Disasters of all types have profound impacts on human and animal health, the environment, economies and trade, and societies. In 2022, there were 387 natural hazards and disasters worldwide, resulting in the loss of 30 704 lives and affecting 185 million individuals. Economic losses totaled around US $223.8 billion. These numbers do not include the extraordinary impacts of the COVID-19 pandemic or terrorism/armed conflict. 1
The economic losses from animals impacted by disaster events can be significant. The direct impact of disasters on animals was highlighted in the United Nations Office for Disaster Risk Reduction (UNDRR) Annual Report 2019 where an estimated 1.25 billion animals were killed during the Australian wildfires from October 2019 to March 2020. 2 The Food and Agriculture Organization of the United Nations (FAO) analyzed the post-disaster needs assessments undertaken in the aftermath of medium-to-large-scale disasters in Africa, Asia, and Latin America over the decade from 2003–2013. Livestock were the second most affected subsector after crops, accounting for US $11 billion, or 36% of all damage and losses. 3 Animals and animal-related issues are increasingly part of disaster management and risk reduction due to their economic, health and welfare, food security, and social aspects.
Veterinarians are involved in disaster preparedness and response due to the link between human and animal health and the economic and social impacts of animal loss or disease. The World Organisation for Animal Health (WOAH) has undertaken support for member states’ National Veterinary Services through numerous pathways. WOAH has developed and published disaster guidelines for National Veterinary Services, developed veterinary emergency training, and conducted simulation exercises. WOAH accepted the technical item, World Organisation for Animal Health, Veterinary Services and Aquatic Animal Services Engagement in global, regional and national emergency management systems during the 89th General Session of World Assembly in May 2022 as a framework for future activities in this arena. 4
Veterinarians have high rates of anxiety, depression, and suicide. In fact, a scoping review found that veterinarians have higher burnout, anxiety, and depressive disorders compared to the general population and other occupational groups.Reference Pohl, Botscharow and Böckelmann 5 Compounding this underlying risk, the mental health of responders in disaster and emergency events is a significant issue. Medical responders in general are at risk of experiencing a wide range of negative psychological health conditions following a disaster.Reference Brooks, Dunn and Amlôt 6 , Reference Naushad, Bierens and Nishan 7 In the past, depression and post-traumatic stress disorder (PTSD) were the most studied outcomes in medical responders.Reference Naushad, Bierens and Nishan 7 Risk factors for adverse outcomes were found to be lack of social support and communication, maladaptive coping, and lack of training.Reference Naushad, Bierens and Nishan 7 However, studies focused on veterinary disaster responders are limited, and have focused on transboundary disease incursions such as foot and mouth diseaseReference Davies 8 or avian influenza.Reference Lee, Torchetti and Killian 9 Recent research has also been focused on the mass depopulation of swine during the COVID-19 pandemic. In 1 of these studies, Baysinger and Kogan, 2022Reference Baysinger and Kogan 10 surveyed veterinarians involved in depopulation and reported nearly a third of participants had high levels of burnout. In addition, a qualitative study of swine veterinarians outlined the need for additional training and supportive services for veterinarians involved in future depopulation efforts.Reference Bussolari, Packman and Currin-McCulloch 11
Due to the lack of research in veterinary responders and the high rate of mental health disorders in this occupational group, the objective of this study was to determine if there are demographic, operational, or functional factors associated with reported behavioral health issues in veterinary disaster responders. By identifying risk factors for adverse behavioral health outcomes, interventions and policies can be better targeted towards those at highest risk. This study builds on results previously reported from the survey that ascertained the scale and scope of behavioral health issues in veterinary responders and found that 50% of veterinarians responding to the survey experienced behavioral health issues during the disaster event and 32% reported persistence of these issues 6 months after the disaster event.Reference Vroegindewey and Kertis 12
Methods
The Lincoln Memorial University Institutional Review Board (#875 V.0) reviewed and approved the study protocol. This anonymous 24-item online cross-sectional survey was developed to identify risk factors for behavioral health issues among veterinarians involved with disaster response. The survey instrument was evaluated for construct validity by multiple experts in the field, including veterinarians, disaster responders, and health practitioners, prior to use. The survey link was distributed via snowball sampling by email, starting with contact lists of the WOAH headquarters and attendees from conferences related to disaster and emergency management. Two recruitment emails were sent to contact lists, 1 month apart. The survey was kept open 1 month after the second recruitment email was sent. Snowball sampling was implemented because this specific group (veterinary disaster responders) is hard to target and sample from and this method allowed participants to forward the survey invitation to other veterinary disaster responders.Reference Chambers, Bliss and Rambur 13 Data was collected and securely secured on the Qualtrics platform, where informed consent was obtained. The consent form stated that participation was voluntary, and participants could stop the survey at any time. More details about the survey methodology were presented in Vroegindewey and Kertis, 2021.Reference Vroegindewey and Kertis 12
Stata version 18.0 was used for all statistical analyses (StataCorp, College Station, TX). Observations from participants that completed less than 50% of the survey were dropped from the analysis. Small cell sizes in behavioral health outcome reporting were censored to protect against re-identification of study participants. Descriptive statistics were performed to assess factors (demographics, location and length of deployment, awareness of current mental health policies, role while deployed, behavioral health training and support, and work history) associated with the following behavioral health outcomes during and after deployment:
-
1. Anxiety/restlessness/lack of concentration and/or depression (hereafter referred to as anxiety and/or depression),
-
2. Difficulty with personal and/or professional relationships (hereafter referred to as difficulty with relationships),
-
3. Trouble sleeping and/or dreaming/nightmares/flashbacks (hereafter referred to as sleep problems),
-
4. Mood swings, and
-
5. Suicidal thoughts
Statistical significance in quantitative analyses was tested using Chi-square tests or Fisher’s exact tests (when expected counts were less than 5). Statistical significance was set at P ≤ 0.05. Data on the helpfulness of behavioral health support before and during disaster events were summarized descriptively.
Results
A description of the study sample was reported in more detail in Vroegindewey and Kertis, 2021.Reference Vroegindewey and Kertis 12 The final sample size for this analysis was 237 participants after dropping 28 observations due to these participants completing <50% of the survey (Table 1). When applicable, the results state when data were censored to protect re-identification of study participants.
Table 1. Questionnaire variables stratified by behavioral health outcomes that occurred during and/or after a disaster response in a sample of veterinarians (n = 237) 1

1 Missing data summary: Birth year (n = 5); Years as vet (n = 1); Disaster year (n = 4); Disaster type (n = 1); Length of deployment (n = 1); Fieldwork (n = 1); Received support during (n = 1); Received support after (n = 2); Aware of guidelines (n = 1); Anxiety and/or depression (n = 6); Difficulty with relationships (n = 7); Sleep problems (n = 5); Mood swings (n = 8); Suicidal thoughts (n = 10). Bolded values indicate statistical significance of an association between that variable (row) and behavioral health outcome (column) at P ≤ 0.05. Comparisons of each variable with each behavioral health outcome were conducted using Chi-square analyses. Fisher’s exact test was used when exact counts <5.
2 Anxiety/restlessness/lack of concentration and/or depression.
3 Difficulty with personal and/or professional relationships.
4 Trouble sleeping and/or dreaming/nightmares/flashbacks.
5 Indicates censored data due to small cell size.
Behavioral Health Outcomes During and/or After the Disaster Event
Participants that were involved in more than 1 disaster event were more likely to have anxiety and/or depression (43.4% versus 28.6%, respectively), difficulty with relationships (28.1% versus 14.3%, respectively), and sleep problems (44.6% versus 28.0%, respectively). In addition, those with longer deployments (3-4 weeks and longer) were more likely to report anxiety and/or depression and sleep problems (see Table 1 for details). Those who received behavioral health training before deployment were less likely to report anxiety and/or depression (27.8% versus 42.9%, respectively). Difficulty with relationships was reported more often among those who received support after the event (43.3% versus 21.2%, respectively). Lastly, those who were aware of behavioral health guidelines were less likely to report sleep problems (28.6% versus 48.0%, respectively). Awareness of behavioral health guidelines was not significantly different by disaster location (data not shown). There were no characteristics associated with mood swings or suicidal thoughts.
Supplementary Table 1 shows behavioral health outcomes stratified by during versus after the disaster response. Of note, those whodid fieldwork were more likely to experience anxiety and/or depression (30.8% versus 16.0%, respectively), sleep problems (13.1% versus 5.0%, respectively), and mood swings (14.0% versus 5.0%, respectively) after the event compared to those whodid not do fieldwork. There were no differences in behavioral health outcomes in those who did fieldwork versus those who did not during the event. Those who were aware of behavioral health guidelines were less likely to report anxiety/and or depression (10.1% versus 31.2%, respectively), difficulty with personal relationships (6.7% versus 18.8%, respectively), sleep problems (censored data), and mood swings (censored data) after the event compared to those who were unaware of guidelines.
Behavioral Health Outcomes During and/or After the Disaster Event by Type of Fieldwork
Among those who were involved with depopulation, anxiety and/or depression (66.7% versus 36.7%, respectively) and sleep problems (58.1% versus 36.0%, respectively) were higher compared to those who were not involved in depopulation (Table 2). Those who were involved with sheltering had lower rates of anxiety and/or depression (24.0% versus 51.2%, respectively), sleep problems (censored data), and mood swings (censored data) compared to those not involved with sheltering. Additionally, participants involved in treatment had lower rates of anxiety/depression (32.5% versus 52.2%, respectively) compared to those not involved in treatment.
Table 2. Behavioral health outcomes stratified by fieldwork type during and/or after a disaster response among veterinarians (n = 113) 1

1 Bolded values indicate statistical significance of an association between that variable (row) and behavioral health outcome (column) at P ≤ 0.05. Comparisons of each variable with each behavioral health outcome were conducted using Chi-square analyses. Fisher’s exact test was used when exact counts <5.
2 Anxiety/restlessness/lack of concentration and/or depression.
3 Difficulty with personal and/or professional relationships.
4 Trouble sleeping and/or dreaming/nightmares/flashbacks.
5 Indicates censored data due to small cell size.
Supplementary Table 2 shows behavioral health outcomes stratified by fieldwork type and time point (during and after the event). Anxiety and/or depression werehigher among those involved with carcass management (50.0% versus 24.4%, respectively) and quarantine (50.0% versus 25.6%, respectively) during the event compared to those not involved in carcass management and quarantine, respectively. Conversely, participants involved in sheltering had lower rates of anxiety and/or depression during the event (censored data) compared to those not involved with sheltering. Those involved with depopulation were more likely to have anxiety and/or depression after the event (50.0% versus 23.4%, respectively) compared to those not involved in depopulation. In comparison, those involved with treatment had lower levels of anxiety and/or depression after the event (18.4% versus 37.7%, respectively).
Helpfulness of Behavioral Health Support During and After a Disaster Event
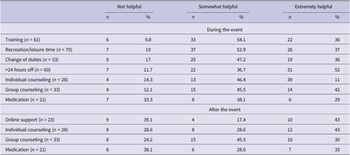
The most common support received during an event was recreation/leisure time (n = 70), followed by training (n = 61), and getting more than 24 hours off (n = 60) (Table 3). The most helpful support received during an event was getting more than 24 hours off, with 51.7% reporting that this was extremely helpful and 36.7% reporting that this was somewhat helpful. Group counseling was also highly rated with 42.4% reporting that it was extremely helpful and 45.5% reporting that it was somewhat helpful. For help after the event, the most helpful support was not clear, although the average rating of individual counseling (1=Not helpful, 2=Somewhat helpful, 3=Extremely helpful) was slightly higher (mean[sd]; 2.14[0.8]) compared to group counseling (2.06[0.7]), online support (2.04[0.9]), and medication (1.95[0.9]).
Table 3. Helpfulness of behavioral health support during and after a disaster response in veterinarians

Limitations
There are several limitations to the present study. The severity of behavioral health outcomes was not assessed, and clear definitions of each outcome in the survey were not described to the participants. Future studies should use validated survey instruments to evaluate behavioral and mental health in this population. In addition, the study may be subject to volunteer bias, meaning those who participated are different from the general population. For example, those who have experienced negative mental health outcomes may be more likely to respond. Lastly, the survey was cross-sectional in nature and survey responses may be subject to recall bias. Some of the disaster responses reported in the survey by participants occurred years earlier, so they may not have accurately recalled their behavioral health state during that time. Future studies could consider conducting longitudinal studies that span before, during, and after a disaster event to better ascertain causality and reduce the risk of recall bias. Still, this study addresses a gap in the literature as very few studies have assessed behavioral health risk factors in veterinarians. Future studies should consider a longitudinal study design that utilizes validated survey instruments to measure behavioral health.
Discussion
In this study, multiple risk factors for adverse behavioral health outcomes in veterinarians involved with disaster response were identified, including increased number of disaster events experienced, increased length of deployment, lack of pre-deployment training, being involved in depopulation, and lack of awareness of behavioral health guidelines. Additionally, the study identified types of behavioral health support the respondents viewed as most beneficial during the disaster event, including getting more than 24 hours off and group counseling.
Those deployed more than 1 time and deployed for a longer time (at least 3 weeks) were at higher risk of adverse behavioral health problems. In addition, respondents rated having more than 24 hours off as a very helpful form of support during a disaster event. Out of 198 free text responses to the question “What behavioral health support do you believe veterinarians need BEFORE, DURING, and/or AFTER participating in a disaster event?”, 29 mentioned time-off and breaks between deployments.Reference Vroegindewey and Kertis 12 These findings are similar to studies among human medicine disaster respondents.Reference Brooks, Dunn and Sage 14 In a simulated disaster-training exercise, sleep quantity and cognitive effectiveness were decreased after 3-5 days.Reference James, Smart and Odom-Maryon 15 Burgess, 2007Reference Burgess 16 created recommendations for 24-hour emergency coverage based on human physiology and the circadian rhythm, including avoiding scheduling key individuals on a 24-hour basis, shifting to 8-hour shifts instead of 12-hour shifts, and the inclusion of recuperative days. In addition, there is a need to increase the veterinary disaster workforce, starting with veterinary training in veterinary curricula and continuing education,Reference Dunning, Martin and Tickel 17 so that deployment times and time off can be better managed.
Similar to findings in a systematic review in medical responders, lack of training prior to a disaster event was associated with adverse mental health events.Reference Naushad, Bierens and Nishan 7 In a study on hurricane response, the Florida Center for Public Health Preparedness (FCPHP) tested disaster mental health training and reported that the majority of respondents found that the training gave them more knowledge of mental health and provided them with useful mental health skills.Reference Reid, Ruzycki and Haney 18 In the current study, those who received behavioral health training before deployment were less likely to report anxiety and/or depression. Out of 198 free-text responses to the question “What behavioral health support do you believe veterinarians need BEFORE, DURING, and/or AFTER participating in a disaster event?”, 86 mentioned behavioral health training.Reference Vroegindewey and Kertis 12 This supports the previous recommendation for WOAH, with the United Nations Agency for Food and Agriculture (UNFAO), to develop guidelines and standards for behavioral health training.Reference Vroegindewey and Kertis 12
Depopulation was associated with adverse behavioral health outcomes, including anxiety, depression, and sleep problems. These findings are similar to findings in previous studies conducted among veterinarians, which found that veterinarians involved in de-population of swine during the COVID-19 pandemic had high levels of burnout and needed additional support.Reference Baysinger and Kogan 10 , Reference Bussolari, Packman and Currin-McCulloch 11 Of note, in the current study, those who were involved with depopulation tended to experience greater adverse behavioral health events after the event, indicating that continued support is necessary for these individuals. Conversely, those involved with sheltering and treatment had lower risk of behavioral health outcomes.
In agreement with qualitative findings from this survey previously reported,Reference Vroegindewey and Kertis 12 participants thought counseling was an important aspect of behavioral health support. In the current study, participants tended to rate group and individual counseling higher than some other forms of support, including medication. Additionally, out of 198 free text responses for the question “What behavioral health support do you believe veterinarians need BEFORE, DURING, and/or AFTER participating in a disaster event?”, 68 mentioned counseling, 14 mentioned mentoring and peer support, 32 mentioned check-ins, and 36 mentioned de-briefing.Reference Vroegindewey and Kertis 12 Winders et al. 2021Reference Winders, Bustamante and Garbern 19 performed a systematic review of interventions for first responders to treat mental health effects of a disaster response and found that psychological interventions likely positively impact mental health outcomes post-disaster. There is a need to develop and implement training programs for counseling psychologists to treat trauma related to disaster response.Reference Bowman and Roysircar 20
Conclusions
Multiple risk factors for adverse behavioral health outcomes were identified, including responding to more than 1 event, longer deployments, being involved with depopulation, carcass management, or quarantine, and lack of behavioral health training prior to deployment. The majority of participants (51.7%) reported that adequate time-off was extremely helpful and 36.7% reported that it was somewhat helpful. Group counseling was rated as extremely helpful by 42.4% of respondents and somewhat helpful by 45.5% of respondents. These results can assist veterinary response leadership to evaluate their current standard operating procedures and response plans to incorporate behavioral health resilience training and support and adequate time-off across the entire spectrum of the disaster management cycle. Interventions to alleviate behavioral health outcomes should be developed to target those in high-risk roles, such as those involved in depopulation, carcass management, and quarantine. Future studies should consider longitudinal designs that use validated instruments to address limitations of the current design.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/dmp.2024.257.
Author contribution
Gary Vroegindewey was involved in the conception and design of the study, acquisition of data, and drafting and revising the manuscript. Lauren Wisnieski was involved in designing and conducting the statistical analysis and revising the manuscript. J Lee Jenkins was involved as a subject matter expert and was involved in designing the statistical analysis and revising the manuscript.
Competing interest
The authors declare none.