Childhood adversities include multiple types of potentially traumatic stressors, such as child maltreatment, domestic violence, and parental pathology (Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards and Marks1998). According to the landmark Kaiser study, more than half of adults (63.9%) reported at least one adverse childhood experience (Centers for Disease Control and Prevention, 2016). A substantial body of literature has documented that childhood adversity has a dose–response relationship with an array of health outcomes later in life, including mental health: More reported adverse childhood experiences are associated with poorer health consequences (Hughes et al., Reference Hughes, Bellis, Hardcastle, Sethi, Butchart, Mikton and Dunne2017; Kalmakis & Chandler, Reference Kalmakis and Chandler2015).
Less empirical attention has been given to the intergenerational influences of childhood adversity; mothers’ earlier adverse experiences may compromise not only their own developmental outcomes, but also those of their children (Stargel & Easterbrooks, Reference Stargel and Easterbrooks2020; Stepleton et al., Reference Stepleton, Bosk, Duron, Greenfield, Ocasio and MacKenzie2018). With few exceptions (e.g., Doi et al., Reference Doi, Fujiwara and Isumi2021; Schickedanz et al., Reference Schickedanz, Halfon, Sastry and Chung2018; Stargel & Easterbrooks, Reference Stargel and Easterbrooks2020), most relevant studies have focused on children’s developmental outcomes into early childhood. Further, existing studies typically focused on one developmental epoch rather than multiple developmental periods. As such, no identified studies have evaluated the extent to which the impact of mothers’ childhood adverse experiences on children’s developmental outcomes varies across the children’s development, leaving an untapped opportunity to reveal critical developmental periods for multigenerational intervention strategies, which are increasingly suggested (Hagan et al., Reference Hagan, Shaw and Duncan2017). Child development is a dynamic process with ongoing growth, fluctuation, and malleability across childhood and adolescence (Cheng et al., Reference Cheng, Johnson and Goodman2016). With that consideration, it is imperative to expand the assessment period beyond early childhood, utilize data with repeated assessments across multiple developmental epochs, and account for the developmental nature of mental health over time to further clarify the influences of mothers’ childhood adversity on the next generation’s mental health. Finally, although evidence in within-generation studies with adults increasingly suggests possible gender differences in the impacts of childhood adversity (Cavanaugh et al., Reference Cavanaugh, Petras and Martins2015), gender differences in the intergenerational influences of childhood adversity have rarely been evaluated. Probing possible gender differences is critical, because it would advance the field’s capacity to locate a subgroup of children with particularly heightened vulnerabilities.
To fill these critical gaps in prior studies, the current study examined the influences of maternal childhood adversities on externalizing and internalizing problems (between ages 4.53 and 17 years) among children born to teen mothers. Specifically, informed by the life course perspective on the influences of adversities (Ben-Shlomo & Kuh, Reference Ben-Shlomo and Kuh2002; Braveman & Barclay, Reference Braveman and Barclay2009; Nelson & Gabard-Durnam, Reference Nelson and Gabard-Durnam2020), we probed the question of timing: Is there a developmental inflection point when the intergenerational influences of maternal childhood adversity on children’s mental health become particularly elevated? Children born to young mothers often experience more mental (Lee et al., Reference Lee, Jeong, Yuan, Boden, Umana-Taylor, Noris and Cederbaum2020) and behavioral (Cederbaum et al., Reference Cederbaum, Jeong, Yuan and Lee2020) problems. Further, teen mothers are more likely to experience adversity in their own childhood (Hillis et al., Reference Hillis, Anda, Dube, Felitti, Marchbanks and Marks2004; Madigan et al., Reference Madigan, Wade, Tarabulsy, Jenkins and Shouldice2014) in comparison to older mothers. Thus, this population permits meaningful investigation of the intergenerational linkage between maternal childhood adverse experiences and children’s mental health, extending the body of literature regarding the role of maternal childhood adversity in shaping mental health among youth at elevated risk of the early onset or later escalation of psychopathology.
Intergenerational influences of maternal childhood adversity: An unexplored developmental inflection point
An emerging body of literature has documented that the deleterious impacts of childhood adversity may trickle down to the next generation and play a role in shaping children’s mental health; maternal childhood adversity has been associated with increased mental health problems in children at ages 2 (Letourneau et al., Reference Letourneau, Dewey, Kaplan, Ntanda, Novick and Thomas2019), 5 (Cooke et al., Reference Cooke, Racine, Plamondon, Tough and Madigan2019), 8 (Stargel & Easterbrooks, Reference Stargel and Easterbrooks2020; Stepleton et al., Reference Stepleton, Bosk, Duron, Greenfield, Ocasio and MacKenzie2018), and 9 (Schickedanz et al., Reference Schickedanz, Halfon, Sastry and Chung2018). Mechanisms explicating the intergenerational impacts of childhood adversity on children’s mental health have been increasingly proposed and tested, including biological (e.g., disrupted allostasis and neural functioning), elevated inflammation (Danese & McEwen, Reference Danese and McEwen2011; Perry & Pollard, Reference Perry and Pollard1998), brain development in utero (Buss et al., Reference Buss, Entringer, Moog, Toepfer, Fair, Simhan and Wadhwa2017), maternal psychosocial distress (Doi et al., Reference Doi, Fujiwara and Isumi2021; Madigan et al., Reference Madigan, Wade, Plamondon, Maguire and Jenkins2017; Letourneau et al., Reference Letourneau, Dewey, Kaplan, Ntanda, Novick and Thomas2019), and parenting (Schickedanz et al., Reference Schickedanz, Halfon, Sastry and Chung2018) factors. Although these existing studies have shed important light on the intergenerational impacts of childhood adversity, they are limited in two important ways.
First, one important mechanistic aspect underlying the intergenerational influences of maternal childhood adversity has been overlooked—a developmental point when the intergenerational influences of maternal childhood adversity on children’s mental health clearly emerge. The life course perspective suggests that there might be a critical or sensitive period during which the adverse effect of exposure to risk on developmental outcomes becomes more pronounced (Ben-Shlomo & Kuh, Reference Ben-Shlomo and Kuh2002; Braveman & Barclay, Reference Braveman and Barclay2009; Nelson & Gabard-Durnam, Reference Nelson and Gabard-Durnam2020). Following this logic in the current study, maternal childhood adversity may function as a distal risk factor that affects children’s mental health, yet there may be developmental periods when the intergenerational effects of maternal childhood adversity experiences become more prominent. The developmental nature of internalizing and externalizing behavior problems may warrant further exploration of this possibility.
Internalizing and externalizing behavior problems are fundamentally developmental, although the specific manifestation of their developmental nature differs. Generally, externalizing behavior problems tend to surface at a moderate level in infancy and toddlerhood (Tremblay et al., Reference Tremblay, Nagin, Seguin, Zoccolillo, Zelazo, Boivin and Japel2004), decrease during childhood (Miner & Clarke-Stewart, Reference Miner and Clarke-Stewart2008), and then climb and peak during adolescence (Moffitt, Reference Moffitt1993), whereas internalizing behavior problems tend to surface during mid-adolescence (Nivard et al., Reference Nivard, Lubke, Dolan, Evans, St. Pourcain, Munafò and Middeldorp2017). By definition, detrimental impacts of maternal childhood adverse experiences on children’s mental health imply that children born to mothers with childhood adversity may diverge from trends developmentally appropriate at a given developmental period and experience heightened levels of mental health problems. Such deviation may be less prominent during developmental periods when mental health problems are expected to be high (e.g., adolescence). On the other hand, the negative influences of maternal childhood adversity on children’s mental health may emerge more clearly during developmental periods when mental health problems are expected to be low (e.g., childhood). Further, the predictive capacity of maternal childhood adversity may attenuate during adolescence, a developmental period when factors embedded in other ecological contexts beyond family, such as neighborhood influences, start gaining salience (Sharkey & Faber, Reference Sharkey and Faber2014). Yet the importance of pubertal maturation has been noted for child developmental in general (Byrne et al., Reference Byrne, Whittle, Vijayakumar, Dennison, Simmons and Allen2017; Mendle, Reference Mendle2014; Pfeifer & Allen, Reference Pfeifer and Allen2021). Consistently, pubertal maturation, particularly its early occurrence, has been associated with elevated responsiveness to stress (Copeland et al., Reference Copeland, Worthman, Shanahan, Costello and Angold2019; Dahl & Gunnar, Reference Dahl and Gunnar2009) and youth mental health problems (Dimler & Natsuaki, Reference Dimler and Natsuaki2015; Ullsperger & Nikolas, Reference Ullsperger and Nikolas2017). This consideration suggests that the impacts of maternal childhood adversity on children’s mental health may emerge more prominently during adolescence.
Clarifying the developmental inflection point of a given risk exposure has increasingly been noted as critical to tailoring intervention strategies and maximizing their potential benefits (Cheng et al., Reference Cheng, Johnson and Goodman2016; McLaughlin, Reference McLaughlin2016). Relatedly, few within-generation studies have examined whether timing of exposure to childhood adversity is particularly detrimental for developmental outcomes in childhood (Nelson & Gabard-Durnam, Reference Nelson and Gabard-Durnam2020; Schroeder et al., Reference Schroeder, Slopen and Mittal2020), adolescence (Yoon, Reference Yoon2020), and adulthood in retrospective studies (Atzl et al., Reference Atzl, Narayan, Rivera and Lieberman2019; Schalinski et al., Reference Schalinski, Teicher, Nischk, Hinderer, Muller and Rockstroh2016). However, no identified studies have examined whether the unfolding of the intergenerational effects of maternal childhood adversity may depend on children’s developmental periods. As such, the extent to which the intergenerational influences of maternal childhood adversity on children’s mental health vary across developmental epochs is unknown, leaving an untapped opportunity to properly orchestrate intervention targets at the right time. Studying this issue necessitates panel data from the same children across multiple developmental epochs. The current study leveraged a long-running panel study with children born to teen mothers to address this critical gap.
Gender differences
Gender differences in the influences of risk factors on mental health have been conceptually proposed and empirically tested. Conceptually, gendered strain theory (Broidy & Agnew, Reference Broidy and Agnew1997) and the gender socialization hypothesis (Chodorow, Reference Chodorow1978; Kågesten et al., Reference Kågesten, Gibbs, Blum, Moreau, Chandra-Mouli, Herbert and Amin2016) suggest that mental health manifestation in response to distress tends to differ across genders—girls may take distress inward, more likely expressing their distress in a form of internalizing problems, whereas boys may express distress outward, more likely manifesting their distress in a form of externalizing problems (Chaplin & Aldao, Reference Chaplin and Aldao2013). Corroborating such conceptual speculation, empirical evidence indicated that internalizing problems are elevated among girls (Carter et al., Reference Carter, Godoy, Wagmiller, Veliz, Marakovitz and Briggs-Gowan2010; Gutman & Codiroli McMaster, Reference Gutman and Codiroli McMaster2020) and externalizing problems are elevated among boys (Arnett et al., Reference Arnett, Pennington, Willcutt, DeFries and Olson2015; Castelao & Kröner-Herwig, Reference Castelao and Kröner-Herwig2014; Paz et al., Reference Paz, Orlitsky, Roth-Hanania, Zahn-Waxler and Davidov2021). Applying this notion and empirical findings to the current study, the intergenerational influences of maternal childhood adversity may surface as internalizing problems for girls and externalizing problems for boys. On the other hand, the gendered patterns of behavioral norms have become more fluid, as evidenced by increased reports of early onset of externalizing behavior among girls (Fontaine et al., Reference Fontaine, Carbonneau, Vitaro, Barker and Tremblay2009). Consistently, the cooccurrence of internalizing and externalizing problems has been reported for both girls and boys in the presence of maternal stressors, such as maternal depression (Wang & Yan, Reference Wang and Yan2019). These findings signal less prominent gender differences.
Further, gender differences in the intergenerational influences of maternal childhood adversity may have age-varying associations with children’s mental health across childhood and adolescence. During adolescence, social expectations of conformation to gendered behavior intensify (Hill & Lynch, Reference Hill, Lynch, Brooks-Gunn and Peresen1983), children’s self-endorsement of gendered norms begins to solidify (Kågesten et al., Reference Kågesten, Gibbs, Blum, Moreau, Chandra-Mouli, Herbert and Amin2016), and gendered patterns in internalizing and externalizing problems surface more clearly (Gutman & Codiroli McMaster, Reference Gutman and Codiroli McMaster2020). Similarly, it has been posited that boys’ maladjustment tends to emerge during early childhood, whereas girls’ mental health problems tend to increase during adolescence, along with the onset of puberty (Hayward, Reference Hayward2003; Martel, Reference Martel2013), although findings are not entirely consistent (Dimler & Natsuaki, Reference Dimler and Natsuaki2015; Ullsperger & Nikolas, Reference Ullsperger and Nikolas2017). As such, the influences of risk factors, such as maternal childhood adversity, on children’s mental health may vary across genders more prominently during adolescence. In general, gender differences in the influence of adversities on mental health have received limited empirical attention (Leban & Gibson, Reference Leban and Gibson2020). None of the within-generation studies examining the importance of timing of exposure to childhood adversity (Atzl et al., Reference Atzl, Narayan, Rivera and Lieberman2019; Nelson & Gabard-Durnam, Reference Nelson and Gabard-Durnam2020; Schalinski et al., Reference Schalinski, Teicher, Nischk, Hinderer, Muller and Rockstroh2016; Schroeder et al., Reference Schroeder, Slopen and Mittal2020; Yoon, Reference Yoon2020) examined gender differences. Relevant empirical evidence is even more limited regarding gender differences in the intergenerational influences of maternal childhood adversity on children’s mental health, with one exception (Letourneau et al., Reference Letourneau, Dewey, Kaplan, Ntanda, Novick and Thomas2019)—maternal childhood adversity influenced internalizing and externalizing problems at age 2 via mothers’ mental health during prenatal and postpartum years only among boys. No identified studies have evaluated whether gender differences in the intergenerational impact of maternal childhood adversity on children’s mental health vary across children’s developmental periods.
Current study
A robust body of literature has documented the deleterious influences of childhood adversity on later mental health. An emerging body of literature has increasingly reported that the influences of maternal childhood adversity may extend into the next generation, with a few studies examining possible mechanisms underlying these intergenerational influences. However, prior studies typically focused on factors underlying intergenerational influences in early childhood or a single developmental period. As such, another question that can further explicate the intergenerational influences of maternal childhood adversity experiences on children’s mental health has been overlooked—the question of timing. Similarly, possible moderating effects by gender have received little empirical attention in the relevant literature, despite differences in the developmental nature of mental health across genders and formation as well as solidification of gendered norms about behaviors across developmental epochs. Applying a developmental lens to possible gender differences has been even rarer. Expanding these lines of inquiry will enhance the field’s ability to locate whom to prioritize and when to intervene to disrupt the intergenerational influence of childhood adversity.
To address these gaps in the scientific literature, the current study focused on two central research aims. First, it tested maternal childhood adversity experiences on children’s internalizing and externalizing problems from ages 4.3 to 17.6 using time-varying effect models (TVEMs) to examine fluctuations in intergenerational effects of maternal childhood adversity on children’s mental health over time. We hypothesized that the negative influences of maternal childhood adversity on children’s mental health may become more prominent during childhood rather than adolescence. Second, moderation TVEMs were evaluated to examine whether the intergenerational influences of maternal childhood adversity experiences and their developmental inflection timing regarding their children differ by the child’s gender. We hypothesized that gender differences emerge more clearly during adolescence. Considering mixed empirical evidence on whether there will be gender differences in types of children’s maladjustment (i.e., internalizing problems vs. externalizing problems), we did not formulate a directional hypothesis regarding types of children’s maladjustment.
Method
Study design and sample
The Young Women and Child Development Study is a longitudinal study examining family process and developmental outcomes of two community cohorts of adolescent mothers and their children (Lee et al., Reference Lee, Gilchrist, Beadnell, Lohr, Yuan, Hartigan and Morrison2017). Recruitment of participants occurred in health and social services agencies in three urban counties in a northwest region of the United States (Oxford et al., Reference Oxford, Lee and Lohr2010). Eligibility criteria included: (a) younger than 18 years old at the time of enrollment, (b) unmarried, (c) intention to bear and parent the child, and (d) ability to speak English. Data collection began in 1988 for Cohort 1 (C1, n = 240) and 1992 for Cohort 2 (C2, n = 255) and concluded for both cohorts in 2007. At the initial interview, the average age of mothers was 16.07 years (SD = 1.01), 71.5% reported no prior pregnancy, 81% reported public assistance as their main source of income, and they reported 9.31 (SD = 1.30) years of schooling. No significant differences by cohort existed in racial and ethnic composition (χ2[1] = 2.541, p = .111), average age at intake (t[493] = 0.775, p = .439), pregnancies prior to the one at intake (χ2[1] = 0.005, p = .942), and having mothers without a high school diploma, a proxy measure for socioeconomic status in the family of origin (χ2[1] = 0.799, p = .371). Sample retention rates were consistently high across study years, averaging 94.6% for C1 and 83.7% for C2. The sample was racially and ethnically diverse (50.1% White, 24.2% Black, 6.3% Hispanic, 5.3% Native American, 4.2% Asian or Pacific Islander, 4.8% mixed Black and White, and 5.1% other or unknown).
The current analysis utilized 11 age points between ages 4.3 (SD = 0.2) and 17.6 (SD = 0.1) that were collectively provided by the two cohorts—seven waves from each cohort including C1 covering ages 5.9–17.6 and C2 covering ages 4.3–14.1. There were 1.5-year gaps between ages 4.5 and 6 and ages 13.5 and 15. There was a 2.4-year gap between ages 7.1 and 9.5. The rest were a year apart. The differences in time spacing between assessment points were handled by modeling participants’ age as “time.” The TVEM leveraged the age coverage collectively provided by two cohorts and modeled the change in outcomes and the varying influence of the independent variable over this age span. Prior to age 4.3, the Child Behavior Checklist, a measure to assess children’s mental health, was not used. A total of 2,190 records from 361 children who had responses to mental health measures for at least one assessment point constituted the final analysis sample. Children who were not included in the analysis (n = 134) were not different than those included based on gender, age, race, and cohort (p > .05). Among the 361 children included in the analysis, 42.4% (n = 153) were girls, 33.5% (n = 121) were White, 25.5% (n = 92) were Black, 11.9% (n = 43) were Hispanic, 2.5% (n = 9) were Native American, 1.7% (n = 6) were Asian or Pacific Islander, 13% (n = 47) were mixed (Black and White), and 11.9% (n = 43) were other races and ethnicities.
Measures
Maternal childhood adversity
Mothers’ childhood adverse experiences were assessed using items informed by the original Adverse Childhood Experiences study (Anda et al., Reference Anda, Whitfield, Felitti, Chapman, Edwards, Dube and Williamson2002) and the emerging literature suggesting the need to add more items assessing other adversity constructs (Afifi, Reference Afifi, Asmundson and Afifi2020). As shown in Table 1, nine items were used to represent mothers’ childhood adversity: (a) physical abuse (Did parents ever throw something at you, push, grab shove, or slap you?); (b) sexual abuse (Have you ever been forced to have sexual intercourse against your will?); (c) emotional abuse (Have you ever been put down by your parents?); (d) foster care experience; (e) food insecurity (How often have you worried about having enough food for yourself?); (f) parental divorce (Were your parents divorced?); (g) parental alcohol use (Did you ever live with an alcoholic parent or parent figure?); (h) death of a parent; and (i) parental arrest (Were your parents arrested?). Maternal childhood adversity was assessed prior to the maternal age 19.5 assessment except for three retrospective items asking about physical abuse, parental substance use, and being in foster care in childhood for C1 and one retrospective item asking about sexual abuse in childhood for C2. Mothers were also asked to report about their experiences between assessments, capturing mothers’ experiences prior to age 18.5. When mothers positively endorsed an adversity item in these assessments, the given item was coded as 1, indicating that mothers experienced that adversity at a given data point. Each item was coded as 0 (no) versus 1 (yes) and summed to create a total maternal childhood adversity score, which ranged from 0 to 8.
Table 1. Maternal childhood adversity constructs and measures

Child behavior
Children’s internalizing and externalizing behaviors were assessed using the Child Behavior Checklist (Achenbach, Reference Achenbach1991). The checklist contains 118 items that measure internalizing (e.g., withdrawn) and externalizing (e.g., aggressive behavior) problems for children aged 4–18. Items were anchored with a 3-point Likert scale (0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true). Total raw scores of internalizing (α = .75–.89) and externalizing (α = .84–.94) symptoms were used.
Covariates
Covariates included gender (0 = male, 1 = female), race (0 = White, 1 = non-White), grandmother’s education (1 = less than seventh grade to 7 = graduate or professional training) and cohort (C1 vs. C2).
Analysis
TVEMs were employed to assess the time-varying relationship between maternal childhood adversity and children’s mental health problems across the children’s developmental period. TVEM is an extension of spline regression that allows an estimated association between the time-varying dependent variable and independent variables. Independent variables can be either time varying (i.e., values of independent variables vary) or time invariant (i.e., values of independent variables do not vary)—values of independent variables may or may not vary, but the effect of those independent variables on the dependent variable differs across time. TVEM does not require specification of the shape of the curve beforehand (i.e., linear, quadratic, or cubic; Tan et al., Reference Tan, Shiyko, Li, Li and Dierker2012), which leverages the age coverage provided by two cohorts and allows for estimation of more complex time-varying effects of maternal childhood adversity on children’s mental health outcomes across the children’s multiple developmental epochs.
In the current analysis, TVEMs were estimated for each child’s internalizing and externalizing scores in the following steps. First, to evaluate the fluctuation in the association between maternal childhood adversity and children’s mental health problems from ages 4.3 to 17.6, the intercept, maternal childhood adversity, and gender were included to assess their time-varying effects with the P-spline estimation method. Following the established guideline (Tan et al., Reference Tan, Shiyko, Li, Li and Dierker2012), participants’ age was modeled as “time.” With the number of knots set at 10, the age interval was split into 10 equal intervals and a lower-order polynomial curve was fitted in each interval to estimate the age-varying effect (Tan et al., Reference Tan, Shiyko, Li, Li and Dierker2012). Second, interaction TVEMs were estimated with the product term between maternal childhood adversity and child’s gender. All models were adjusted for children’s gender, race, grandmother’s education, and cohort, assuming time-invariant values and effects. Areas in Figures 1 and 2 with mean curves of the coefficients where 95% confidence intervals do not overlap with 0 indicate statistically significant effects at p < .05. All participants with data on the Child Behavior Checklist from at least one wave were included in the analyses. All TVEMs were done with the TVEM SAS macro (Li et al., Reference Li, Dziak, Tan, Huang, Wagner and Yang2017; Methodology Center, 2017).

Figure 1. Intercept-only models of offspring’s (a) internalizing and (b) externalizing problems from ages 4.53 to 17, with 95% confidence intervals.
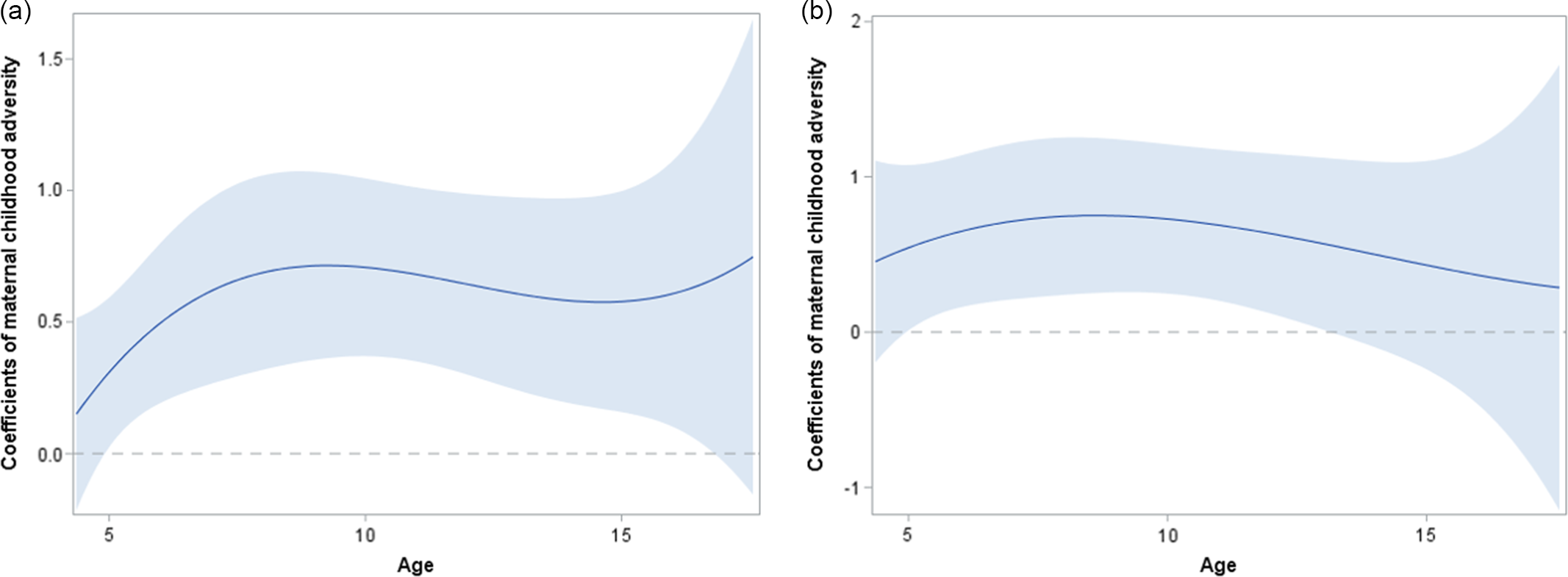
Figure 2. Time-varying main effect of maternal childhood adversity on offspring’s (a) internalizing and (b) externalizing problems from ages 4.53 to 17, with 95% confidence intervals. The central line shows the point estimate of the coefficient and the gray ribbon shows the 95% confidence interval. Areas where 95% confidence intervals do not overlap with 0 (dashed line) indicate statistically significant effects at p < .05. Models are adjusted for gender, race, grandmother’s education, and cohort.
Results
Descriptive statistics for the variables are shown in Table 2. Item-level frequencies showed that 97% of teen mothers reported experiencing at least one childhood adversity and 47.2% of teen mothers reported experiencing four or more types of adversities in childhood. Children’s internalizing problem scores ranged from 5.8 (SD = 5.11) to 9.98 (SD = 5.61) and their externalizing problem scores ranged from 9.16 (SD = 8.17) to 15.95 (SD = 8.74) over time. The means of t-scores were 52 (SD = 10.2) for internalizing and 55.4 (SD = 10.3) for externalizing problems, suggesting that on average, the scores are right below the borderline clinical range (t-scores ≥ 60). Intercept-only (unconditional) models of internalizing problems showed that the average internalizing scores had two “growth periods”—from 6.2 (age 5) to 7.5 (age 9) and from 6.8 (age 13) to 8.0 (age 15). The growth was steeper in the second period (Figure 1a). In contrast, externalizing problems showed a steady decreasing pattern, from 17.4 at age 5 to 12.7 at age 17 (Figure 1b).
Table 2. Descriptive statistics of analysis variables (N = 361)
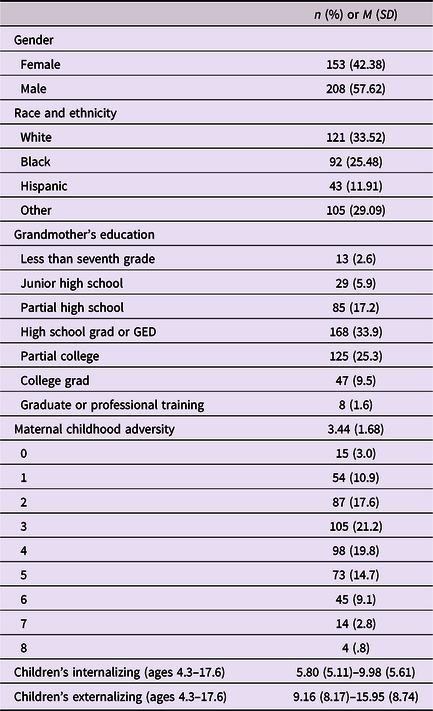
Time-varying effects of maternal childhood adversity on children’s internalizing and externalizing problems from childhood to adolescence
Increased maternal childhood adversity was associated with higher internalizing scores during the study assessment period, from age 5 (b = 0.34, 95% CI = 0.03, 0.65) to age 16 (b = 0.63, 95% CI = 0.13, 1.14; Figure 2a). The intergenerational impact of maternal childhood adversity increased until children were age 8 or 9 (b = 0.75, 95% CI = 0.37, 1.13) and then remained at a similar level until age 16 (highest: b = 0.76, 95% CI = 0.40, 1.12 at age 10; lowest: b = 0.62, 95% CI = 0.20, 1.05 at age 15). Maternal childhood adversity was also associated with increased externalizing problems between ages 5 and 13 (Figure 2b). As with children’s internalizing problems, the intergenerational influence of maternal childhood adversity showed an increasing pattern from age 5 (b = 0.66, 95% CI = 0.10, 1.22) to age 8 (b = 0.87, 95% CI = 0.33, 1.41), but then diverged from the pattern observed for internalizing problems and gradually decreased thereafter.
Time-varying maternal childhood adversity and gender interactions
To examine whether the intergenerational influences of maternal childhood adversity and their developmental inflection timing differed by gender, we created an interaction term between maternal childhood adversity and gender and added it to the main effects models for internalizing and externalizing problems. As with the main effects models, the possible age range for all gender interaction effects was 4.3–17.6 years.
Results revealed that the influences of maternal childhood adversity on children’s internalizing problems differed by gender, particularly between age 11.5 (interaction: b = 0.68, 95% CI = 0.03, 1.32) and age 14.8 (interaction: b = 0.89, 95% CI = 0.14, 1.65; Figure 3, shaded area). To illustrate the moderation interaction, Figure 3 shows the effect of maternal childhood adversity on children’s internalizing problems for girls and boys. For girls, the effect of maternal childhood adversity on internalizing problems was statistically significant for most of the assessment period (from ages 7.3 to 16.7)—the effect showed a steady increase from age 7.3 (b = 0.57, 95% CI = 0.01, 1.13) until 14.5 (b = 1.11, 95% CI = 0.46, 1.76), and then declined thereafter yet remained statistically significant. For boys, the impact of maternal childhood adversity on internalizing problems was statistically significant for a shorter period—the effect started emerging at age 5.3 (b = 0.39, 95% CI = 0.03, 0.75) and leveled off at age 7.3 (b = 0.69, 95% CI = 0.22, 1.16); maternal childhood adversity became irrelevant after age 11 (b = 0.38, 95% CI = −0.01, 0.77) for boys (Figure 3). In contrast, results from the interaction TVEM for externalizing problems reveal no gender moderation effect (ranging from b = −1.88 [95% CI = −4.5–0.73] to b = .82 [95% CI = −0.38–2.03]).

Figure 3. Time-varying interaction effect between maternal childhood adversity and gender on offspring’s internalizing problems from ages 4.53 to 17, with 95% confidence interval, by gender. Line shows the point estimate of the coefficient by gender. The shaded area indicates the estimates between genders are statistically significantly different than each other between ages 11.5 and 14.8 for internalizing problems (p < .05). Models are adjusted for race, grandmother’s education, and cohort.
Discussion
The primary goals of the current study were to understand better how maternal childhood adversity predicts children’s internalizing and externalizing problems from early childhood to late adolescence and the extent to which these intergenerational relations may differ by children’s gender. The effect of maternal childhood adversity experiences on children’s mental health increased from ages 5 to 8. This effect was maintained until age 13 for both internalizing and externalizing problems and then remained a statistically significant predictor for internalizing problems until age 16. The detected intergenerational influences on children’s mental health from childhood to adolescence in our study are consistent with prior studies (Stargel & Easterbrooks, Reference Stargel and Easterbrooks2020; Stepleton et al., Reference Stepleton, Bosk, Duron, Greenfield, Ocasio and MacKenzie2018), adding to the few existing studies examining the intergenerational influences of childhood adversity on children’s mental health beyond early childhood (Doi et al., Reference Doi, Fujiwara and Isumi2021; Schickedanz et al., Reference Schickedanz, Halfon, Sastry and Chung2018). Further, consistent with the life course perspective, particularly the notion of a critical or sensitive period (Ben-Shlomo & Kuh, Reference Ben-Shlomo and Kuh2002; Braveman & Barclay, Reference Braveman and Barclay2009; Nelson & Gabard-Durnam, Reference Nelson and Gabard-Durnam2020), the current study revealed a developmental inflection point when maternal childhood adversity rapidly gains salience, from ages 5 to 8, extending the relevant body of literature in an important direction.
The developmental period spanning ages 5 to 8 represents a period when externalizing behavior problems deescalate from their moderately elevated level in infancy and toddlerhood (Miner & Clarke-Stewart, Reference Miner and Clarke-Stewart2008) and internalizing problems remain relatively low (Nivard et al., Reference Nivard, Lubke, Dolan, Evans, St. Pourcain, Munafò and Middeldorp2017). As hypothesized in the current study, the negative impacts of a risk factor, namely maternal childhood adversity, appeared to emerge more prominently during developmental periods when externalizing (Miner & Clarke-Stewart, Reference Miner and Clarke-Stewart2008) and internalizing (Nivard et al., Reference Nivard, Lubke, Dolan, Evans, St. Pourcain, Munafò and Middeldorp2017) problems are expected to be low. However, partially refuting our hypothesis, the intergenerational influences did not appear to attenuate after an initial increase during the developmental inflection point of ages 5–8, particularly for internalizing problems. Rather, the intergenerational influences tended to remain steady during later childhood and through adolescence for internalizing problems. For externalizing problems, the intergenerational influences remained steady until early adolescence and then showed a gradual decreasing pattern, partially supporting our hypothesis that intergenerational influences may attenuate during adolescence. These findings collectively suggest that the developmental span from ages 5 to 8 may represent a critical intervention window when intergenerational influences of maternal childhood adversity on children’s mental health can be disrupted during childhood and adolescence.
Furthermore, the developmental period spanning ages 5–8 represents a period of transition to primary schooling. This transition period features dynamic changes and exciting opportunities in children’s lives (Hanke et al., Reference Hanke, Backhaus, Bogatz, Dogan, Dockett, Griebel and Perry2017), but also triggers and necessitates adjustments by the entire family, bringing challenges and thus, representing a potentially stressful period for parents (DeCaro & Worthman, Reference DeCaro and Worthman2011). Stressors during this transition period may function as an added risk burden for mothers with preexisting stressors—namely, their own childhood adversity—further exacerbating struggles with psychological distress and parenting behaviors that already have been compromised due to their early childhood adversity (Doi et al., Reference Doi, Fujiwara and Isumi2021). In addition, teen mothers are often confronted with struggles throughout their life course (Boden et al., Reference Boden, Fergusson and Horwood2008; Easterbrooks et al., Reference Easterbrooks, Chaudhuri, Bartlett and Copeman2011), including low socioeconomic resources (Oxford et al., Reference Oxford, Lee and Lohr2010), which may further deepen the challenging nature of this period of transition to primary schooling, amplify the burden of psychological distress among teen mothers with childhood adversity, and eventually affect children’s mental health.
The results from gender interaction TVEMs reveal a more nuanced developmental process by gender—maternal childhood adversity was a statistically significant predictor for internalizing problems until age 11 regardless of the child’s gender, and it remained statistically significant for girls’ internalizing problems until age 16. However, for boys, the association was no longer statistically significant after age 11. Such gender differences were particularly prominent from ages 11.5 to 14.8. For externalizing problems, maternal childhood adversity was a statistically significant predictor until age 13, regardless of gender. These results partially support our hypothesis that gender differences emerge most prominently during adolescence when children are increasingly expected to conform to gendered behavior (Hill & Lynch, Reference Hill, Lynch, Brooks-Gunn and Peresen1983) and endorse gendered norms (Kågesten et al., Reference Kågesten, Gibbs, Blum, Moreau, Chandra-Mouli, Herbert and Amin2016) and gender differences in internalizing and externalizing problems emerge more substantially (Gutman & Codiroli McMaster, Reference Gutman and Codiroli McMaster2020). Some studies have shown that factors embedded in ecological contexts other than the family, such as peer influence, have stronger effects on externalizing than internalizing behaviors (Fortuin et al., Reference Fortuin, van Geel and Vedder2015), offering a potential explanation for why maternal childhood adversity ceased exerting an impact on externalizing problems earlier than it did for internalizing problems. Our study findings also suggest that maternal childhood adversity may exert more influences on youth mental health among girls than boys, because the intergenerational influences remained longer for girls’ internalizing problems. It has been reported that the boys are more influenced by their friends and less influenced by their parents, compared to girls (Cutrín et al., Reference Cutrín, Gómez-Fraguela, Maneiro and Sobral2017), potentially offering an explanation for why the predictive capacity of maternal childhood adversity was less prominent for boys. The current study findings appear to contradict a prior study that reported the intergenerational effects of maternal childhood adversity on externalizing problems only for boys (Letourneau et al., Reference Letourneau, Dewey, Kaplan, Ntanda, Novick and Thomas2019). However, the prior study covered age 2, whereas the current study covered ages 4.3–17.6. The differences in developmental periods examined may have contributed to such discrepancies observed across studies, suggesting gender differences may emerge differently in infancy and toddlerhood versus preschool years and beyond and thus, emphasizing the importance of deploying a development lens in relevant studies.
Further, the negative effect of maternal childhood adversity did not manifest in a particular form for girls (i.e., internalizing problems) and boys (i.e., externalizing problems), refuting gendered strain theory (Broidy & Agnew, Reference Broidy and Agnew1997) and the gender socialization hypothesis (Chodorow, Reference Chodorow1978). It is particularly noteworthy that the current findings indicate the need to develop practice strategies for effectively screening and addressing boys’ internalizing problems (Davis et al., Reference Davis, Votruba-Drzal and Silk2015; Sterba et al., Reference Sterba, Prinstein and Cox2007), which have received less attention in empirical discussions and practical considerations due to relatively low prevalence rates compared to girls. Conversely, it is also noteworthy that our study findings indicate the need to develop intervention strategies tailored for girls’ externalizing problems (Habersaat et al., Reference Habersaat, Boonmann, Schmeck, Stéphan, Francescotti, Fegert and Urben2018), which similarly have received less attention due to relatively low prevalence rates compared to boys.
Limitations and strengths
The current findings should be contextualized by the study’s methodological limitations. First, the study relied on a community sample of teen mothers and their children in a northwest region of the United States. However, the general developmental trend of broadband ratings of internalizing and externalizing problems in our study sample is similar to those in other general community samples of children, with internalizing problems showing an increasing trend (Davis et al., Reference Davis, Votruba-Drzal and Silk2015; Flouri et al., Reference Flouri, Ruddy and Midouhas2017; Olson et al., Reference Olson, Choe and Sameroff2017) and externalizing problems showing a decreasing trend (Fanti & Henrich, Reference Fanti and Henrich2010; Flouri et al., Reference Flouri, Ruddy and Midouhas2017), including high-risk samples, such as welfare system-involved children (Mowbray et al., Reference Mowbray, Jennings, Littleton, Grinnell-Davis and O’Shields2018; Yoon et al., Reference Yoon, Yoon, Wang, Tebben, Lee and Pei2017), easing the concern of generalization to some degree. Nevertheless, given the specificity of our sample, generalization of the current study findings to the general population should be done cautiously. Second, all measures relied on mothers’ self-report, which may introduce bias in estimating children’s mental health problems, particularly internalizing problems (Müller et al., Reference Müller, Romer and Achtergarde2013). The issue of shared method variance across measures also might have influenced findings. Third, similar to existing studies on teen parents (Mollborn & Lovegrove, Reference Mollborn and Lovegrove2011), teen fathers’ experiences were not reflected. Although relatively higher influences of maternal childhood adversity on child developmental outcomes have been observed, compared to the influences of paternal childhood adversity (Folger et al., Reference Folger, Eismann, Stephenson, Shapiro, Macaluso, Brownrigg and Gillespie2018; Schickedanz et al., Reference Schickedanz, Halfon, Sastry and Chung2018), clarifying the unique and joint influences of maternal and paternal experiences of childhood adversity represents an important next step in this line of inquiry. Fourth, the study sample included mostly White and Black participants. It is imperative to understand the experiences of other ethnic and racial groups, specifically Latinx children born to young Latina mothers—teen pregnancy rates are disproportionately concentrated in this group in the United States (U.S. Department of Health & Human Services, 2018). Fifth, the data collection concluded in 2007, which may not accurately reflect today’s developmental setting. Particularly, the gendered patterns of behavioral norms might have become more fluid. The gendered patterns—conceptually predicted by gendered strain theory (Broidy & Agnew, Reference Broidy and Agnew1997) and the gender socialization hypothesis (Chodorow, Reference Chodorow1978) and empirically evidenced by elevated internalizing problems among girls (Carter et al., Reference Carter, Godoy, Wagmiller, Veliz, Marakovitz and Briggs-Gowan2010; Gutman & Codiroli McMaster, Reference Gutman and Codiroli McMaster2020) and externalizing problems among boys (Castelao & Kröner-Herwig, Reference Castelao and Kröner-Herwig2014; Paz et al., Reference Paz, Orlitsky, Roth-Hanania, Zahn-Waxler and Davidov2021)—may be less prominent in more recent data. Our findings do not follow such patterns. As previously noted, the general trends in broadband ratings of internalizing and externalizing problems in our sample are similar to other studies with other samples of children. These considerations ease the concern that the timing of data collection may introduce biases to the estimation to some degree. Finally, the Child Behavior Checklist, an assessment tool for children’s mental health, was not used prior to age 4.3. Considering that the association between maternal childhood adversity and mental health was observed at earlier ages (Greenfield et al., Reference Greenfield, Williams-Butler, Pirozzolo Fay, Duron, Adlin Bosk, Stepleton and Mackenzie2019; Stepleton et al., Reference Stepleton, Bosk, Duron, Greenfield, Ocasio and MacKenzie2018), particularly externalizing problems (Greenfield et al., Reference Greenfield, Williams-Butler, Pirozzolo Fay, Duron, Adlin Bosk, Stepleton and Mackenzie2019), extending the assessment period into infancy and toddlerhood will be a fruitful future direction to further clarify when the intergenerational impacts of maternal childhood adversity prominently emerge.
Despite its limitations, the present study extended prior studies in three meaningful ways. First, to our best knowledge, the current study is the first to examine a developmental inflection point when the intergenerational impacts of maternal childhood adversity on children’s mental health prominently emerge and revealed that ages 5–8, the period of transition into official schooling, may represent a critical intervention window for mental health problems among children born to teen mothers. Second, by leveraging data from longitudinal studies of teen mothers and their children, the current study expanded the assessment period from a heavy focus on infancy and early childhood or a single developmental period in existing studies to cover multiple developmental epochs from ages 4.3 to 17.6. The repeated and prospective nature of the current data enabled us to focus on within-person variability, which is critical to locate a developmental inflection point of a given risk factor for children’s mental health. Finally, to our best knowledge, the current study represents the first empirical inquiry examining time-varying effects of gender differences in intergenerational influences of maternal childhood adversity on the next generation’s mental health. Our study findings reveal that maternal childhood adversity may function as a distal risk source for not only internalizing but also externalizing problems, particularly among girls. By expanding the relevant body of literature in these three important ways, the current study advances the field’s capacity to address the questions of when and among whom to intervene to disrupt the intergenerational influences of maternal childhood adversity on children’s mental health and enhances the ability to tailor intervention strategies for children born to teen mothers. No identified studies appear to incorporate these unique strengths.
Implications
Our novel findings reveal that ages 5–8, the period of transition into primary schools, may represent a developmental inflection point when the intergenerational influences of maternal childhood adversity start emerging more substantially. Once elevated, the impacts of maternal childhood adversity on internalizing and externalizing problems remained steady, particularly for girls. From the perspective of developmental science, the current study findings highlight the importance of applying a development lens and considering the specific developmental period of children when examining the intergenerational influences of maternal adversity. In some prior studies, maternal distress, for example, was not a significant factor regarding the influences of maternal adversity on child developmental outcomes in childhood (Esteves et al., Reference Esteves, Gray, Theall and Drury2017), whereas it was a significant mediator of child developmental outcomes in adolescence (Doi et al., Reference Doi, Fujiwara and Isumi2021). Differences in developmental timing might explain these observed discrepancies in the findings. Reflecting on current findings, explicating factors that underlie the association between maternal childhood adversity and children’s mental health during the period of transition into primary schools might be a fruitful research direction to strengthen the relevant developmental science base. Regarding practice, the current findings indicate that the period of transition into primary school may be a critical intervention point to prevent maternal childhood adversity from functioning as a distal risk source compromising the next generation’s mental health. Locating intervention points other than the prenatal period is particularly important for young and low-income women and their children. The support for a multigenerational approach in pediatric settings (Cheng & Solomon, Reference Cheng and Solomon2014) to account for maternal history of childhood trauma is growing (Hagan et al., Reference Hagan, Shaw and Duncan2017), suggesting that maternal history of trauma should be added to prenatal assessment profiles (Racine et al., Reference Racine, Madigan, Plamondon, Hetherington, McDonald and Tough2018; Sun et al., Reference Sun, Patel, Rose-Jacobs, Frank, Black and Chilton2017). The importance of screening for maternal risks has been highlighted for the prenatal period (Goyal et al., Reference Goyal, Gay and Lee2010). The majority of intervention efforts for teen mothers have typically focused on the pre- and postnatal periods (e.g., Barlow et al., Reference Barlow, Mullany, Neault, Goklish, Billy, Hastings and Walkup2015; Cox et al., Reference Cox, Harris, Conroy, Engelhart, Vyavaharkar, Federico and Woods2019), including the widely implemented Nurse Family Partnership program (Miller, Reference Miller2015). The importance of the pre- and postnatal periods is inarguable. However, many young and low-income women receive late, inadequate, or no prenatal care compared to older pregnant women (Child Trends Databank, 2015; Sidebottom et al., Reference Sidebottom, Hellerstedt, Harrison and Jones-Webb2017; Taylor et al., Reference Taylor, Alexander and Hepworth2005). Our study findings suggest that the period of transition into primary schools should be considered as an additional developmental point for screening maternal history of childhood adversities. Providing interventions that have shown promising results in reducing mental health problems in school-aged children, such as Parent Management Training (Kazdin, Reference Kazdin1997) and the Incredible Years initiative (Leijten et al., Reference Leijten, Raaijmakers, Orobio de Castro, van den Ban and Matthys2017), may disrupt the intergenerational influences of maternal childhood adversity on children’s mental health problems. Considering the varied accessibility of providers who are trained in these interventions, effective elements of these interventions can be deployed by providers to support families experiencing these challenges (Chorpita et al., Reference Chorpita, Daleiden and Collins2014) to increase parenting skills and efficacy and reduce potential impacts of maternal childhood adversity on mental health problems in children.
Conclusions
In conclusion, our study findings suggest that the developmental period from ages 5 to 8 should be considered as an additional developmental point when maternal childhood adversity should be considered in pediatric settings. This developmental period may represent another crucial junction point, in addition to the pre- and postnatal periods, to work with young and low-income mothers, particularly those who received no prenatal care, to disrupt the impacts of maternal childhood adversity on the next generation’s mental health and thus, promote healthy development among children born to young mothers.
Acknowledgements
We would like to extend our gratitude to YCDS study participants for their contribution to the study.
Funding statement
This study was supported by grants HD097379 from National Institute of Child Health and Human Development, DA05208 from National Institute on Drug Abuse, and MH52400 and MH56599 from National Institute of Mental Health. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. The funding agencies played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit this article for publication.
Conflicts of interest
None.








