Dear Editor,
Thus far, there are eight long-action injectable (LAIs) forms of atypical antipsychotics on the market (Table 1)—a truly very welcomed addition to the psychopharmacological armamentarium. With easiness of use on clinical grounds, three major advents have taken place with recent agents, namely, no more need for the initial oral coverage, less frequent injections (might be dosed up to q12 weeks), and, above all, almost devoid of the stigmatizing neuro-hormonal side effects that plagued the older “depot” forms.
Clinical practice has witnessed a shift from using LAIs for chronic stabilized cases into first-episode psychosis (FEP) patients especially with data accruing speaking to the idea of improving the clinical and functional outcomes when used sooner than later.Reference Stahl 1 For instance, a randomized controlled trial (RCT) has shown a sevenfold decrease in relapses for those starting LAIs for FEP. This ensures almost 100% adherence. This is really a desideratum. The European First Episode Schizophrenia Trial (EUFEST) study, for instance, has shown that 42% of patients have stopped their meds within the first year. Apart from relapse prevention, it subserves a survival advantage since schizophrenia has been tied to premature mortality (shortened telomere, suicide, metabolic burden, etc.). Moreover, each relapse portends a poor pharmacological response for subsequent episodes (correlates with neuroprogression). LAIs can in theorem modify these trajectories.
Having said that, few points germane to the use of LAIs in practice are noteworthy mentioning.Reference Rieford 2
Emphasizing nonadherence as the only indication for LAIs is misleading. Atypical antipsychotics can allegedly confer some neuroprotection (eg, promoting neurogenesis in the subventricular zone, anti-inflammatory actions, increasing the BDNF, etc.) Less variation in peak-and-trough levels would portend a better side effects profile compared to the corresponding oral counterparts. Moreover, some data, albeit inconsistent, also has showed superior efficacy for more resistant cases.
Although LAIs are generally globally underutilized, sole reliance on LAIs to enhance treatment-adherence might prove counter-intuitive. This is twofolded. First, it belittles a host of strategies that can help improving adherence, like developing a therapeutic alliance with patients, psychoeducation, family engagement, therapeutic drug monitoring, using evidence-based high-quality psychotherapy, negotiating undisclosed side effects (weight gain, sexual dysfunction), and so forth. Second, it might be regarded by patients as a sort of coercive treatment (passive compliance).
This can further be obfuscated, where a study found no difference in relapse rates over 30 months in patients receiving either LAI risperidone or oral atypical antipsychotics!
Another concern to be factored in is the economic impact, especially many of these newer agents are still brands and pretty expensive. Of related interest, one study found no difference in relapse rates over 2.5 years among patients receiving paliperidone palmitate or haloperidol decanoate!
Moreover, prescribing LAIs early on in FEP might have negative connotations to some patients as erroneously implying severity of condition. Also, there remain some loose ends to be tied up regarding the diagnostic stability for FEP. Similarly, there is dearth of data regarding LAIs in child/adolescent psychiatry (CAP) population being currently underresearched. We could locate a review by Lytle et alReference Lytle, McVoy and Sajatovic 3 of seven reports. These included three case reports, three case series and one open-label trial, a totality of 36 patients with circa 80% being male with mean age of the trial 12.1 ± 2.2 years and half had bipolar I diagnosis with 2/3 on risperidone LAI. This review suggested that LAI use in youth with serious mental illness may improve clinical outcomes and adherence. Side effects of LAIs among youth appeared similar to oral preparations. A recent observational studyReference Fortea, Ilzarbe and Espinosa 4 with retrospective analysis of medical records showed 2.6% were prescribed second generation (SG)-LAIs; females (53%) slightly outnumbered males, mean age of 16.3 years, main diagnoses were psychosis (70%) and disruptive behavior disorders (DBDs; 30%), and primary reasons were poor compliance (90%) and/or poor insight. SG-LAIs used were aripiprazole (40%), risperidone (36%), and paliperidone palmitate. The authors concluded that SG-LAIAs may be a safe treatment option during adolescence in inpatients with psychotic disorders, as well as with DBDs. No differences were found in clinical global impression-improvement (CGI-I) improvement scores between the three SG-LAIs used, although patients on risperidone reported more side effects than those on aripiprazole.
Last but not least, considering some unforeseen (tardy) side effects, when using LAIs, it can be difficult to eliminate it by just withdrawing the medication due to prolonged half-lives and different pharmacokinetics. Additional side effects related to the parenteral route of administration (eg, local pain, skin irritation, etc.) might be encountered.Reference Kane 5
It behoves prescribers then to be mindful and vigilant manipulating merits and demerits of LAIs in clinical practice on the way to define its real place in the niche of psychopharmacotherapy.
Disclosures
The authors declare no conflict of interests in the past 36 months. No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Table 1. LAIs of atypical antipsychotic (AAPs) Currently on Market
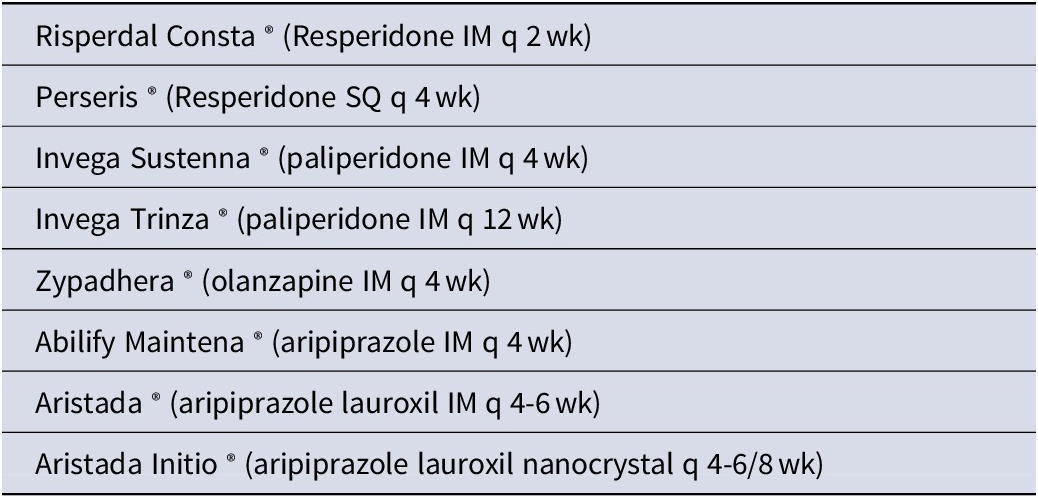
Abbreviations: LAI, long-action injectable forms.



