Fetuses with critical aortic stenosis with severe mitral regurgitation and left atrial enlargement are at risk to develop heart failure, hydrops and intrauterine death or, if liveborn, have to undergo immediate postnatal cardiac interventions or surgeries with a poor prognosis. Reference Tulzer, Arzt and Tulzer1–Reference Mallmann, Herberg and Gottschalk7 Fetal cardiac interventions have been introduced to alter the natural history of these patients in order to improve fetal hemodynamics, fetal survival and ultimately the chances for a biventricular outcome after birth. Usually sometimes complex procedures are required postnatally ranging from aortic balloon valvuloplasty to open heart surgery with repair or replacement of the aortic valve, or a univentricular palliation for hypoplastic left heart syndrome might be necessary.
In this case report we present two fetuses with this physiology who underwent fetal aortic valvuloplasty at our center as their only intervention without a need for any postnatal procedures during short- to medium-term follow-up.
Case series
Both patients were part of a previously published report. Reference Tulzer, Arzt and Gitter5 Two pregnant women with critical aortic stenosis, severe mitral regurgitation and left atrial enlargement of their fetuses (gestational ages 25 + 5 and 28 + 2 weeks, respectively) were admitted to our center for fetal aortic valvuloplasty. Fetus 1 had signs of congestive heart failure with hydrops, fetus 2 did not show signs of hydrops. Table 1 shows the pre-procedural and follow-up fetal echocardiographic findings until birth of the two patients. Figure 1 and supplementary video 1 show the four chamber views from baseline to birth of fetus 1. The procedures were performed as described previously. Reference Tulzer, Arzt and Tulzer1,Reference Wohlmuth, Tulzer, Arzt, Gitter and Wertaschnigg8,Reference Tulzer, Arzt, Franklin, Loughna, Mair and Gardiner9 Both cases had fetal echocardiograms on the day after the procedure showing morphologic and hemodynamic changes: the aortic valve (4.5 mm) of fetus 1 was dilated with a 4 mm balloon catheter up to 16 atm (4.5 mm). The day after the procedure fetus 1 had new antegrade flow in the aortic arch with only little aortic valve regurgitation, shortening of the left ventricle improved, and the left ventricular inflow duration increased. Preprocedural hydrops resolved within two days after the intervention.
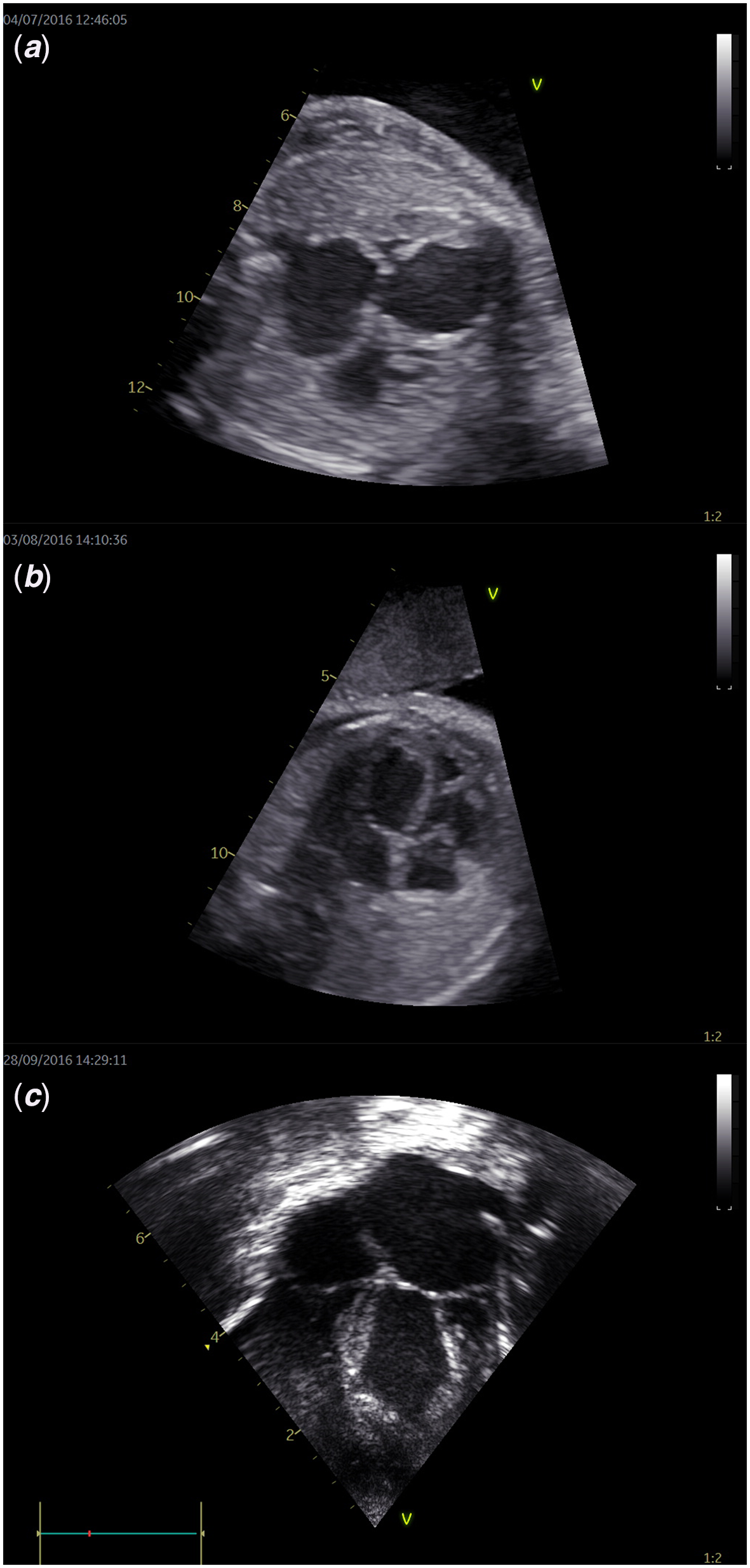
Figure 1. Four-chamber views of fetus 1: from baseline to birth. ( a ) The four-chamber view of fetus 1 before fetal aortic valvuloplasty shows a severely dilated left ventricle and atrium compressing the right-sided cardiac structures. ( b ) Four weeks after FAV, the left ventricle appears shorter with less dilatation, also the size of the left atrium is normalized; the right ventricle shows improved size due to better filling after decompression of the left ventricle. ( c ) Directly after birth, the left ventricle still shows mild to moderate dilatation, but is of good function; the left atrium is also enlarged with the ductus arteriosus still open.
Table 1. Echocardiographic data before FAV until birth in two fetuses with CAS and severe mitral regurgitation.
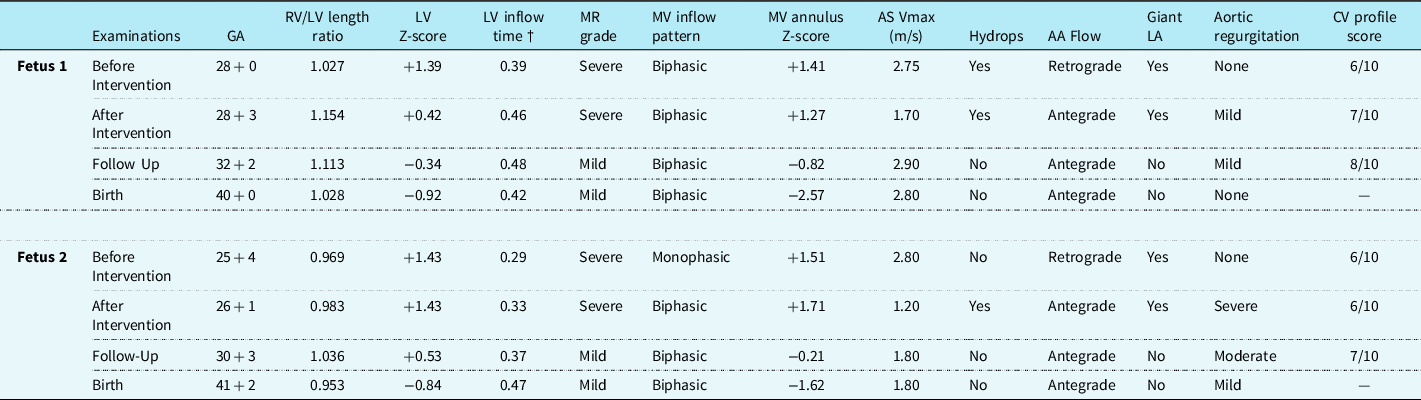
AA, aortic arch; AS, aortic stenosis; GA, gestational age; LA, left atrium; LV, left ventricle; MR, mitral regurgitation; RV/LV length ratio, right-to-left ventricular length ratio.
†Duration of mitral valve (MV) inflow indexed to cardiac cycle length.
Four weeks after the fetal intervention, mitral valve regurgitation decreased from severe to mild and the left ventricle showed further remodeling with decreased size estimated by a change in right ventricle/left ventricle ratio. There was no longer evidence of aortic valve regurgitation and the gradient across the aortic valve increased from 1.70 m/sec after the intervention to 2.90 m/sec at follow-up.
The aortic valve of fetus 2 (4.3 mm) was dilated with a 4 mm balloon catheter up to 18 atm (4.6 mm). Fetus 2 developed ascites the day after the procedure, which resolved within one week. There was also new antegrade flow in the aortic arch, but there was also severe aortic valve regurgitation. There was no relevant change in left ventricular size or left ventricular inflow on the day after the intervention. At follow-up, four weeks after the intervention, the severity of mitral valve regurgitation decreased from severe to mild with a changed inflow pattern from fused to biphasic. There was no longer evidence of ascites. Similarly to fetus 1, the gradient across the aortic valve increased somewhat from 1.20 m/sec to 1.80 m/sec and the severity of aortic valve regurgitation decreased from severe to moderate.
In both patients further echocardiographic improvements up to an almost normalization of left ventricular function could be found during the rest of pregnancy.
Both fetuses were born at term (40 + 0 and 41 + 2 weeks) at our institution. Residual gradients, estimated by echo, of 31 mmHg and 13 mmHg across the aortic valve could be found in both patients. There was no aortic regurgitation left in patient 1 and only mild aortic regurgitation in patient 2. Both patients did not show any significant abnormalities with regards to mitral valve morphology. Prostaglandine E2 infusions could be stopped without the need of postnatal interventional or surgical procedures and the patients could be discharged in the neonatal period. Both patients are still free of any procedures and medication and do not show any signs of post-capillary pulmonary hypertension at follow-ups at 1.4 and 4.9 years, respectively.
Discussion
We report 2 cases of fetuses with critical aortic stenosis and congestive heart failure in whom a fetal aortic valvuloplasty was a definite successful treatment during short- and medium-term follow-up.
The beneficial course of these two patients stands in contrast to the reported outcomes of other patients with this physiology with a mortality of up to 80%. Reference Tulzer, Arzt and Tulzer1,Reference Vogel, McElhinney and Wilkins-Haug6,Reference Mallmann, Herberg and Gottschalk7
A possible explanation for this excellent course after fetal aortic valvuloplasty was that the anatomy of the aortic valves, which usually are very dysplastic, allowed a very good result with no relevant residual gradient. Postinterventional aortic valve regurgitation was present in both patients indicating a successful and effective dilatation. However, fetus 2 had severe aortic regurgitation and ascites after the intervention. The left ventricular length increased compared to the pre-interventional echocardiography. A possible explanation for the development of ascites could be that the already severely pressure and volume loaded left ventricle with poor function was additionally stressed by the severe aortic regurgitation which led to a deterioration of cardiac output in the first hours after fetal intervention.
In the two fetuses presented here, aortic regurgitation improved or even resolved until birth due to valvular remodeling. In our longitudinal observations after the interventions, we were able to observe improved left ventricular-shortening, improved left ventricular filling and a decrease of left atrial size. Another finding was that the severity of mitral regurgitation obviously improved until birth. This stands in contrast to a previous report, which claimed that a primary abnormal mitral valve may be a key anomaly in fetuses with this kind of physiology leading to severe left atrial enlargement and even hydrops. Reference Vogel, McElhinney and Wilkins-Haug6 Thus, severe mitral regurgitation could be seen as a secondary phenomenon in these patients.
Conclusion
In some fetuses with critical aortic stenosis, mitral regurgitation and severe left atrial enlargement with or without hydrops fetal aortic valvuloplasty has the potential to restore cardiac function and fetal hemodynamics up to a point where no postnatal treatment is required in the first years of life.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951122002566
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees (study number 1009/2017; Ethikkommission des Landes Oberösterreich, Austria).





