tertiary care hospital from central India to assess their level of psychological problems such as depression, anxiety, and stress scale-21 (DASS-21); as well as to take note of event-related stress symptoms (Impact of Event Scale-Revised-22 [IES-R]). Psycho-social determinants including attitudinal factors such as perceived stigma, sense of controllability over the patients’ conditions, etc., were also considered.
Methods
Descriptive statistics and Chi-square-, Pearson’s correlation coefficient and ordinal logistic regression (LR) (relationship between the socio-demographic, professional profiles of the HCWs, attitude towards COVID19 and their psychological problems) were used for the analysis.
Results
Out of the 315 participants, a sizeable portion had moderate to very severe depression (28.5%), anxiety (31%), stress (18.4%), event-related stress (21.9%), and negative attitudes (about a third) towards the COVID-19 pandemic. Being female (vs male, LR: 2.5- 5.5, P ≤ 0.002), married (vs unmarried, LR: 2.5, P ≤ 0.005 on a measure of stress), working as junior doctors, or supporting staff (vs. nursing staff, LR: 11.08, P < 0.0001), and a higher level of perceived stigma (vs lesser stigma, LR: 6.03 to 14.06, P < 0.0001) and lesser reliance on PPE (vs greater reliance, LR: 5.11, P = 0.003 on a measure of anxiety), and belief of uncontrollability over the patients’ condition (vs greater controllability, LR: 3.01 to 5.41, P ≤ 0.007) had a higher likelihood to experience psychological problems (Table 1).
Table 1. Strength of association of socio-demographic and occupational variables with various psychological outcome measures (ordinal regression analysis)
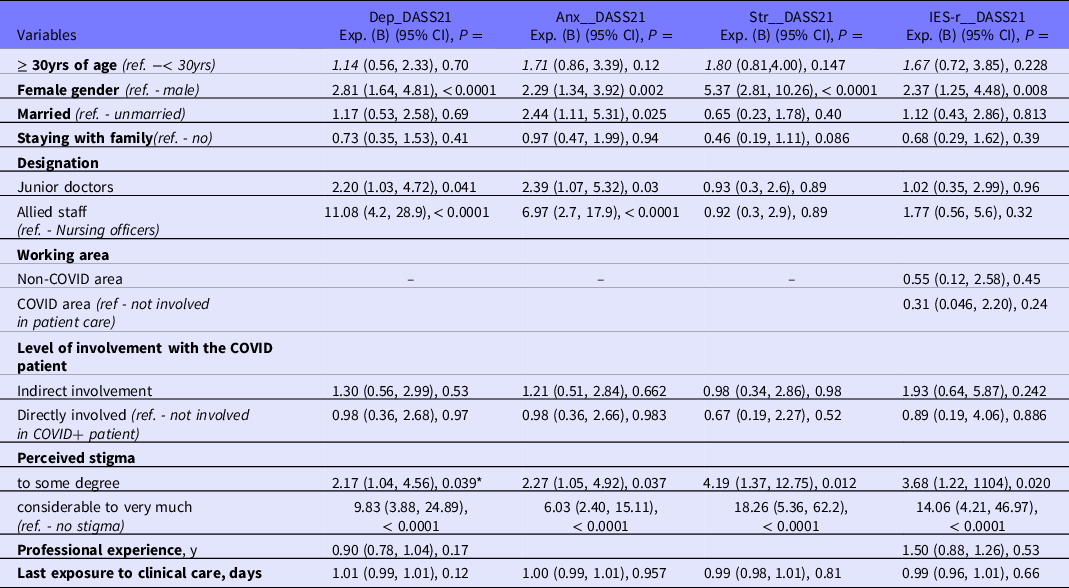
Exp. (B): likelihood ratio - represents that this variable did not achieve the threshold P = 0.2 in the univariate logistic regression analysis to be included in multivariate regression model; ref. - reference category.
These findings are in line with previous literature. Reference Gupta and Sahoo1,Reference Gupta, Prasad and Dixit2 The findings of this study underscore the need for hospital-level mental health support systems for frontline HCWs. Reference Şahin, Aker, Şahin and Karabekiroğlu3,Reference Yıldırım and Worry4 This includes a system of early identification of mental health concerns, peer support systems, tele-counseling services, Reference Gupta, Kumar and Rozatkar5 and COVID support systems for HCWs who acquired the infection (or who are in quarantine). Also, the association between perceived stigma and poor psychological outcomes reflects the need to ensure social security for HCWs, as well as the necessity behind recognizing and rewarding their efforts while spreading awareness among the public. Reference Gupta, Prasad and Dixit2 Furthermore, the importance of having hospital-level support system, effective communication between the HCWs and hospital administration, and having mental health professionals in the hospital infection-control committee cannot be overemphasized. There is an urgent need for tailored support services in order to create a conducive work environment, thereby improving productivity and quality of life. Lastly, HCWs need to be trained in soft skills, such as communication skills, so that they can deal with COVID-19 patients (in possible upcoming waves), and address the vaccination hesitancy among the general public. Future research could build on these findings.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2021.290
Conflict of interest
None of the authors has any association with any commercial entity or agency which could be construed as a potential conflict of interest with regard to the current research work.



