Introduction
High rates of metabolic syndrome, ranging from 29% to 35%, are observed in patients with schizophrenia.Reference Mitchell, Vancampfort and Sweers1 The characteristic clinical and metabolic findings, comprising central obesity, dyslipidemia, hypertension, and insulin resistance, are associated with a significant increased risk of cardiovascular morbidity and mortality1–3 as well as cognitive impairment.Reference Bora, Akdede and Alptekin4, Reference Grover, Padmavati and Sahoo5 In a meta-analysis of randomized clinical trials and observational studies in schizophrenia (N = 29 596 patients), the prevalence of metabolic syndrome (MetS) was 33%, representing 1.9-fold increased odds for developing MetS compared to the general population.Reference Vancampfort, Stubbs and Mitchell6 In an analysis of baseline data from the CATIE study (N = 689 patients), significantly higher rates of metabolic syndrome were observed (vs matched controls) for both men (36.0% vs 19.7%; P < .001) and women (51.6% vs 25.1%; P < .001).Reference McEvoy, Meyer and Goff7
The extent to which the diagnosis of schizophrenia is associated with a metabolic syndrome diathesis, independent of exposure to antipsychotic therapy, has not been fully determined. Some evidence suggests that drug-naïve patients with schizophrenia may represent an at-risk group with higher rates of diabetes, impaired glucose tolerance, increased insulin resistance, elevated lipid levels, and obesity.Reference Ryan, Collins and Thakore8–Reference Saddichha, Manjunatha and Ameen14 Nonetheless, evidence is strong indicating that antipsychotic treatment is associated with a marked increase in the rate of metabolic syndrome and its components.Reference Mitchell, Vancampfort and Sweers1, Reference Newcomer15
While antipsychotic treatment can significantly increase the odds of developing metabolic syndrome, there is extensive evidence of clinically and statistically significant differences in the magnitude of risk across individual antipsychotic medications.Reference Newcomer15, Reference Leucht, Leucht and Huhn16 Marked differences have been reported in the propensity for weight gain among atypical antipsychotic medications.13–20 In meta-analyses of clinical trials in schizophrenia, mean weight gain is highest for clozapine, olanzapine, and iloperidone; intermediate for quetiapine, risperidone, and paliperidone; and lowest for ziprasidone, aripiprazole, lurasidone, asenapine, and amisulpride.Reference Kirkpatrick, Miller and Garcia-Rizo13, Reference Newcomer17 Antipsychotics may also have differential effects on glucose regulation and lipid metabolism that are independent of body weight.21–23
Several studies have implicated activity at 5-HT2C and histamine H1 receptors as a potential mechanism underlying the effects of antipsychotics on lipids, glucose metabolism, and weight.Reference Reynolds and Kirk24, Reference Kroeze, Hufeisen and Popadak25 There are notable differences among atypical antipsychotic medications in the degree of affinity for these receptors, with olanzapine and clozapine being among the most active.Reference Reynolds and Kirk24 In contrast, lurasidone exhibits weak affinity for 5-HT2C receptors and no appreciable affinity for histamine H1 or muscarinic M1 receptors.Reference Ishibashi, Horisawa and Tokuda26
Lurasidone has demonstrated efficacy in short- and long-term clinical trials in patients with schizophrenia,27–34 with limited risk for weight gain and low rates of adverse metabolic effects.35–38 The objective of this analysis was to assess the odds of development of metabolic syndrome associated with lurasidone treatment of adult patients with schizophrenia. The results summarized here include data from double-blind, placebo-, or active-comparator-controlled short-term (6 week) and long-term (≥12 month) trials in the lurasidone schizophrenia clinical trials database and from open-label extension studies in the database in which patients were switched from other atypical antipsychotic agents to lurasidone.
Methods
This analysis included data from the following clinical trials: all three short-term placebo-controlled phase III trials that supported FDA approval of lurasidone for the treatment of patients with schizophrenia; two 12-month active-comparator-controlled double-blind studies; and the 6-month open-label extension to one of the short-term placebo-controlled studies and the 6-month open-label extension to one of the 12-month double-blind active-comparator studies (see Table 1). These studies were selected since they included data comprising all five of the NCEP ATP III criteria. The current analysis was limited to the subgroup of patients with blood samples obtained while fasting.
Table 1. Summary of Studies Included in this Metabolic Syndrome Analysis.

Patients were classified as having metabolic syndrome based on the 2005 revision of the NCEP ATP III criteriaReference Grundy, Cleeman and Daniels40 when any three of the following five criteria were met: elevated waist circumference (≥102 cm for men, ≥88 cm for women), elevated triglycerides (≥ 150 mg/dL), reduced high-density lipoprotein cholesterol (<40 mg/dL in men, <50 mg/dL in women), elevated blood pressure (systolic ≥130 mm Hg or diastolic ≥85 mm Hg), or elevated fasting glucose (≥100 mg/dL). In the current analysis, an NCEP ATP III criterion was not considered to be met if a patient had normal values for triglycerides, blood pressure, high-density lipoprotein (HDL), and/or glucose while receiving drug treatment for one or more of these parameters.
All study protocols were approved by an independent ethics committee or institutional review board, and written informed consent was provided by all patients before initiation of study procedures. All studies were conducted in accordance with the International Conference on Harmonization Good Clinical Practice guidelines and with the ethical principles of the Declaration of Helsinki.
Short-term studies
Patients enrolled in these three studies32–34 were aged 18 to 75 years, had a diagnosis of schizophrenia (based on DSM-IV/ DSM-IV-TR criteria), and were experiencing an acute exacerbation of psychotic symptoms. Key exclusion criteria were an acute or unstable medical condition, alcohol or other drug abuse or dependence within the past 6 months, evidence of a severe movement disorder, or imminent risk of suicide (as judged by the study investigator). Patients who met study entry criteria were randomized, double-blinded to 6 weeks of once-daily, fixed-dose treatment with lurasidone (40, 80, 120, or 160 mg/d) or placebo (Table 1).
Long-term studies
Study D1050237 (NCT00641745) was a 12-month, randomized, double-blind, safety study of flexibly dosed lurasidone (40-120 mg/d) compared with risperidone (2-6 mg/d) in clinically stable outpatients with schizophrenia.Reference Citrome, Cucchiaro and Sarma32 Study D1050234 (NCT00789698) was a 12-month, double-blind, relapse-prevention study of flexibly dosed lurasidone (40-160 mg/d) compared with quetiapine XR (200-800 mg/d; Table 1).Reference Loebel, Cucchiaro and Xu33
Extension studies with medication switch
Study D1050231-E (NCT00615433) was a 6-month extension study of open-label lurasidone that followed an initial 6-week, randomized, double-blind study of fixed-dose lurasidone (40 or 120 mg/d), olanzapine (15 mg/d), or placebo (Study D1050231).Reference Stahl, Cucchiaro and Simonelli39 The extension of Study D1050237-E (NCT00641745) was a 6-month extension study of open-label lurasidone (40-120 mg/d) that followed an initial 12-month, randomized, double-blind study of flexibly dosed lurasidone (40-120 mg/d) or risperidone (2-6 mg/d) (Study D1050237; Table 1).Reference Citrome, Cucchiaro and Sarma32
Statistical methods
Short-term studies
Patient-level data were pooled for the analyses of three similarly designed, double-blind, 6-week, phase III studies. The safety sample for each study utilized in this analysis consisted of patients who were randomly assigned to treatment and received ≥ 1 dose of study medication. Logistic regression analysis, adjusted for baseline metabolic syndrome status, using a last observation carried forward (LOCF) approach was performed to determine statistical significance for between-group differences in weight and metabolic outcomes. Safety evaluations included vital signs, weight, waist circumference measurements, and laboratory tests (including lipids and glycemic indices).
To provide a preliminary assessment of the benefit of lurasidone, in terms of treatment response (≥20% reduction from baseline in PANSS total score at LOCF endpoint vs placebo), and the risk of lurasidone treatment, in terms of clinically significant weight gain (≥7% weight gain from baseline to endpoint vs placebo), we calculated the likelihood to be helped or harmed (LHH) as the NNH/NNT ratio for the two short-term trials (NCT00615433 and NCT00790192) that included both a placebo and an active comparator drug (olanzapine and quetiapine XR).
Long-term studies
Data from two long-term, active-controlled studies of lurasidone in the treatment of adult patients with schizophrenia were analyzed separately due to differences in study design. Between-group differences (D1050237: lurasidone vs risperidone; D1050234: lurasidone vs quetiapine XR) were tested for significance using logistic regression analysis.
Extension studies with medication switch
Data from two open-label extension studies that included a medication switch to lurasidone were analyzed separately, due to differences in study design. The proportion of patients with metabolic syndrome was calculated at extension study baseline and extension study month 6. Patients who received continuous treatment with lurasidone were compared with patients who switched to lurasidone from olanzapine or risperidone. Patients randomly assigned to receive placebo in the acute phase of Study D1050231 were excluded from this analysis.
Results
Short-term studies: pooled analyses of metabolic syndrome
A total of 1457 patients were included in the safety population, of whom, 1203 patients had at least one postbaseline safety assessment and were included in this analysis. In the pooled short-term studies (N = 3; D1050229, D1050231, D1050233), patients received lurasidone (N = 852), olanzapine (N = 122), quetiapine XR (N = 119), or placebo (N = 364) for up to 6 weeks. Of the lurasidone-treated patients, 243 (28.5%), 246 (28.9%), 242 (28.4%), and 121 (14.2%) patients received 40, 80, 120, and 160 mg/d, respectively. Demographic and baseline clinical characteristics are summarized in Table 2.
Table 2. Demographic and Baseline Clinical Characteristics.
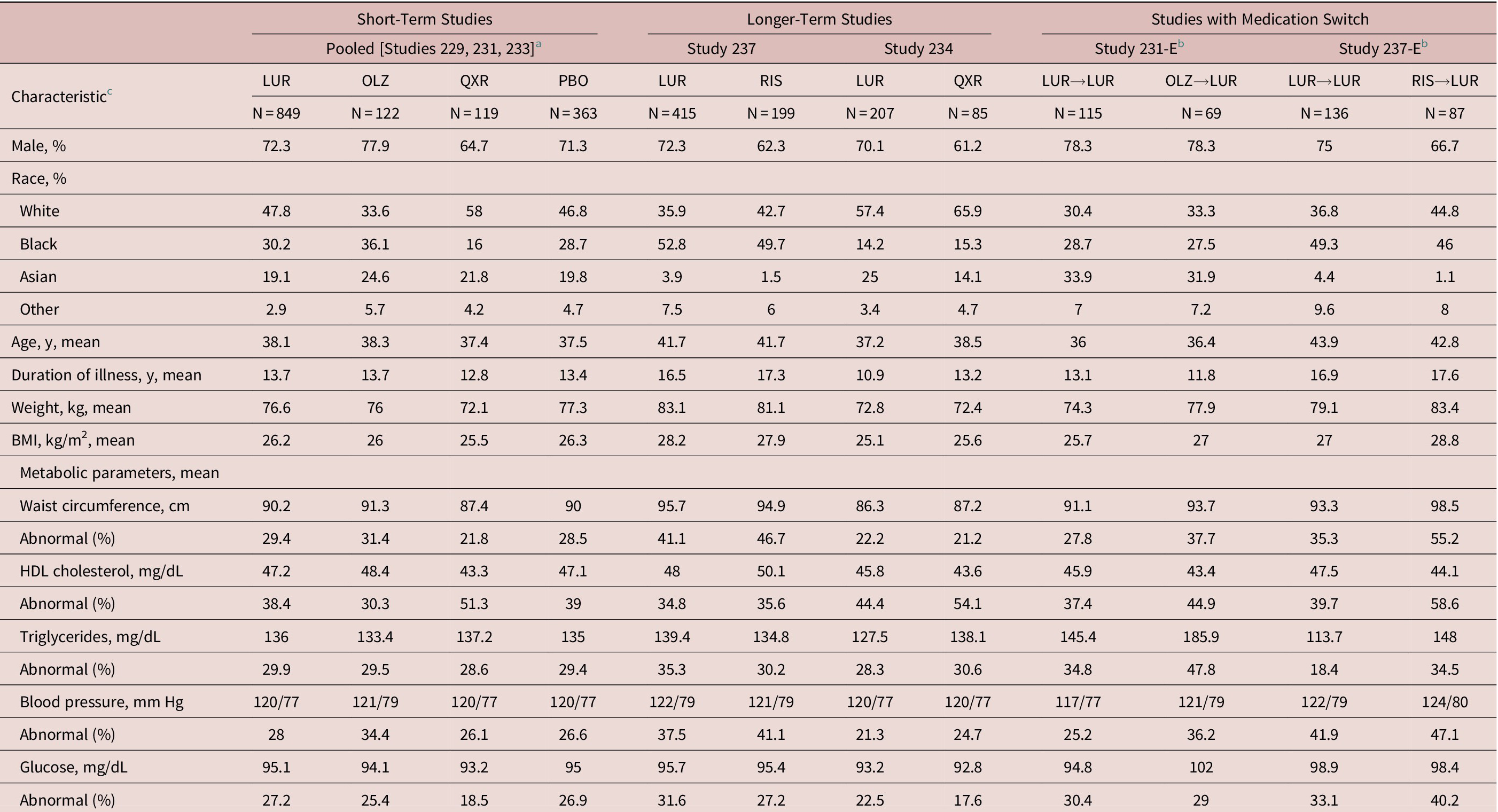
Abbreviations: BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LUR, lurasidone; OLZ, olanzapine; PBO, placebo; QXR, quetiapine; RIS, risperidone.
a Pooled for patients with metabolic syndrome data at baseline and ≥ 1 postbaseline assessment.29–31
b For the two switch studies,Reference Mattingly, Haddad and Tocco34, Reference Stahl, Cucchiaro and Simonelli39 data shown are for the open-label baseline following double-blind treatment, at the switch (or continuation) time-point.
c Sample sizes vary based on data availability.
d Abnormal criteria: elevated waist circumference (≥102 cm for men, ≥88 cm for women), elevated triglycerides (≥150 mg/dL), reduced HDL (<40 mg/dL in men, <50 mg/dL in women), elevated BP (systolic ≥130 mm Hg or diastolic ≥85 mm Hg), or elevated fasting glucose (≥100 mg/dL).
The proportion of patients meeting NCEP ATP III criteria for metabolic syndrome at baseline and week 6 (LOCF endpoint), respectively, was 21.6% and 23.4% for lurasidone, 21.3% and 36.3% for olanzapine, 16.0% and 37.4% for quetiapine XR, and 20.7% and 20.6% for placebo (Figure 1A). The odds of meeting NCEP ATP III criteria for metabolic syndrome at week 6 LOCF (adjusted for baseline metabolic syndrome status) was similar for the lurasidone and placebo groups (OR = 1.18; [95% CI, 0.81-1.71]; P = .39.), but the odds were significantly greater for olanzapine (OR = 2.81; [95% CI, 1.53-5.15]; P < .001) and quetiapine (OR = 3.49; [95% CI, 1.93-6.29]; P < .0001) vs placebo. The proportion of patients with metabolic syndrome at baseline compared to week 6 (LOCF) was 26.8% vs 28.1%, respectively, for lurasidone 40 mg/d, 22.4% vs 19.7% for 80 mg/d, 19.9% vs 21.7% for 120 mg/d, and 16.1% vs 24.1% for 160 mg/d. The odds of meeting criteria for metabolic syndrome at week 6 LOCF were similar for each dose level of lurasidone compared to placebo, with no significant, or trend significant, difference at any dose.

Figure 1. Metabolic syndrome status: pooled short-term studies.18–20 (A) Proportion of patients meeting metabolic syndrome criteria at baseline and week 6 (LOCF). (B) Proportion of patients without metabolic syndrome at baseline who met criteria for metabolic syndrome at week 6 (LOCF). Abbreviation: LOCF, last observation carried forward.
In patients who did not meet criteria for metabolic syndrome at baseline, the proportion who met criteria for metabolic syndrome at 6 weeks (LOCF) was significantly greater for the olanzapine (18.6%; P < .05) and quetiapine XR (24.3%; P < .01) groups compared with both the placebo (8.4%) and lurasidone (8.4%, combined doses; Figure 1B) groups. For lurasidone doses of 40 mg/d, 80 mg/d, 120 mg/d, and 160 mg/d, the proportion who met metabolic syndrome criteria at 6 weeks (LOCF) was 7.9%, 7.2%, 8.6%, and 11.6%, respectively (Figure 1B).
Short-term studies: analyses of individual metabolic parameters
In the pooled short-term studies, the proportion of patients with individual metabolic parameters that were abnormal at baseline (based on NCEP ATP III criteria; all treatment groups combined) was 28.7% for waist circumference, 29.6% for triglycerides, 38.9% for HDL, 28.0% for blood pressure, and 26.3% for glucose (Table 2). Mean increase in weight and waist circumference and median increase in triglyceride and glucose levels from baseline to 6-week endpoint were greater in patients treated with olanzapine or quetiapine XR compared with patients who received placebo (Table 2). The largest increases at 6 weeks were associated with olanzapine treatment, most notably in weight (+4.2 kg), waist circumference (+3.4 cm), and triglycerides (+25.5 mg/dL). Changes in metabolic parameters at week 6 (LOCF endpoint) on lurasidone were similar to placebo, with the exception of a modest mean increase in waist circumference (+0.9 cm vs +0.3 cm).
Short-term studies: benefit–risk for treatment response
Two placebo-controlled, short-term trials included an active comparator. In the first trial (NCT00615433) that included olanzapine as an active comparator, the NNH for weight gain (≥ 7%) was 100 for lurasidone and 4 for olanzapine. The NNT for treatment response was 9 for lurasidone and 4 for olanzapine. The resulting likelihood of being helped or harmed (LHH) for lurasidone was 11.1 vs 1 for olanzapine (higher LHH values indicate a more favorable benefit–risk ratio for a medication). In the second trial (NCT00790192) which included quetiapine XR as an active comparator, the NNH for weight gain was 56 for lurasidone and 8 for quetiapine XR. The NNT for treatment response was 4 for lurasidone and 3 for quetiapine XR. The resulting benefit–risk LHH for lurasidone was 14 compared to 2.7 for quetiapine XR.
Individual analyses of long-term studies: metabolic syndrome
The safety population of Study D1050237 included 621 patients (Table 2), of whom 147 lurasidone-treated and 90 risperidone-treated patients had metabolic syndrome data at baseline and at month 12. The safety population of study D1050234 included 292 patients (Table 2), of whom 102 lurasidone-treated and 85 quetiapine XR–treated patients had metabolic syndrome data at the initial study baseline and at month 12 of the relapse prevention study.
In Study D1050237, the percentage of patients who met NCEP ATP III criteria for metabolic syndrome at baseline and month 12, respectively, was 30.1% and 26.8% in the lurasidone group and 28.6% and 41.3% in the risperidone group (Figure 2A; left panel). The odds of metabolic syndrome after 12 months of treatment was significantly higher for risperidone compared with lurasidone (OR = 2.12; 95% CI, 1.15-3.90; P = .016). In patients who did not meet criteria for metabolic syndrome at baseline, the proportion who met criteria for metabolic syndrome after 12 months of treatment was significantly lower for lurasidone vs risperidone (11.6% vs 20.0% [OC]; P < .05; Figure 2B; left panel).

Figure 2. Metabolic syndrome status: long-term studies. (A) Proportion of patients meeting metabolic syndrome criteria at baseline and month 12 in two long-term studies (observed cases). (B) Proportion of patients without metabolic syndrome at baseline who met criteria for metabolic syndrome at month 12 in two long-term studies (observed cases).
In Study D1050234, the percentage of patients who met NCEP ATP III criteria for metabolic syndrome at baseline and month 12, respectively, was 16.7% and 10.6% in the lurasidone group and 15.3% and 21.2% in the quetiapine XR group (Figure 2A; right panel). The odds of metabolic syndrome after 12 months of treatment was significantly higher for quetiapine XR compared with lurasidone (OR = 3.92; 95% CI, 1.15-13.40; P = .029). In patients who did not meet criteria for metabolic syndrome at baseline, the proportion who met criteria for metabolic syndrome after 12 months of treatment was significantly lower for lurasidone vs quetiapine XR (3.9% vs 15.2% [OC]; P < .05; Figure 2B; right panel).
Analyses of long-term studies: individual metabolic parameters
In Study D1050237, the proportion of patients with individual metabolic parameters that were abnormal at baseline (based on NCEP ATP III criteria; all treatment groups combined) was 42.9% for waist circumference, 33.7% for triglycerides, 35.1% for HDL, 38.6% for blood pressure, and 30.1% for glucose (Table 2). In Study D1050237, 12 months of treatment with lurasidone was associated with reduction in weight (−1.0 kg), waist circumference (−0.4 cm), and triglycerides (−8.5 mg/dL), whereas treatment with risperidone was associated with increases in weight (+2.6 kg), waist circumference (+2.6 cm), and glucose (+4.0 mg/dL) and a decrease in HDL cholesterol (−4.0 mg/dL; Table 3).
Table 3. Change from Baseline in Weight and Metabolic Parameters.

Abbreviations: HDL, high-density lipoprotein; LOCF, last observation carried forward; LUR, lurasidone; OC, observed cases; OLZ, olanzapine; PBO, placebo; QXR, quetiapine; RIS, risperidone.
a Change from baseline of the preceding 6-week, double-blind study.
b Change from extension study baseline to month 6.
c Mean change is reported for weight, waist circumference, and blood pressure; median change is reported for HDL, triglycerides, and glucose.
d Sample sizes vary based on data availability.
In Study D1050234, the proportion of patients with individual metabolic parameters that were abnormal at baseline (based on NCEP ATP III criteria; all treatment groups combined) was 21.9% for waist circumference, 29.0% for triglycerides, 47.2% for HDL, 22.3% for blood pressure, and 21.1% for glucose (Table 2). In Study D1050234, 12 months of treatment with lurasidone was associated with a small increase in weight (+0.8 kg) and waist circumference (+1.1 cm) and a reduction in triglycerides (−18.0 mg/dL), whereas treatment with quetiapine XR was associated with increased weight (+1.2 kg) and minimal increase in waist circumference (+0.6 cm; Table 3).
Extension studies with medication switch: individual study analyses
In patients with available metabolic data who completed 6 weeks of treatment with lurasidone (N = 115) or olanzapine (N = 69) and who entered the 6-month extension study (D1050231-E), the percentage of patients who met NCEP ATP III criteria for metabolic syndrome at open-label (switch) baseline and month 6 (LOCF), respectively, was 25.2% and 22.9% in patients who continued on lurasidone and 29.0% and 21.8% in patients who switched from olanzapine to lurasidone (Figure 3A). Body weight, waist circumference, and triglyceride level increased during 6 weeks of treatment with olanzapine; while reduction in each of these parameters was observed after switching to 6 months of open-label treatment with lurasidone (Table 3).

Figure 3. Metabolic syndrome status at month 6 (LOCF endpoint) in two medication switch studies. (A) Proportion of patients meeting metabolic syndrome criteria before and after 6 weeks of double-blind treatment with lurasidone vs olanzapine and after 6 months of open-label treatment with lurasidone (olanzapine patients were switched to lurasidone). (B) Proportion of patients meeting metabolic syndrome criteria before and after 12 months of double-blind treatment with lurasidone vs risperidone and after 6 months of open-label treatment with lurasidone (risperidone patients were switched to lurasidone). Abbreviations: LOCF, last observation carried forward; LUR, lurasidone; OLZ, olanzapine; RIS, risperidone.
In patients with available metabolic data (87.4% of the safety population) who completed 12 months of treatment with lurasidone (N = 136) or risperidone (N = 87) and who entered the 6-month extension study (D1050237-E), the percentage of patients who met NCEP ATP III criteria for metabolic syndrome at open-label (switch) baseline and month 6 (LOCF), respectively, was 25.7% and 24.6% in patients who continued on lurasidone and 42.5% and 32.9% in patients who switched from risperidone to lurasidone (Figure 3B). Body weight and waist circumference increased during 12 months of treatment with risperidone; while reduction in each of these parameters was observed after switching to 6 months of open-label treatment with lurasidone (Table 3).
Discussion
This pooled analysis of short- and long-term studies from the lurasidone schizophrenia clinical trial database, which included active comparators, demonstrated that the odds of developing metabolic syndrome, based on NCEP ATP III criteria, were low during treatment with lurasidone. In contrast, the odds (vs placebo) of developing metabolic syndrome were significantly higher for olanzapine and quetiapine XR in two short-term trials and for quetiapine XR and risperidone (vs lurasidone) during long-term trials.
The proportion of patients with schizophrenia meeting NCEP ATP III criteria for metabolic syndrome remained unchanged during 6 weeks of treatment with lurasidone and placebo. Notably, no dose effect on the prevalence rate of metabolic syndrome was observed during 6 weeks of treatment with lurasidone, across the dose range of 40 to 160 mg/d. In contrast, the proportion of patients meeting criteria for metabolic syndrome was significantly increased from baseline to week 6 by 15% and 21.4%, respectively, in patients treated with olanzapine or quetiapine XR.
In patients who did not meet NCEP ATP III criteria for metabolic syndrome at pretreatment baseline, the proportion who met criteria after 6 weeks of treatment was similar for lurasidone and placebo (8.4% for both treatment groups). In contrast, the proportion of patients meeting full criteria for metabolic syndrome after 6 weeks of treatment was significantly higher (vs placebo) for olanzapine (18.6%) and quetiapine XR (24.3%).
In the current short-term trials, the proportion of patients meeting NCEP ATP III criteria for metabolic syndrome at baseline (prior to randomization) was approximately 20%. This is lower than the overall prevalence rate of 32.5% reported in a large meta-analysis of patients with a diagnosis of schizophrenia.Reference Mitchell, Vancampfort and Sweers1 Baseline prevalence of abnormal individual metabolic parameters was also lower in the current study vs results reported in the Mitchell et al meta-analysis,Reference Mitchell, Vancampfort and Sweers1 for example, 28.7% vs 49.4% for abnormal waist circumference. The reason for the lower prevalence rate of metabolic syndrome at baseline in the current analyses, and lower baseline rates of abnormal individual metabolic parameters, may be due to use of standard phase III entry criteria that excluded most medical comorbidities.
Results from our analysis of two long-term, double-blind, active-comparator studies in patients with schizophrenia further support the minimal metabolic effect of lurasidone relative to risperidone and quetiapine XR. The odds of having metabolic syndrome after 12 months of treatment were significantly greater for patients treated with risperidone or quetiapine XR compared to patients treated with lurasidone.
Prospective results from two open-label extension studies thatincluded a medication switch also suggest that worsening metabolic parameters during initial treatment with olanzapine (6 weeks) or risperidone (12 months) can partially be reversed by switching patients to lurasidone (for 6 months). Prevalence rates for metabolic syndrome decreased by 7.2% in patients who switched from olanzapine to lurasidone and by 9.6% in patients who switched from risperidone to lurasidone. Similar improvement in metabolic parameters, and/or rates of metabolic syndrome, have also been reported after switch to aripiprazole and ziprasidone.41–44
The increase in rate of metabolic syndrome observed after short-term treatment with olanzapine and quetiapine XR, and after long-term treatment with risperidone and quetiapine XR in the lurasidone schizophrenia database, is consistent with the known propensity of these agents to produce weight gain and metabolic disturbance.Reference Newcomer15, 45–47
The low risk of metabolic syndrome observed here for lurasidone may be related to its receptor-binding profile which exhibits no clinically relevant affinity for receptors such as histamine H1 (Ki, > 1000) and 5-HT2C (Ki, 415)Reference Ishibashi, Horisawa and Tokuda26 that are known to be associated with weight gain.Reference Reynolds and Kirk24, Reference Kroeze, Hufeisen and Popadak25 In a preclinical study, lurasidone has also been shown to have no effect on insulin resistance.Reference Wu, Yuen and Boyda48 In contrast, atypical antipsychotics associated with higher risk of weight gain and metabolic syndrome (eg, olanzapine, quetiapine, and risperidone) have notably higher affinity for histamine H1 and 5-HT2C receptors and have been shown to be associated with glucose intolerance and increased insulin resistance.Reference Reynolds and Kirk24, 48–50 Preliminary preclinical data in rodents also suggest that lurasidone, when coadministered with olanzapine, may suppress food intake and weight gain associated with olanzapine.Reference Reynolds, Dalton and Watrimez51
The diagnosis of schizophrenia is associated with significantly increased cardiovascular morbidity, excess mortality, and an approximately 20-year shorter life span when compared to nonschizophrenia cohorts.Reference Laursen, Nordentoft and Mortensen52 Metabolic syndrome significantly contributes to this excess morbidity and mortality risk.Reference Laursen, Nordentoft and Mortensen52 The results of this pooled analysis provide further support for treatment guideline recommendations that clinicians should routinely monitor body weight and metabolic parameters throughout the course of treatment with antipsychotic agents.
Early behavioral interventions (eg, exercise, change in diet) are typically recommended if clinically significant weight gain or metabolic abnormalities develop during treatment with atypical antipsychotics.Reference Burghardt, Seyoum and Mallisho50 However, the ability of such interventions to yield sustained improvement in weight or metabolic parameters in the face of continued antipsychotic therapy has not been established.Reference Cooper, Reynolds and Barnes53 Based on current data, it appears that switching to a metabolically safe medication provides greater improvement than exercise or diet.Reference Cooper, Reynolds and Barnes53
The current analyses were not designed to provide a systematic benefit–risk comparison of lurasidone to other antipsychotics and were limited to the active comparator medications included in the available trials. However, LHH is a widely used benefit–risk parameter that allowed us to obtain a preliminary composite index of efficacy relative to metabolic safety for lurasidone, olanzapine, and quetiapine XR during short-term treatment. We utilized weight gain as the safety parameter since it is highly correlated with adverse metabolic effects and is frequently used as a proxy for metabolic outcomes.Reference Rummel-Kluge, Komossa and Schwarz47 Consistent with results from a previous meta-analysis,Reference Huhn, Nikolakopoulou and Schneider-Thoma54 olanzapine had a notably higher short-term response rate compared to lurasidone and quetiapine XR. However, the markedly higher rate of weight gain associated with olanzapine treatment, even during a 6-week trial, resulted in an unfavorable benefit–risk profile for this medication. Patients treated with olanzapine were equally likely to benefit from treatment as they were to be harmed by significant weight gain (LHH = 1), whereas, lurasidone-treated patients were 11 times more likely to benefit from treatment than be harmed by significant weight gain (LHH = 11.1). In the second short-term study, lurasidone-treated patients were 14 times more likely to benefit than be harmed (LHH = 14), while patients receiving quetiapine XR were over twice as likely to experience benefit than harm (LHH = 2.7).
Limitations of the current analysis include, first, the possible bias introduced by study attrition, particularly during long-term treatment studies, resulting in reduced exposure that might lead to an underestimation of the effect of treatment on weight and metabolic parameters. Second, sample sizes were smaller in the active comparator groups thus making estimates of metabolic effects less robust for these medications. Third, it is possible that some patients in the current trials were nonfasting which also may have introduced bias in our estimates of medication treatment effects. Fourth, the current results are limited to studies in the lurasidone schizophrenia clinical trials database for which data comprising of all five individual NCEP ATP III criteria were available. And finally, it should be noted that the comparator antipsychotics in the current analyses (olanzapine, risperidone, quetiapine) have previously demonstrated clinically significant adverse weight and metabolic effects; therefore, the current results for lurasidone may not be generalizable to other typical and atypical antipsychotic drugs (eg, haloperidol and aripiprazole) that have been shown to have minimal adverse weight and metabolic effects. It should be noted, however, that the results of a meta-analysis of >18 000 patients with schizophrenia treated with antipsychotics in controlled trialsReference Laursen, Nordentoft and Mortensen52 found lurasidone to have a low relative risk (vs placebo, RR = 1.23) for clinically significant weight gain (≥7%) compared to the relative risk associated with aripiprazole (RR = 1.86) and haloperidol (RR = 2.02). Consistent with the current results, the relative risk for clinically significant weight gain was markedly higher for risperidone (RR = 3.64), quetiapine (RR = 4.50), and olanzapine (RR = 5.61).Reference Huhn, Nikolakopoulou and Schneider-Thoma54
Conclusions
The results of this analysis of short-term and long-term trials from the lurasidone clinical trials database found that treatment with lurasidone, in the dose range of 40 to 160 mg/d, was associated with a low risk for the development of metabolic syndrome in patients with schizophrenia. These findings contrast with the incidence of metabolic syndrome observed in patients receiving short- and long-term treatment with olanzapine, quetiapine XR, and risperidone.
Given that patients with schizophrenia are at significantly increased risk for cardiovascular disease, type II diabetes, and early death, the favorable metabolic profile of lurasidone, taken together with its demonstrated efficacy in short- and long-term trials,27–34 makes it an important treatment option for patients with schizophrenia.
Acknowledgments
The authors wish to thank the study participants and study investigators. Nancy Holland, PhD of Synchrony Medical Communications, LLC and Edward Schweizer of Paladin Consulting Group provided medical writing and editorial assistance for this manuscript that was funded by Sunovion Pharmaceuticals Inc., Marlborough, MA.
Financial Support
This work was supported by funding from Sunovion Pharmaceuticals Inc.
Disclosures
M.T., A.P., Y.M., and A.L. are employees of Sunovion Pharmaceuticals Inc. J.W.N. has received grant support from the National Institutes of Health and the Substance Abuse and Mental Health Services Administration; has served as a consultant to Indivior, Sunovion, Intra-Cellular Therapies, Otsuka, and Alkermes; has been involved in patent litigation on behalf of Sunovion; and serves on a Data Safety Monitoring Board for Amgen.
Authorship Contributions
All authors meet ICMJE contribution criteria. M.T., J.W.N., A.P., Y.M., and A.L. all contributed to the analysis plan for this paper, the interpretation of the analysis results, and participated actively in the revisions of all drafts of the manuscript.








