High rates of suicide are common among homeless youth, with research indicating that over 30% of homeless youth report a lifetime suicide attempt (Yoder et al., Reference Yoder, Whitbeck and Hoyt2010). This is considerably higher when compared to the rate of the general youth population, 13.95% (Centers for Disease Control and Prevention, 2020). Suicidal ideation is one of the most potent predictors for suicidal behavior and completed suicide (Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019). Chronic elevated suicidal ideation is associated with an increased likelihood of future suicide attempts (Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019), and warrants special research and clinical attention. In particular, more research is needed to understand the heterogeneity of the process of change as a result of suicide intervention among youth populations (Musci et al., Reference Musci, Kharrazi, Wilson, Susukida, Gharghabi, Zhang, Wissow, Robinson and Wilcox2018).
In the present study, we examined the heterogeneous trajectories of homeless youth experiencing suicidal ideation in a randomized controlled intervention study. This investigation is informed by a framework for heterogenous treatment effects (Varadhan et al., Reference Varadhan, Segal, Boyd, Wu and Weiss2013), in which intervention effects are perceived as changing in multiple pathways that reflect the dynamic interplay between pretreatment risk factors and received intervention. Adopting such a framework, the goals of our study were threefold. First, we modeled the change process of suicidal ideation using a person-centered approach. A person-centered approach captures changes across time and identifies subgroups of youth who follow distinct trajectories. This approach is well-suited towards understanding heterogeneous treatment effects and differential treatment responses in youth (Varadhan et al., Reference Varadhan, Segal, Boyd, Wu and Weiss2013). Second, we sought to evaluate factors that channel youth into different change trajectories to identify risk factors precipitating less satisfactory treatment responses. Third, we examined the associations between trajectories of suicidal ideation and suicide-related outcomes at 9-month post-baseline. This increases our understanding of treatment effectiveness post-intervention in each subgroup.
Heterogeneous trajectories of suicidal ideation
Researchers have paid increasing attention towards youth suicidality due to its dire public health consequences (Musci et al., Reference Musci, Kharrazi, Wilson, Susukida, Gharghabi, Zhang, Wissow, Robinson and Wilcox2018). Despite the majority of cross-sectional research focused on youth suicidality, a small body of research has emerged capturing the heterogeneous, longitudinal changes in youth suicidal ideation. Indeed, change in suicidal ideation is likely to follow heterogeneous patterns, as opposed to a singular trajectory (Czyz & King, Reference Czyz and King2015). The heterogeneous trajectories of suicidal ideation are observed across diverse populations including military service members (Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019), patients with psychosis (Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016), and clinical and community samples of adolescents (Czyz & King, Reference Czyz and King2015; Rueter et al., Reference Rueter, Holm, McGeorge and Conger2008).
Even though research substantiates the heterogeneous trajectories of suicidal ideation, only a few studies have examined these trajectories in the context of therapeutic interventions. Following a group of adolescents hospitalized due to acute suicidal ideation over a year, Czyz and King (Reference Czyz and King2015) identified three distinct trajectory groups including a subclinical group, an elevated and rapidly declining ideation group, and a chronically elevated ideation group. Wolff et al. (Reference Wolff, Davis, Liu, Cha, Cheek, Nestor, Frazier, Schaffer and Spirito2018) studied hospitalized adolescents over 6 months and also observed three groups with chronic, declining, or subclinical suicidal ideation levels. Another study described three trajectory groups of suicidal ideation among adult patients during 2 years after the onset of psychosis: low-decreasing, frequent-stable, and frequent-increasing, with about 40% of patients experienced frequent suicidal ideation that persisted or increased (Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016). Finally, over 13 years, Goldston et al. (Reference Goldston, Erkanli, Daniel, Heilbron, Weller and Doyle2016) followed adolescents discharged from hospitalization into their adulthood, assessed their suicidal ideation and behaviors, and found four groups, namely increasing risk, highest overall risk, decreasing risk, and low risk groups. These studies support further investigation into heterogeneous change processes during and following treatments for suicide.
Additionally, little is known about whether suicide interventions affect the multifinality of suicidal, homeless youth, showing similar, heterogeneous trajectories of suicidal ideation to those found in adolescent and adult samples. Homeless youth is a vulnerable population who experience multiple forms of developmental risks that make them distinct from their housed peers (Slesnick et al., Reference Slesnick, Feng, Guo, Brakenhoff, Carmona, Murnan, Cash and McRee2016a). Homeless youth experience high rates of mental health problems (69%), substance abuse (70%–95%), and victimization experiences (83%; Bender et al., Reference Bender, Brown, Thompson, Ferguson and Langenderfer2015; Chen et al., Reference Chen, Thrane, Whitbeck and Johnson2006; Martijn & Sharpe, Reference Martijn and Sharpe2006; Morton et al., Reference Morton, Dworsky, Samuels and Patel2018). Homeless youth often do not complete a high school education and are involved with the foster care or juvenile systems (Morton et al., Reference Morton, Dworsky, Samuels and Patel2018). Additionally, important executive functions such as inhibition and planning skills are still developing in early adulthood. Without consistent, caring homes, homeless youth are at greater biological risks of engaging in high-risk behaviors (Fry et al., Reference Fry, Langley and Shelton2020). Together, multiple threats impede homeless youth’s development, including unmet basic needs, untreated mental health issues, substance use, sexually transmitted diseases including HIV, abuse and victimization, and suicide. Due to multiple risks and undermined cognitive processing skills, it is unclear how homeless youth would respond to treatment similarly from other adolescent and adult samples. This is especially critical in suicide treatments that involve high-level cognitive functioning, such as Cognitive Therapy for Suicide Prevention (CTSP; Wenzel et al., Reference Wenzel, Brown and Beck2009). Further, information on psychosocial and demographic factors predicting distinct suicidal ideation trajectories remains insufficient, which would help identify the most vulnerable homeless youth at risk for suicide and can be thus used to facilitate personalized interventions.
Predictors characterizing trajectory groups of suicidal ideation
Etiological theories on suicidality usually emphasize a constellation of factors that initiate or maintain suicidality (Joiner, Reference Joiner2005; Nock et al., Reference Nock, Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). These factors may include mental health risk factors and demographic predictors. Indeed, homeless youth generally report high levels of mental health challenges (Thompson et al., Reference Thompson, Rew, Barczyk, McCoy and Mi-Sedhi2009), substance use (Slesnick et al., Reference Slesnick, Feng, Guo, Brakenhoff, Carmona, Murnan, Cash and McRee2016a), and trauma exposure (e.g., violence and childhood abuse; Cauce et al., Reference Cauce, Paradise, Ginzler, Embry, Morgan, Lohr and Theofelis2000; Slesnick et al., Reference Slesnick, Zhang and Brakenhoff2016b). In the current study, we included factors that are most pertinent to homeless youth’s suicidality, as well as factors associated with treatment in order to better understand treatment response.
Depressive symptoms are commonly associated with elevated suicidal ideation. Depressed adolescents report a six-fold greater likelihood of suicide attempts (Nock et al., Reference Nock, Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). Substance use is also one of the primary factors contributing to increased suicide risk in adolescence; substance using adolescents are 3–20 times more likely to report suicidal ideation (Esposito-Smythers & Spirito, Reference Esposito-Smythers and Spirito2004; Hallfors et al., Reference Hallfors, Waller, Ford, Halpern, Brodish and Iritani2004). Childhood abuse history, including both physical and sexual abuse, is associated with higher suicidal ideation among youth (Miller & Esposito-Smythers, Reference Miller and Esposito-Smythers2013). In addition, we included demographic information such as youth’s sex, as female adolescents are more likely to report suicidal ideation and behaviors (Hallfors et al., Reference Hallfors, Waller, Ford, Halpern, Brodish and Iritani2004; Nock et al., Reference Nock, Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). We also included information on race, as White, non-Hispanic youth reported higher odds of suicidal thoughts and attempts compared to African American youth (CDC, 2020; Hallfors et al., Reference Hallfors, Waller, Ford, Halpern, Brodish and Iritani2004; Nock et al., Reference Nock, Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). Meanwhile, a higher level of education is a protective factor against suicidal ideation among adults (Johnston et al., Reference Johnston, Pirkis and Burgess2009). We also assessed predictors specifically pertaining to youth’s homeless experience, the length of lifetime homelessness, as it is a significant predictor to homeless youth’s mental health (Cauce et al., Reference Cauce, Paradise, Ginzler, Embry, Morgan, Lohr and Theofelis2000; Slesnick et al., Reference Slesnick, Feng, Guo, Brakenhoff, Carmona, Murnan, Cash and McRee2016a). Finally, we included treatment attendance of both CTSP and treatment-as-usual (TAU) sessions. Attending more CTSP sessions reduced homeless youth’s suicidal ideation (Slesnick et al., Reference Slesnick, Zhang, Feng, Wu, Walsh and Granello2020).
Suicide-related psychosocial outcomes
The third goal of the current study is to assess suicide-related outcomes associated with different change trajectories of suicidal ideation. Previous studies have indicated that people in frequent, stable, and/or chronic suicidal ideation trajectory groups have the highest risk for future suicide attempts (e.g., Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019; Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016). In the current study, we consider it crucial to examine suicide-related factors post-intervention, which may feed into future suicidality. Indeed, suicide-related psychosocial risk or protective factors may also change during the intervention, along with the change of suicidal ideation. Effective interventions may reduce the intensity of risk factors (e.g., feelings of hopelessness or a negative world view) and promote protective factors (e.g., reaching out for help from family and friends), and thus prevent the transition from suicidal ideation to attempts. Thus, this study contributes to the current literature by providing evidence on post-treatment suicide-related factors among different trajectory groups of youth. A better understanding of these patterns will help retarget future treatment towards factors that barely changed, thus improving treatment efficacy.
Cognitive distortions
As one of the most pernicious factors contributing to suicide risk among adults, cognitive distortions are defined as distorted information processing that generates maladaptive responses to stressful situations (Jager-Hyman et al., Reference Jager-Hyman, Cunningham, Wenzel, Mattei, Brown and Beck2014). These distortions may manifest as negative views of self, the world, and the future (Miller et al., Reference Miller, Williams, Day and Esposito-Smythers2017), cognitive rigidity, dichotomous thinking, overgeneralization, and selective abstraction (Jager-Hyman et al., Reference Jager-Hyman, Cunningham, Wenzel, Mattei, Brown and Beck2014).
Thwarted belongingness and perceived burdensomeness
The interpersonal–psychological theory posits that the simultaneous presence of thwarted belongingness and perceived burdensomeness contributes to suicidal thoughts (Joiner, Reference Joiner2005; Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). Although both perceived burdensomeness and thwarted belongness are positively associated with suicidal ideation (e.g., Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a; Reference Van Orden, Witte, James, Castro, Gordon, Braithwaite, Hollar and Joiner2008b), perceived burdensomeness is a particularly strong predictor of suicidal ideation across a variety of youth and adult populations (Chu et al., Reference Chu, Walker, Stanley, Hirsch, Greenberg, Rudd and Joiner2018), including homeless youth (Zhang et al., Reference Zhang, Wu and Slesnick2021).
Acquired capacity for suicide
Suicidal ideation alone does not lead to suicidal behavior. According to the interpersonal–psychological theory (Joiner, Reference Joiner2005), in addition to suicidal ideation, individuals must have the capability to enact lethal injury to engage in suicidal behavior. That is, the presence of thwarted belongingness, perceived burdensomeness, and acquired capability together contributes elevated rates of suicide attempts and death by suicide among adults (Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). Capability alone did not predict clinician-rated suicide risk without the presence of perceived burdensomeness (Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a).
Hopelessness
The feeling of hopelessness has also been identified as a predictor of suicidal behavior (Brausch & Gutierrez, Reference Brausch and Gutierrez2010; Brown et al., Reference Brown, Beck, Steer and Grisham2000). For example, Thompson et al. (Reference Thompson, Mazza, Herting, Randell and Eggert2005) found that hopelessness directly affected suicidal behavior among teens.
Distress tolerance
Youth’s ability to tolerate environmental and psychological stressors is likely to contribute to their suicidal behavior (Anestis et al., Reference Anestis, Bagge, Tull and Joiner2011). Adolescents and adults who have low distress tolerance will engage in maladaptive behaviors, including self-harm and suicide, as a way to avoid unpleasant emotions (Chapman et al., Reference Chapman, Gratz and Brown2006; Nock & Mendes, Reference Nock and Mendes2008).
Impulsivity
Individuals who attempted suicide generally have higher impulsivity than peers without suicide attempts (Michaelis et al., Reference Michaelis, Goldberg, Davis, Singer, Garno and Wenze2004). This is because individuals who attempt suicide may have difficulty controlling impulsive behaviors when feeling distressed (Bornovalova et al., Reference Bornovalova, Tull, Gratz, Levy and Lejuez2011).
Social problem solving
Social problem solving refers to cognitive, emotional, and behavioral coping responses to stressful situations (D’Zurilla & Nezu, Reference D’Zurilla and Nezu1990). It has been linked to decreased suicidal ideation among adult samples (Ghahramanlou-Holloway et al., Reference Ghahramanlou-Holloway, Bhar, Brown, Olsen and Beck2012; Wenzel et al., Reference Wenzel, Brown and Beck2009).
Social network
Social connections with family and friends are related to fewer suicidal thoughts and behaviors among homeless youth. Homeless youth, usually running away from home because of abusive family relationships or violence (Cauce et al., Reference Cauce, Paradise, Ginzler, Embry, Morgan, Lohr and Theofelis2000; Slesnick et al., Reference Slesnick, Zhang and Brakenhoff2016b), are likely to perceive less support from their family members. Instead, they often turn to friends and peers for social support (Bao et al., Reference Bao, Whitbeck and Hoyt2000). Peer connection may influence homeless youth’s suicidal behavior both positively and negatively. Affiliation with prosocial peers protects homeless youth from elevated psychological distress (Dang, Reference Dang2014) and depression (Bao et al., Reference Bao, Whitbeck and Hoyt2000), whereas affiliation with deviant peers increases suicide risk (Rice et al., Reference Rice, Kurzban and Ray2012).
The current study
The current study is a secondary analysis of a randomized controlled trial of CTSP among homeless youth who experienced suicidal ideation. In the major outcome analysis, youth’s suicidal ideation decreased in both treatment groups, but those in the group receiving CTSP added on to TAU declined faster, compared to youth receiving TAU alone (Slesnick et al., Reference Slesnick, Zhang, Feng, Wu, Walsh and Granello2020). As both treatment conditions were effective in reducing youth’s suicidal ideation, the current study extended previous findings by investigating the heterogeneous trajectories of suicidal ideation over 9 months in both treatment groups using a person-centered approach, and tested predictors and outcomes of subgroups of youth defined by distinct trajectories.
Consistent with previous studies (e.g., Czyz & King, Reference Czyz and King2015; Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016), we first hypothesized to find heterogenous groups of youth with distinct change trajectories in suicidal ideation over 9 months. Second, we expected that pretreatment mental health, demographic information, and session attendance would characterize youth’s group membership. Third, youth in different subgroups would have different suicide-related outcomes at the 9-month assessment. Similar to Madsen et al. (Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016), we expected to identify youth with a relatively quick reduction of suicidal ideation, as well as ones with relatively persistent ideation. We further expected youth having relatively persistent suicidal ideation to have higher mental health concerns, demographic risk factors, and fewer CTSP sessions, as well as worse outcomes at the 9-month follow-up assessment, compared to their peers who had a relatively quick reduction in suicidal ideation (see the conceptual model of the current study in Figure 1).

Figure 1. The conceptual model of the current study.
Method
Participants
Participants (N = 150) were recruited from a drop-in center for homeless youth in a large midwestern city in the USA. To be eligible for the study, youth had to be experiencing homelessness, between 18 and 24 years old, able to provide informed consent, and score over 16 on the Scale for Suicidal Ideation – Worst Point (SSI-W; Beck et al., Reference Beck, Brown, Steer, Dahlsgaard and Grisham1999). Youth were deemed ineligible if they required hospitalization due to suicidal ideation or showed symptoms of a psychotic disorder as determined by the Structural Clinical Interview for DSM-5 disorders psychotic screening (SCID; First et al., Reference First, Williams, Karg and Spitzer2015). Demographic information is included in Table 1.
Table 1. Demographic characteristics of the current sample

Note
a Possible ranges 0–1.
Procedure
Youth were recruited and screened for eligibility at the drop-in center by trained research assistants. Prescreening generated 225 youth who fell into the age range (18–24), and who met the criteria for homelessness, reported suicidal thoughts, and showed interest in the study. The SCID section on psychosis and the SSI-W were administered to these youth to determine formal eligibility, with 14 youth excluded for low SSI-W scores and another 29 excluded for failing the SCID. Youth who met the study inclusion criteria consented and completed the baseline assessment battery (N = 150). Another 32 youth, although eligible, never finished the baseline assessment due to various reasons (e.g., distractions or interruptions of assessment, having left the center and never returned) and thus were excluded from the study. Ineligible youth were given a care package for their time and continued to receive services at the drop-in center. Any youth determined at imminent risk for suicide were taken to a local hospital for psychiatric evaluation and/or crisis management.
Youth eligible for the study completed a baseline assessment and then were randomly assigned to receive Cognitive Therapy for Suicide Prevention plus treatment as usual (CTSP+TAU; n = 75) or TAU alone (n = 75). There were no between-group differences in demographic characteristics or baseline scores. Licensed therapists employed by the drop-in center provided both interventions, and tracked intervention contact and session completion. All CTSP sessions were completed within 6 months, and TAU sessions were available for 9 months for all participants. Youth received $5 gift cards for each attended CTSP session. Follow-up assessments were completed to evaluate treatment outcomes for all participants at 3 months (89.4% retention), 6 months (86.6%), and 9 months (85.9%) post-baseline, using an intent-to-treat design. Youth received a $40 gift card for the completion of each assessment for compensation. We included the diagram of the intervention study in Figure 2. All study procedures were approved by the Ohio State University Institutional Review Board (study number 2014B0532).

Figure 2. Diagram of the intervention study.
Intervention
Treatment as usual (TAU)
The drop-in center offers a variety of services to meet youth’s basic needs, such as food, toiletries, laundry, shower facilities, recreational activities such as television, games, books, and art, opportunities to socialize and connect with peers, and connection to community resources as needed. The drop-in center also employs two on-site mental health therapists who provide non-directive client-centered therapy as a standard practice for suicide prevention.
Cognitive therapy for suicide prevention (CTSP) + TAU
CTSP is a manualized therapeutic approach that focuses exclusively on suicide prevention (Wenzel et al., Reference Wenzel, Brown and Beck2009) and was added on to TAU. CTSP interventions include assessing suicidal thoughts and behaviors, creating a crisis plan, and teaching cognitive restructuring and behavioral changes to decrease risk factors related to suicide. The intervention included up to 10 CTSP sessions, 9 booster sessions, and any TAU sessions. Additional details about treatment conditions can be found elsewhere (Slesnick et al., Reference Slesnick, Zhang, Feng, Wu, Walsh and Granello2020).
Ongoing supervision, fidelity, and treatment attendance
The independently licensed therapists read the CTSP manual (Wenzel et al., Reference Wenzel, Brown and Beck2009) and attended a 3-day onsite training of the CTSP intervention by Dr. Wenzel. Additionally, Dr. Wenzel provided weekly virtual supervision of digitally recorded sessions and evaluated sessions for therapist competence using the Cognitive Therapy Rating Scale (Young & Beck, Reference Young and Beck1980). Both therapists received satisfactory scores in their evaluations. At the 6-month timepoint, CTSP+TAU participants attended an average of 5.01 sessions (SD = 6.08), and TAU participants attended an average of 3.32 sessions (SD = 4.65).
Measures
Suicidal ideation was assessed using the Scale for Suicidal Ideation – Worst Point (SSI-W; Beck et al., Reference Beck, Brown and Steer1997) at all time points. The SSI-W is a 19-item scale used to measure the severity of suicidal attitudes, thoughts, and desires in the past 90 days, rated on a 3-point Likert-type scale (0 = “none”, 2 = “moderate to strong”). The SSI-W is administered by the research assistant. A sample items is “My reasons for dying outweigh my reasons for living.” Total scores are generated by summing up responses on all items, with higher scores indicate higher suicidal ideation. The SSI-W has good internal consistency and validity (Beck et al., Reference Beck, Brown and Steer1997). In this study, alpha levels for the SSI-W ranged from .72 to .87.
Predictors towards trajectory groups of suicidal ideation
Depressive symptoms were assessed at baseline using the Beck Depression Inventory – II (BDI-II; Beck et al., Reference Beck, Brown and Steer1997). The BDI-II is the most frequently used self-report instrument for assessing mood as well as cognitive and somatic aspects of depression, with good internal consistency estimates for psychiatric and nonpsychiatric populations (Beck & Steer, Reference Beck and Steer1988). Items are rated on a 0–3 scale, assessing aspects of depression such as loss of pleasure, punishment feelings, and worthlessness. Cronbach’s alpha in the current study was .90 at baseline.
Substance use was assessed at baseline using the fifth edition of the Addiction Severity Index (ASI; McLellan et al., Reference McLellan, Kushner, Metzger, Peters, Smith, Grissom, Pettinati and Argeriou1992), a structured clinical interview administered by research assistants. The ASI assesses the type, frequency, and amount of substance use in the prior 30 days and has shown good reliability (Zanis et al., Reference Zanis, McLellan, Cnaan and Randall1994). This measure was scored using the procedures by McGahan et al. (Reference McGahan, Griffith, Parente and McLellann1986), with higher scores indicating more frequent and severe substance use. In addition to assessing the days of using different types of substances (e.g., alcohol, cannabis, cocaine, heroin, polydrug, etc.), this measure assesses the severity of substance use. Sample items include “Days of any alcohol use at all in the past 30 days” and “How troubled or bothered have you been in the past 30 days by drug problems?” In this study, the scores of alcohol and drug use (ranges 0–1) were standardized and averaged to generate a final score for substance use. At baseline, 86.7% of youth reported any substance use.
Childhood abuse experience was measured at baseline. Three questions were asked: “Before you were 18 years old, has anyone ever hit, punched, kicked, shaken, tortured, or otherwise physically hurt you that made you bleed or gave you bruises or scratches?”, “Before you were 18 years old, has anyone ever kissed you in a sexual way or touched your body in a way that made you feel uncomfortable against your will?”, and “Before you were 18 years old, has anyone ever had oral, anal, or vaginal intercourse with you or insert a finger or object in your anus or vagina?” A final score was generated by aggregating youth’s response to both questions (0 = no abuse, 1 = has experienced physical or sexual abuse).
Demographic predictors were assessed at baseline using a demographic questionnaire, including sex (0 = male, 1 = female), race (0 = minority races, 1 = White, non-Hispanic), and education in years. We also asked about youth’s number of days being homeless. Number of attended CTSP and TAU sessions during the 6 months of treatment were tracked by the therapists and reported on a monthly basis.
Outcomes in suicide-related factors
Cognitive distortions were assessed at baseline and 9 months with the Inventory of Cognitive Distortions (ICD; Yurica, Reference Yurica2002). The ICD is a 69-item self-report questionnaire rated on a 5-point Likert scale (1 = “never”, 5 = “always”). Sample items include “I tend to discount the good things about me,” and “Even small events can bring on catastrophic consequences.” A total score was calculated by summing all items, with higher scores indicating a greater severity of cognitive distortions. The ICD has shown strong concurrent validity and internal consistency (Yurica, Reference Yurica2002). Alpha levels in the current study were .96 at baseline and .97 at 9 months.
Acquired capability for suicide was assessed at baseline and 9 months using the Acquired Capability for Suicide Scale (ACS; Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). The 20-item ACS assesses fearlessness about lethal self-injury, is rated on a 5-point scale (0 = “not at all like me”, 4 = “very much like me”), and has adequate reliability (Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). Sample items include “The sight of my own blood does not bother me,” and “The fact that I am going to die does not affect me.” In this study, alpha levels were .82 at baseline and .83 at 9 months.
Perceived burdensomeness and thwarted belongingness, the two components of suicidal desires, were assessed at baseline and 9 months using the 25-item Interpersonal Needs Questionnaire (INQ; Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). Items are rated on a 7-point Likert scale (1 = “not at all true”, 7 = “very true”). Sample items include “These days I think I have failed the people in my life,” and “These days I think my death would be a relief to the people in my life.” The INQ has shown high internal consistency (Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). Alpha levels in the current study were .87 and .91 at baseline and 9 months, respectively.
Hopelessness was assessed at baseline and 9 months using the Beck Hopelessness Scale (BHS; Beck & Steer, Reference Beck and Steer1988). The BHS measures positive and negative beliefs about the future experienced in the past week via 20 true-false statements. The BHS is a commonly used measure of hopelessness, with high internal reliability (Beck & Steer, Reference Beck and Steer1988). Example items include “I might as well give up because I can’t make things better for myself,” and “My future seems dark to me.” Alpha coefficients were .90 at baseline and .89 at 9 months in the current study.
Distress tolerance was assessed using the Distress Tolerance Scale (DTS; Simons & Gaher, Reference Simons and Gaher2005) at baseline and 9 months. The DTS is a 15-item self-report scale examining the extent to which individuals experience negative emotions as intolerable. Items are rated on a 5-point Likert scale (1 = “strongly agree,” 5 = “strongly disagree”). Sample items include “I can’t handle feeling distressed or upset,” and “I’ll do anything to avoid feeling distressed or upset.” The DTS has shown high internal consistency and concurrent validity (Simons & Gaher, Reference Simons and Gaher2005). Alpha levels in the current study were .89 and .91 at baseline and 9 months, respectively.
Impulsivity was measured at baseline and 9 months using the Impulsivity Control Scale (ICS; Plutchik & Van Praag, Reference Plutchik and Van Praag1989). The ICS is a 15-item scale with items rated on a 4-point scale, ranging from “never” to “very often.” The ICS assesses the tendency to engage in impulsive behaviors and lack of patience, and has shown good internal reliability (Plutchik & Van Praag, Reference Plutchik and Van Praag1989). Sample items include “Do you find it difficult to wait on lines?”, and “Do you finish things you start?” In this study, alpha levels were both .77 at baseline and 9 months.
Social problem solving was assessed at baseline and 9 months via the 25-item Social Problem Solving Inventory – Revised Short-Version (SPSI; D’Zurilla & Nezu, Reference D’Zurilla and Nezu1990), one of the most widely used self-report instruments for measuring personal perceptions of social problem-solving ability as related to suicidal behaviors. Items are rated on a 5-point scale (0 = “not at all true of me”, 4 = “extremely true of me”). The SPSI assesses both constructive/adaptive and dysfunctional problem-solving dimensions, has shown high internal consistency and concurrent validity (Hawkins et al., Reference Hawkins, Sofronoff and Sheffield2009). Alpha levels were .81 at baseline and .77 at 9 months.
Social network was assessed at baseline and 9 months using the Social Network Inventory, a modified version of the Social Network Interview (SNI; Stein et al., Reference Stein, Rappaport and Seidman1995). The SNI is administered by the research assistant and assesses the total number of network members in the participant’s social network, frequency of contact with said members, and satisfaction with any help received from their social network members. In the current study, we used family and friends network contact, measured by summing up the frequency of contact from each member of family or friend network, using 5-point scales (0 = “about once a year or less”, 4 = “about daily”); as well as total scores of family and friend network satisfaction (0 = “feel worse”, 4 = “feel very relieved”). Higher scores indicating higher contact frequency or satisfaction levels. The SNI has been validated for use with homeless samples and high-risk youth.
Data analytic plan
Analysis was conducted using the Mplus 8.1 program (Muthén & Muthén, Reference Muthén and Muthén2017). Little’s MCAR test (Little, Reference Little1988) revealed that data were missing completely at random (MCAR), χ 2 (71) = 64.40, p = .70. Full information likelihood (FIML) estimation was thus used as recommended to generate unbiased estimates under the condition of MCAR (Enders & Bandalos, Reference Enders and Bandalos2001), with robust (Huber-White) standard errors to handle skewed data (e.g., the number of sessions; Li, Reference Li2016).
To test the first hypothesis regarding different subgroups of youth, we used a person-centered approach – Growth Mixture Modeling (GMM). GMM was conducted based on the 4 time points of suicidal ideation, with the treatment condition used as a control variable in the model. By including youth from both groups in the analyses and using the treatment condition as a control variable, we would be able to address questions such as whether youth in different trajectory groups respond differently to treatment conditions, and whether treatment condition would predict different group memberships. A series of GMM models with different numbers of classes (1–6 classes) were estimated to determine the model that best fit the data. Several criteria were used to determine the best fitting model: (a) a small Bayesian Information Criteria (BIC) value as well as a small BIC value adjusted by sample size (Adjusted BIC); (b) an entropy value above 0.80; (c) the p-value for Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (LRT); (d) a reasonable number of youth assigned into each class; and (e) interpretability of the class memberships (Jung & Wickrama, Reference Jung and Wickrama2008).
Second, we tested key predictors, including mental health and demographic variables as well as session attendance, that might explain youth’s group membership. We used the automatic three-step approach estimating predictors to latent classes in GMM (Asparouhouv & Muthén, Reference Asparouhouv and Muthén2013). The analysis is equivalent to a multinomial logistic regression using predictors to predict trajectory group membership, which was a latent categorical variable created using the latent class posterior distribution generated in the first step, accounting for classification errors.
Third, regarding the mean differences of outcome variables across subgroups, we used the three-step approach estimating distal outcomes in GMM as recommended (Asparouhouv & Muthén, Reference Asparouhouv and Muthén2013). Youth’s suicide-related outcomes at the 9-month assessment were regressed on to group membership with classification errors being taken into account, whereas the same variables at baseline and the treatment condition were controlled for in the model.
Results
Descriptive statistics for suicidal ideation and key mental health and demographic predictors are presented in Table 1. For the first hypothesis, a series of GMMs were estimated to identify subgroups of youth, based on their change trajectories of suicidal ideation from baseline to the 9-month assessment (Table 2). Based on preliminary examination showing that the trajectory was nonlinear (i.e., over time the reduction of suicidal ideation became slower), we used quadratic growth models in GMMs. The LRTs suggested that the 2-class solution was statistically better than the 1-class solution, and the 3-class solution was better than the 2-class solution. The 3-class solution also had relatively low BIC and high entropy values. Based on the theoretical hypothesis and the fit indices, the 3-class solution was considered optimal (Figure 3).
Table 2. Model fit indices for growth mixture models with 1 to 6 classes

Note. BIC = Bayesian information criteria; LRT = Lo-Mendell-Rubin adjusted likelihood ratio test.

Figure 3. Growth trajectories of suicidal ideation of each subgroup, both observed and estimated values.
In the first group, youth showed relatively lower levels of initial suicidal ideation (intercept = 21.49, SE = 0.47), a quick decline especially over the first 3 months (slope = −16.46, SE = 0.53, t = −30.87, p < .001) which significantly slowed down later (quadratic effect = 3.44, SE = 0.15, t = 23.78, p < .001). We named this group “Fast Declining” (n = 112, 74.7%). In the second group, the mean of initial suicidal ideation was slightly higher (intercept = 23.58, SE = 1.83), whereas suicidal ideation reduced slower (slope = −4.88, SE = 1.70, t = −2.87, p = .004) but barely decelerated over the course of 9 months (quadratic effect = −0.74, SE = 0.43, t = −1.73, p = .08). We named this group “Steadily Declining” (n = 9, 6.0%). The youth in the third group showed even higher initial levels of suicidal ideation (intercept = 23.64, SE = 0.97) as well as a decline (slope = −8.25, SE = 1.04, t = −7.94, p < .001) which slowed down over the 9-month period (quadratic effect = 1.75, SE = 0.27, t = 6.63, p < .001), maintaining elevated subclinical levels of suicidal ideation. We thus named this group “Chronic” (n = 29, 19.3%). The treatment condition did not predict group memberships (Fast Declining versus Chronic β = −0.24, SE = 0.47, t = −0.51, p = .61, Odds ratio = 0.79 with 95% CI [0.31, 1.98]; Steadily Declining versus Chronic β = −1.03, SE = 0.82, t = −1.25, p = .21, Odds ratio = 0.36 with 95% CI [0.07, 1.79]; Fast Declining versus Steadily Declining β = 0.78, SE = 0.75, t = 1.04, p = .30, Odds ratio = 2.19 with 95% CI [0.50, 9.53]).
Next, we added predictors to group memberships (Table 3). Youth in the Chronic group had more baseline substance use than the Steadily Declining group, and they were also more likely to be White, non-Hispanic than the Fast Declining group. Youth in the Chronic group attended more CTSP sessions than other groups. In comparison, youth in the Steadily Declining group all had a history of childhood abuse, which was significantly higher compared to the rate in the Fast Declining group (84.8%) and in the Chronic group (75.9%).
Table 3. Predictors for group memberships

Note. OR = odds ratio. Childhood abuse: 0 = no, 1 = yes. Sex: 0 = male, 1 = female. Race: 0 = minority races, 1 = White. Bold values indicate statistically significant results.
a Reference group: fast declining.
b Reference group: steadily declining.
c Standardized errors, t-values, and odds ratios were not estimated, as all participants in the Steadily Declining group had a history of childhood abuse (i.e., no variance in this group), whereas the rate was 84.8% in the Fast Declining group and 75.9% in the Chronic group.
* p < .05.
For our third hypothesis, we used group memberships to predict suicide-related outcomes (Table 4). Youth in the Chronic group showed significant higher levels of cognitive distortions, hopelessness, impulsivity, and thwarted belongingness at the 9-month follow-up assessment compared to their peers in the Fast Declining group, controlling for the baseline levels and the treatment condition. Youth in the Chronic group also showed significantly higher levels of perceived burdensomeness compared to those in the Fast Declining group and the Steadily Declining group at 9 months. Youth in the Chronic group had lower levels of social problem solving compared to those in the Fast Declining group at 9 months. Youth in the Chronic group reported higher frequency of contact with their friends than those in the Steadily Declining group at 9 months. No significant between-group differences were found in acquired capacity for suicide, distress tolerance, or family network contact or satisfaction, or friend network satisfaction.
Table 4. Trajectory group comparisons for youth suicide-related outcomes at 9-month assessment
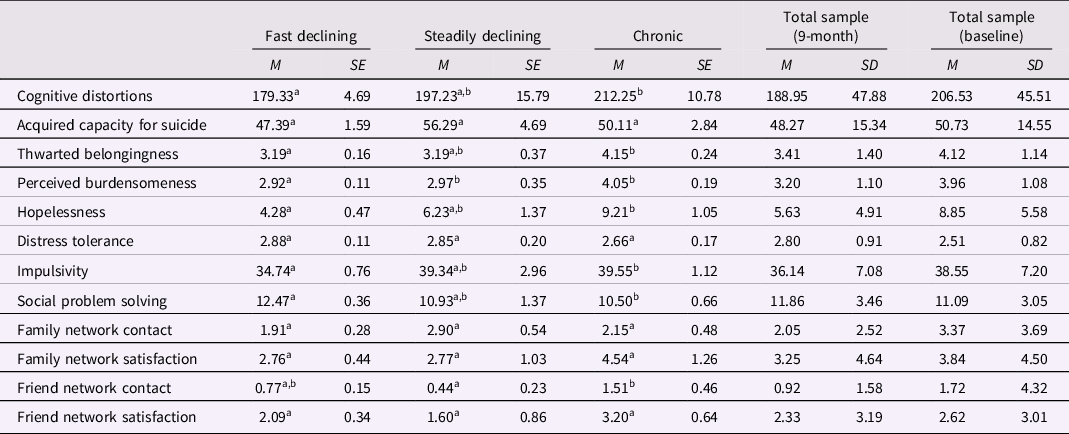
Note. Different superscripts within the same row indicate statistically significant mean differences, p < .05.
Discussion
The current study examined longitudinal heterogenous trajectories of suicidal ideation over a 9-month period among a high-risk sample of homeless youth who experienced suicidal ideation. Using a person-centered approach, we identified three groups of youth with distinct trajectories of suicidal ideation, and examined the predictors and outcomes of the trajectory groups. This study enhances the current understanding of heterogenous treatment effects in suicidal ideation among homeless youth, with implications to improve research and intervention efforts towards this high-risk, vulnerable population.
Heterogenous trajectory groups of suicidal ideation
This study identified three subgroups of youth with different trajectories of suicidal ideation: Fast Declining (74.7%), Chronic (19.3%), and Steadily Declining (6.0%). The findings mirrored those of Czyz and King (Reference Czyz and King2015) and Wolff et al. (Reference Wolff, Davis, Liu, Cha, Cheek, Nestor, Frazier, Schaffer and Spirito2018) who used an adolescent sample hospitalized for suicide. In the current study, we found a higher percentage of youth who had lower suicidal ideation levels (74.7%), compared to previous numbers (31.6% in Czyz & King, Reference Czyz and King2015 and 33.7% in Wolff et al., Reference Wolff, Davis, Liu, Cha, Cheek, Nestor, Frazier, Schaffer and Spirito2018). The difference may lie in the fact that the adolescents in those two studies had even higher risk given that they were hospitalized for suicide, but in the current study we referred youth at imminent risk for suicide to a local hospital for ethical reasons. Our findings were different from those of Madsen et al. (Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016) and Goldston et al. (Reference Goldston, Erkanli, Daniel, Heilbron, Weller and Doyle2016) who found a group with increased suicidal ideation, possibly due to the fact that the intervention in Madsen et al. (Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016) was not specifically focused on suicidality and the sample in Goldston et al. (Reference Goldston, Erkanli, Daniel, Heilbron, Weller and Doyle2016) did not always continue to receive treatment after hospital discharge. Our study was similar to previous randomized controlled trials which identified multiple trajectories groups but did not find that the treatment condition predicted the group memberships (e.g., Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019; Czyz & King, Reference Czyz and King2015; Madson et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016). It is likely that the different trajectories were affected by other risk factors that were intrinsic to youth (as discussed below), rather than the treatment group assignment (Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019; Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016). Together, findings of this study and previous studies (e.g., Czyz & King, Reference Czyz and King2015; Goldston et al., Reference Goldston, Erkanli, Daniel, Heilbron, Weller and Doyle2016; Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016; Wolff et al., Reference Wolff, Davis, Liu, Cha, Cheek, Nestor, Frazier, Schaffer and Spirito2018) support investigations into the heterogenous trajectories of suicidal ideation across a variety of high-risk populations.
Predictors characterizing trajectory groups
Next, we characterized youth in different trajectory groups by mental health and demographic predictors, as well as session attendance. Youth in the Chronic group were characterized by more substance use (compared to the Steadily Declining group), and a higher likelihood to be White, non-Hispanic (compared to the Fast Declining group). Historically, White youth are more likely to complete suicide than Black youth, though this trend is decreasing (Kubrin & Wadsworth, Reference Kubrin and Wadsworth2009). It appeared that substance use was a potent risk factor that slowed down the reduction in youth’s suicidal ideation in intervention (Hallfors et al., Reference Hallfors, Waller, Ford, Halpern, Brodish and Iritani2004). Substance use is likely a factor associated with these youth needing more CTSP sessions to recover. In contrast, youth in the Steadily Declining group were characterized as having a history of childhood abuse compared to other groups. Although these youth may have a surge of suicidal ideation at baseline, possibly due to childhood abuse history, they also recovered slowly and steadily, showing longer-lasting improvement.
Findings support a host of risk factors for suicidal ideation (e.g., Esposito-Smythers & Spirito, Reference Esposito-Smythers and Spirito2004; Hallfors et al., Reference Hallfors, Waller, Ford, Halpern, Brodish and Iritani2004; Nock et al., Reference Nock, Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). In the current study, we further revealed that these risk factors may interfere with youth’s recovery post-intervention, as unique combinations of risk factors may channel youth into different change trajectories with more rapid recovery versus more chronic, stable levels of suicidal ideation. This information may be used by clinicians at the beginning of treatment to identify youth most vulnerable towards less optimal treatment outcomes.
Suicide-related psychosocial outcomes
Finally, we examined outcomes in suicide-related factors among different groups, as these factors may feed into youth’s future suicidality. We found that youth in the Chronic group showed significantly higher risk for future suicide, as they had higher cognitive distortions, hopelessness, impulsivity, and thwarted belongingness, and lower social problem solving compared to those in the Fast Declining group at 9 months. They also had higher perceived burdensomeness compared to youth in two other groups, which is a robust predictor of suicidal ideation and attempts (Chu et al., Reference Chu, Walker, Stanley, Hirsch, Greenberg, Rudd and Joiner2018).
Additionally, youth in the Chronic group reported higher frequency of contact with their friends than those in the Steadily Declining group at 9 months. Although this finding was not expected, as more contact with social networks can be a desired outcome, previous studies also show that deviant peer relationships increase suicide risk for homeless youth (Rice et al., Reference Rice, Kurzban and Ray2012). It is likely that the urgency of suicidal ideation motivated youth in the Chronic group to reach out to their friends over time, whereas it is difficult to rely on family members due to the often conflictual relationships that homeless youth have with their families (Bao et al., Reference Bao, Whitbeck and Hoyt2000). Notably, we did not find between-group differences regarding family network satisfaction or contact. It appears that changes in suicidal ideation are not associated with youths’ family relationships.
In contrast, youth in the Steadily Declining group were not found to be different from those in the Fast Declining group in 9-month suicide-related factors. Our findings are consistent with previous studies by revealing that the chronicity or persistence of suicidal ideation, rather than the acute elevation of symptoms, is a more robust predictor for future suicide risk (Allan et al., Reference Allan, Gros, Lancaster, Saulnier and Stecker2019; Czyz & King, Reference Czyz and King2015). That is, youth in the Chronic group are clearly at higher risk showing many more suicide-related risk factors even post-treatment.
We did not find differences in acquired capacity for suicide or distress tolerance among youth subgroups. These two factors are stronger predictors of suicide attempts than suicidal ideation (Anestis et al., Reference Anestis, Bagge, Tull and Joiner2011; Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). As such, it is likely that the observed change patterns in suicidal ideation are not related to change in distress tolerance or capacity to complete suicide. As suicidal ideation and acquired capacity for suicide are two integral factors associated with suicidal behaviors, this finding suggests an independence of these factors, as asserted in the interpersonal-psychological theory of suicide (Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a). As prior suicide attempts, childhood maltreatment, and impulsivity are some of the hypothesized mechanisms predicting acquired capability to complete suicide (Van Orden et al., Reference Van Orden, Witte, Gordon, Bender and Joiner2008a), future research is warranted to study effective treatment elements that may reduce this capacity specifically, thus reducing suicide risk.
Strengths, limitations, and implications
In light of the framework of heterogenous treatment effects (Varadhan et al., Reference Varadhan, Segal, Boyd, Wu and Weiss2013), the current study characterized distinct change trajectories of suicidal ideation among a high-risk sample of homeless youth who experienced suicidal ideation. Using longitudinal clinical data, we assessed participants four times over a 9-month period, which provided valuable evidence for the process of change during intervention. The current study revealed different patterns of change during suicide intervention (rather than a unitary response pattern), as well as factors contributing to such patterns that can be included at treatment screening. This study further highlighted distinct outcomes in subgroups of youth, underscoring the importance of considering heterogeneity in youth suicide prevention studies (Musci et al., Reference Musci, Kharrazi, Wilson, Susukida, Gharghabi, Zhang, Wissow, Robinson and Wilcox2018).
Several limitations should be considered when interpreting the results of this study. First, we collected data from a convenience sample of youth accessing a drop-in center. Thus, findings of this study may not generalize to youth who do not utilize drop-in centers, and who may suffer greater risk due to limited motivation and skills to obtain resources. Second, this study utilized self-report measures that can be influenced by social desirability. Self-reported measures are common in suicide research. However, researchers have also suggested using alternative measures to assess suicide risk, such as the implicit association test. Also, some predictors (e.g., substance use) were measured during a shorter time span compared to suicidal ideation prior to intervention. This warrants caution when interpreting the findings as we cannot draw causal relations from such findings. Third, in our analysis we did not fully examine intervention effects of CTSP (please refer to Slesnick et al., Reference Slesnick, Zhang, Feng, Wu, Walsh and Granello2020 for a discussion of intervention effects). Rather, we used an intent-to-treat analytic approach and treated the treatment condition as a predictor to group memberships and outcomes. An intent-to-treat analytic approach usually underestimates treatment effects, but it also generates results that are closer to the real-world effect of treatments (e.g., “as-assigned” treatment effects; Ten Have et al., Reference Ten Have, Normand, Marcus, Brown, Lavori and Duan2008). As the nature of our investigation was associative, we cannot draw causal conclusions from our observations regarding treatment attendance and effects (e.g., youth in the Chronic group had more CTSP sessions). Fourth, we had a relatively small group from GMM. Although a small group is not unprecedented in research concerning severe clinical problems because of the rarity of the issues (e.g., Madsen et al., Reference Madsen, Karstoft, Secher, Austin and Nordentoft2016), it may raise concerns of reliability of interpretation, and needs to be replicated in a larger sample. Fifth, while monitoring suicidal attempts and hospitalization throughout the study, only one participant reported hospitalization due to a suicidal attempt, and six others reported hospitalization or emergency room visits due to suicidal thoughts or depression. Due to the small size of participants experiencing these adverse events, we were not able to test whether the trajectory groups were associated with different suicidal behaviors. We contemplated that the lower frequency of actual suicidal attempts could be due to a relatively short study timeframe (9 months), whereas longer-term follow-ups are needed to observe the longitudinal effects of treatment on suicidal behaviors. Additionally, service-using homeless youth may have additional resilience factors such as problem-solving skills (which helped them to seek out services), social connections (friends and service staff met at the drop-in center), and higher self-esteem resulting from problem-solving skills and social connections. Actually, several study participants reported actively seeking help and hospitalization when experiencing suicidal thoughts. The valuable information that we learnt from this project will inform and warrant our future research efforts. Furthermore, our analyses did not examine time-varying effects of baseline variables such as depression, substance use, and homelessness when examining the trajectories of suicidal ideation. It is likely these risk factors lessened over the course of treatment, thus affecting the severity of suicidal ideation, and this should be addressed by future studies. Finally, although an advantage of this study is to be able to test multiple predictors and suicide-related outcomes during intervention to further our current understanding on differential treatment outcomes, doing so may also have introduced reduced study power due to multiple comparisons. This might explain the non-significant findings on several predictors or outcomes. Future intervention studies should incorporate a large sample size for sufficient power to better understand differential characteristics in the heterogeneous trajectories of youth’s suicidality. Future studies may also include a variety of predictors of suicidality among homeless youth that are not examined in the current research. These predictors can be specific to suicidality (e.g., hopelessness, distress tolerance) or to the homeless population (e.g., being a sexual minority, street victimization, or having access to resources; Rhoades et al., Reference Rhoades, Rusow, Bond, Lanteigne, Fulginiti and Goldbach2018).
The findings offer several clinical implications. Clinicians may keep in mind that youth have different trajectories and differential response to suicide prevention treatment. In particular, we found that the Chronic group showing the highest number of risk factors and poorest response to treatment, and these youth were more likely to be White, non-Hispanic and to have more severe substance use problems, factors that can be easily screened prior to treatment and to alert providers to include a focus on substance use treatment. Further, there was no difference in acquired capacity for suicide or distress tolerance among the groups, indicating the change in suicidal ideation is not related to change in these risk factors. Future treatment attention towards increasing distress tolerance and reducing acquired capacity for suicide may be necessary to reduce suicide risk even further. In all, a better understanding towards heterogenous therapy responses can help improve clinical intervention efforts and reduce premature mortality and hospitalization among this very vulnerable population.
Acknowledgments
We are thankful towards youth who participated in this study and thankful for NIDA in supporting the original intervention research.
Author contributions
Wu conceptualized the secondary data analysis, analyzed the data, wrote the results and discussion sections, and edited the manuscript. Zhang wrote the literature review. Walsh cleaned the data and wrote the method section. Slesnick acquired funding for the study, designed the original intervention study, oversaw the execution of the study, provided the data, and edited the manuscript. All author contributed significantly to this manuscript and approved the publication of this paper.
Funding statement
This work was supported by NIDA Grant # R34DA037845 to the last author. NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.










