The local public health agency (LPHA) workforce is at the center of the public health emergency preparedness systemReference Altevogt, Pope, Hill and Shine 1 and is integral to locally driven disaster recovery efforts. The intent of this article is to begin laying the groundwork for a research agenda that aims to investigate threat- and efficacy-oriented perceptions among LPHA workers affected by disaster. The article responds to a need for rigorous, mixed-methods research that applies a behavioral model to qualitatively and quantitatively characterize the operational challenges encountered by LPHA workers in the recovery phase; to understand the relationship of efficacy and threat perceptions to LPHA workers’ willingness and ability to contribute to recovery efforts; and to uncover methods to improve overall capacity of LPHAs to support community-level disaster-recovery services. This article is not intended to be a formal description of the research per se, but rather to conceptualize its intent, overarching approach, and relevant potential for addressing critical existing knowledge gaps regarding the disaster recovery perspectives of LPHAs.
Lpha Workforce Role In Disaster Recovery
LPHAs are a vital component of the local community infrastructure throughout the disaster life cycle. This notion is in keeping with the maxim that “all disasters begin locally”Reference Taylor and Chaffee 2 and is supported by the fundamental National Incident Management System concept of a locally driven approach to disaster management. 3 Indeed, as characterized by the Federal Emergency Management Agency, “recovery can be successful only when it is locally driven and the community takes ownership of the process. Recovery assistance should supplement local efforts and build local capacity as needed.” 4
Following a disaster, LPHAs have primary responsibility for the health of the community and are involved in a spectrum of activities that span the short-term (days) and long-term (months to years) phases of disaster recovery. 5 Anticipated recovery responsibilities include ensuring the continuity of health care services, monitoring environmental infrastructure, assessing and providing referrals to meet the needs of vulnerable populations, initiating surveillance programs, issuing health advisories and continuing open communication with the public, and allocating resources to match public health needs.Reference Landesman 6
In the last 4 years, 55% of LPHAs have had to address at least one event within the all-hazards continuum. However, more than 46,000 state and local LPHA jobs have been eliminated since 2008, representing nearly 21% of the total state and LPHA workforce. 7 , 8 Fewer overall public health staff equates to fewer staff to address emergencies, regardless of whether these workers have been trained as emergency preparedness professionals. Exacerbating this issue, the overall federal funding for emergency preparedness dropped 44% from 2010 to 2013, 9 and from 2011 to 2012, the percentage of LPHAs with an emergency preparedness program fell from 23% to just 15%. 10 These budget cuts have had significant impacts on the quantity and quality of training, exercises, and supplies available in LPHAs. 9
These losses have occurred concurrently with an increase in the frequency and severity of disasters, defined in this article as meeting at least one of the following criteria: 10 or more people reported killed, 100 or more people reported injured, a declaration of a state of emergency, or a call for international assistance. 11 Globally, the number of natural disasters reported has increased steadily since 1960, as has the number of people reported as affected. 11 In some countries, disaster reporting may have political or economic benefits, so it is possible that a proportion of this increase is due simply to less stringent definitions of disaster or a greater likelihood to report them. However, while better reporting and media coverage may artificially inflate measures of disaster incidence, leading experts estimate that at least two-thirds of the growth is real and due to the rise in hydro-meteorological disasters.Reference Than 12 From 2000 to 2009, for example, there were 3 times as many natural disasters as there were between 1980 and 1989. 13 In the United States, 7 of the top 10 disasters affecting the greatest number of people occurred in this decade. 14 The increasing severity of disaster impacts has been largely influenced by the increase in magnitude of the extreme weather events themselves, as well as an increase in exposure and vulnerability of human populations. Settlement patterns, urbanization, and changes in socioeconomic conditions have all influenced observed trends in exposure and vulnerability to climate extremes. 15
Lpha Workers and Disaster Recovery: Operational Research Gaps
While there is most certainly a role for LPHAs in disaster recovery, only in the last decade have national (US) policies begun to formally define this role, 16 enumerate standards for state and local planning within public health agencies and systems, 17 and advocate for support to better integrate LPHAs and their services into disaster planning. 18 , 19 Consequently, while much work has been done to increase the capacity and capability of LPHAs to support local disaster services, little is actually known about how confident LPHA workers are in their ability to contribute to disaster cycle services, particularly in the recovery phase of a disaster.
For example, although the National Disaster Recovery Framework (the Framework) was released in September 2011 as a guide to enable recovery support to disaster-affected communities, there has been a distinct lack of research on LPHAs’ operational familiarity with this tool. The Framework was designed as a flexible strategy for scaling recovery and enabling disaster recovery managers to operate in a unified and collaborative manner, 5 and it introduces 6 recovery support functions (one of which is Health and Social Services Recovery) and 3 specific job roles (at the federal, state or tribal, and local levels) to advance recovery considerations and facilitate collaboration among agencies. 5 Although the Health and Social Services Recovery Support Function specifically includes public health, the Framework is in the early stages of implementation. As it is being applied by federal agencies, and adopted by state and local agencies, there is a timely opportunity to gather impressions from LPHA workers about how the Framework is understood and implemented and how it may influence LPHA workers’ willingness and ability to participate in recovery activities.
Similarly, the National Health Security Strategy and the Public Health Preparedness (PHP) Capabilities each clearly identify the recovery phase of disaster as an area of focus. 17 , 18 , However, like the Framework document, the PHP Capabilities are somewhat newly released, and in the early stages of implementation. Furthermore, Public Health Emergency Preparedness cooperative-agreement grantees that use the PHP Capabilities for planning purposes have recently aligned objectives with Hospital Preparedness Program (HPP) grantees, leaving opportunity for improved understanding of how public and clinical health can better interface to support recovery planning. 20
Lpha Workers and Disaster Recovery: Efficacy-Oriented Research Gaps
Recovery systems require empowered and competent people in addition to materials and plans. A critical component of resilience is an affected individual’s (and by extension, the population’s) self-efficacy. The concept of self-efficacy is defined as one’s perceived ability to influence events that affect their lives.Reference Bandura 21 Because LPHA workers are at the core of local community recovery, it is important that their resilience and self-efficacy be enhanced so that they can confidently lead and participate in the recovery of the disaster-affected health sector. Despite this reality, the LPHA workforce’s perceptions of efficacy toward disaster-recovery activities remain under-examined and poorly understood.
Self-efficacy is a well-established concept in the psychological literature. Indeed, evidence from controlled experiments and field studies has verified that self-efficacy—the belief in one’s own ability to meaningfully contribute to an effort/situation—is the most important determinant of the behaviors that people choose to exhibit and how much they persevere in the face of obstacles and challenges.Reference Bandura 22 - Reference Bandura and Locke 24 A growing body of research has pointed to LPHA workers’ perceptions of self-efficacy as a leading affective modifier of this professional cohort’s self-reported willingness to report to work during disaster response scenarios.Reference Barnett, Balicer and Thompson 25 , Reference Barnett, Thompson and Errett 26 Of major importance, efficacy perceptions reflect actual behaviors and dispositions.Reference Bandura 21 , Reference Witte 27 - Reference Bandura 29 Specifically, self-efficacyReference Bandura 21 and “response efficacy” (ie, the perception that one’s behavior matters in a broader context)Reference Witte 27 have been found to correlate with positive adaptive behaviors and attitudes in the face of novel risks and challenges.Reference Witte 27 Self-efficacy is not one’s perception of skill; rather, it is what one believes they can do with their skills under a particular set of conditions.Reference Snyder and Lopez 30 The limited disaster literature on efficacy perceptions has focused on self-efficacy as a determinant of mental and behavioral healthReference Murphy, Norbeck and Weinert 31 and post-traumatic recovery after a disaster.Reference Benight, Ironson and Klebe 32 - Reference Sumer, Karanci, Berument and Gunes 34 Similar research has identified correlations between optimism and superior performance in adverse situations.Reference Bronson, Faircloth and Valentine 35
In this article, disaster recovery is defined in accordance with the Federal Emergency Management Agency’s Framework as follows: “[R]ecovery encompasses more than the restoration of a community’s physical structures to its pre-disaster conditions. Of equal importance is providing a continuum of care to meet the needs of the affected community members who have experienced the hardships of financial, emotional or physical impacts as well as positioning the community to meet the needs of the future.” 5 Of significance, recovery is a continuum that extends from disaster onset through the response phase and into renewed mitigation and preparedness efforts. 5 Therefore, it is reasonable to hypothesize that worker efficacy is essential not only in response, but throughout the entirety of the recovery period as well. While the role of worker self-efficacy is well supported in the disaster response phase, there is a notable lack of research evidence surrounding the LPHA workforce’s perceptions of efficacy in the context of disaster-recovery processes for any disaster. A variety of differences suggest that findings in the response phase may not be generalizable to the recovery phase. First, the individuals with roles in disaster response may not be the same individuals playing a role in disaster recovery; second, the activities to be performed in disaster response 36 differ from those in disaster recovery 5 ; third, the duration of the response phase is typically days to weeks, whereas the recovery phase can last months to years; and fourth, the environment during the response phase may be much different than that during the recovery phase.
A Behavioral Framework for Examining Lpha Workers’ Disaster Recovery Perceptions: The Extended Parallel Process Model
Behavioral models have historically been underutilized in disaster research,Reference Chaffee 37 including disaster-recovery research. To that end, recent studiesReference Barnett, Balicer and Thompson 25 , Reference Barnett, Thompson and Errett 26 , Reference Barnett, Errett and Rutkow 38 suggest the promise of applying an efficacy-oriented model, Witte’s Extended Parallel Process Model (EPPM), for providing relevant behavioral insights into LPHA workers’ perceptions toward performing disaster roles. The EPPM (Figure 1) describes adaptive behavior in the face of an unknown risk, and has been refined and evaluated in the last two decades.Reference Barnett, Balicer and Thompson 25 , Reference Barnett, Balicer and Thompson 39 The model predicts that, in the face of uncertain risk, people are more apt to engage in proactive behaviors if they perceive the threat associated with a hazard as legitimate and if they believe they can implement a desired intervention efficaciously. Although the model was initially developed to explain individual behavior in response to received messages,Reference Bandura 21 it has since been used to analyze collective behavior as well.Reference Witte and Allen 40
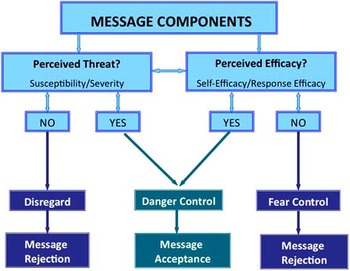
FIGURE 1 The Extended Parallel Process Model. Figure adapted from Barnett et al, 2009.Reference Barnett, Balicer and Thompson 25
Figure 1 depicts how high levels of perceived threat, when coupled with high levels of perceived efficacy, can spur motivation toward positive adaptive behaviors. The first appraisal (threat appraisal) has two components: susceptibility and severity. If the message recipient perceives the hazard to be improbable (low susceptibility) or of negligible consequence (low severity), messages encouraging a desired protection-oriented response or behavior will be rejected. If, however, the message recipient perceives both high severity and high susceptibility in the threat appraisal, he or she will go on to process the message’s content for efficacy (efficacy appraisal). The efficacy appraisal also contains two components: self-efficacy and response efficacy. If the message recipient does not find the message’s targeted behavior to be achievable (low self-efficacy) or efficacious (low response efficacy), the message recipient will reject the message and often engage in responses such as denial and avoidance in order to manage fear (described as “fear control” in the EPPM). If the efficacy appraisal and the threat appraisal are both endorsed, message acceptance will result and the recipient will engage in the message’s intended protective behavior-change outcomes by taking steps to minimize personal risk against the hazard (described as “danger control” in the EPPM).
The EPPM contains attitudinal elements that are relevant to evaluating the public health system’s recovery-phase perceptions. The efficacy components of the model comprise self-efficacy, which augments effective behavior,Reference Bandura 29 , Reference Smith, Ferrara and Witte 41 and response efficacy, or the broader importance of one’s role to overall agency initiatives (ie, “What I do matters”).Reference Barnett, Balicer and Thompson 25 , Reference Barnett, Thompson and Errett 26 The threat components of the EPPM allow for analysis of behavior motivation,Reference Bandura 21 as in the case of previous research on pre-event willingness of LPHA workers to respond to disasters.Reference Barnett, Balicer and Thompson 25 , Reference Barnett, Thompson and Errett 26 There is also a robust literature, developed over the course of several decades, that establishes self-efficacy as a predictor of actual behavior.Reference Bandura 29 , Reference Smith, Ferrara and Witte 41 A growing body of disaster research supports this literature, with the finding that self-efficacy within the EPPM framework is one of the most strongly influential modifiers of willingness to respond in a disaster.Reference Barnett, Balicer and Thompson 25 , Reference Barnett, Thompson and Errett 26
Of note, disaster research on the EPPM has, to date, exclusively focused on LPHA workers’ disaster response-phase perceptions and has uncovered this model’s strong relevance to understanding perceptual determinants of LPHA workers’ disaster response-phase behaviors. However, this prior research, coupled with the features of the EPPM itself, also suggests the model’s significant potential as an analytic framework for understanding LPHA workers’ perceptions and motivations toward fulfilling their disaster recovery-phase role expectations. In the context of disaster recovery, LPHA workers must address a variety of threats to the communities they serve, ranging from ongoing surveillance to environmental contamination and ongoing chronic psychological sequelae. The EPPM framework predicts that if an LPHA worker perceives these recovery considerations to be legitimately concerning, they will be motivated to engage in desirable behaviors when coupled with a sense of efficacy. Hence, the EPPM posits that a worker fitting a “concerned” (high threat) and “confident” (high efficacy) profile will be most apt to treat public health recovery activities as a high priority and engage in them accordingly.
Future Research and Conclusions
The information presented in this article highlights the need to better understand disaster recovery from the perspective of the LPHA workforce and to investigate opportunities for improved LPHA workforce efficacy through public health intervention. The field remains markedly short on research in these areas; application of the concepts and strategies denoted above can begin to fill this critical research gap.
The timeliness of such a research agenda is clear. Only in the last decade has national policy defined the role of public health in disaster recovery, directly added public health services to the disaster planning efforts, and enumerated standards for public health service delivery in crisis. Consequently, little is known about the confidence of LPHA workers in carrying out these responsibilities. Do LPHA workers know their role in disaster recovery? Do they use national policies as guidance and understand how to operationalize the components of these policies in the disaster recovery context? Are the enumerated PHP capabilities useful for improving the understanding of local public health’s role in disaster recovery? These questions begin to elucidate some of the operational research gaps related to LPHA workers’ roles in disaster recovery.
There are also related research gaps in efficacy-related inquiry during disaster recovery. Empowered people are essential to operational and effective recovery systems. As supported in the psychological and disaster response literature, high self-efficacy and response efficacy lead to more empowered and action-oriented people. However, the barriers and contributors to LPHA workers’ perceptions of efficacy are understudied, particularly in the recovery phase of disaster. Although research indicates that self-efficacy and response efficacy improve worker motivation to contribute to disaster response activities, these roles, and the people who are expected to perform them, may differ quite significantly in the recovery phase. Are self-efficacy and response-efficacy perceptions different in the response and recovery phases of disaster? How can we improve local public health worker efficacy during the disaster recovery phase? What are facilitators and barriers to contributing to local disaster recovery services?
Further research is needed to begin to answer these questions and to better understand the motivations of LPHA workers toward disaster recovery efforts that can extend months to years following a catastrophic event. Toward that end, the authors have conceptualized the timely relevance of a research agenda by which a threat- and efficacy-oriented behavioral model framework (EPPM) can be used to better understand disaster recovery from the perspective of the LPHA workforce. Specifically, the EPPM can underpin qualitative (focus group–based) and quantitative (survey-based) mixed-methods assessments of operational and attitudinal facilitators and barriers among LPHA workers regarding disaster recovery. Such EPPM-based assessments can then inform processes and procedures to increase this workforce’s efficacy perceptions toward disaster recovery and yield targeted educational curricular interventions to bolster recovery-based self-efficacy and response efficacy in LPHAs. These research-informed outcomes can thus optimize the LPHA workforce’s role as a critical component of community resilience in present and future disaster recovery contexts.
Acknowledgment
This work was supported by Centers for Disease Control and Prevention Cooperative Agreement 1U01TP000576-01. The authors also wish to acknowledge the Johns Hopkins Center for Public Health Preparedness (PERRC; CDC/grant 1P01tP00288-01; grant 104264). The funders had no role in the decision to publish or in manuscript preparation.
The views expressed are those of the authors and do not reflect the official policy or position of the Uniformed Services University of the Health Sciences, the Department of Defense, or the United States Government.



