Paediatric heart failure carries significant morbidity and mortality, and is prevalent in all regions of the world. While the global burden is largely unknown, recent analyses have shown that it results in up to 14,000 hospitalisations annually in the United States. Reference Rossano, Kim and Decker1–Reference Das3 Acute decompensated heart failure accounted for 6% of > 26,000 admissions to paediatric cardiac intensive care units (ICU) in the Pediatric Cardiac Critical Care Colloquium (PC4) Registry between 2014 and 2017, with 59% of these patients requiring mechanical ventilation and with an ICU mortality rate of 16%. Reference Lasa Javier, Michael and Bush4 Patients with acute decompensated heart failure will frequently need to undergo endotracheal intubation, either as part of resuscitation or prior to a procedure.
We have previously shown that the incidence of cardiac arrest during endotracheal intubation in critically ill paediatric cardiac patients is higher than in non-cardiac patients and is even higher in the presence of systolic ventricular dysfunction. Reference Esangbedo, Byrnes, Brandewie, Ebraheem, Yu, Zhang and Raymond5 Physiologically, this increased risk of cardiac arrest is explained by a possible combination of some of the following: sedative drugs causing myocardial depression, vasodilation or bradycardia; increased intrathoracic pressure with resultant decreased venous return and cardiac output; development of worsened respiratory acidosis intra-procedure; increased metabolic demands from procedural stimulation leading to myocardial stress; and hypoxaemia secondary to airway collapse, aspiration of gastric contents, misplaced endotracheal tube, or inability to place endotracheal tube in a timely fashion.
While there is vast clinical experience supporting an increased incidence of haemodynamic complications such as cardiac arrest during intubation of patients with systolic dysfunction, the description of this phenomenon in the paediatric critical care literature is surprisingly sparse. Data from paediatric anaesthesia studies have shown that there is a risk of haemodynamic complications in children with severe heart failure or cardiomyopathy undergoing general anaesthesia for non-cardiac surgeries, Reference Kipps, Ramamoorthy and Rosenthal6,Reference Murphy, Smith and Ranger7 though these studies have primarily evaluated anaesthetic complications, without a focus on the peri-intubation period. In this publication, we aimed to determine the rate of and risk factors for peri-intubation cardiac arrest in children with significant systolic ventricular dysfunction admitted to intensive care and to describe clinician practices during intubation in this population.
Methods
This was a multicenter retrospective cohort study. We reviewed endotracheal intubations performed in stand-alone paediatric cardiac ICUs at four institutions in the United States between January 2015 and December 2017 (3 years). The rate of peri-intubation cardiac arrest was measured in patients with significant systolic dysfunction, and we compared the intubation events that resulted in cardiac arrest in this population with events that did not. We also reviewed clinician practices during intubation of patients with significant systolic dysfunction and compared them to practices performed during the intubation of other paediatric cardiac ICU patients from the same time period who did not have significant systolic dysfunction.
Multiple intubations in the same patient were included if they were recorded in medical records as separate events. Data collected included patient demographics, cardiac history, cardiac surgeries, co-morbidities, clinician characteristics, event characteristics and outcomes. Institutional review board approval was secured at each study site. Consent was waived per United States Code of Federal Regulations 45 CFR 46.116(f)(3). Data use agreements were obtained between the primary institution (University of Texas Southwestern Medical Center, Dallas, Texas) and each of the other institutions. Compliance with the Health Insurance Portability and Accountability Act was maintained.
Inclusion criteria
We included critically ill children (0–18 years) with congenital or acquired heart disease who were hospitalised in a cardiac ICU and required endotracheal intubation for any indication.
Exclusion criteria
We excluded the following categories of patients:
-
1. Patients who were intubated outside the cardiac ICU.
-
2. Patients who suffered cardiac arrest prior to attempt at tracheal intubation.
-
3. Patients requiring endotracheal tube exchange.
-
4. Patients already on extracorporeal membrane oxygenation during intubation procedure.
-
5. Patients who were intubated by an anaesthesiologist for a scheduled elective procedure or surgery (even if done within cardiac ICU).
-
6. Patients with incomplete medical records.
Definitions
Peri-intubation cardiac arrest was defined as any form of cardiac arrest requiring chest compressions ≥ 1 minute, which occurred during or within 30 minutes of endotracheal intubation.
Significant systolic dysfunction of the systemic ventricle was defined as “moderate” or “severe” systolic dysfunction of the systemic ventricle, as determined and described subjectively by a paediatric cardiologist on the most recent echocardiography report.
Statistical analysis
Descriptive analyses (means, standard deviations, medians, interquartile range (IOQ) for continuous variables and counts and percentages for categorical variables) were used to describe patient demographics, clinical characteristics, and outcomes overall and stratified by group. Chi-square or Fisher exact tests as appropriate were used to compare categorical covariates groups, and Mann–Whitney U-test and Student’s t-test were used to compare continuous variables as appropriate. Multivariable regression analyses were not reported because of small sample size for one group. All hypothesis tests were two-tailed. A P value of < 0.05 indicated statistical significance. All analyses were performed in SAS (version 9.4, Cary, NC).
Results
From four paediatric cardiac ICUs, there were 67 intubation events that were performed in cardiac patients with significant (moderate or severe) systolic dysfunction of the systemic ventricle. Figure 1 is a flow diagram showing distribution of subjects by cardiac ICU and summary of findings. There were 183 intubation events in children with normal systolic function or only mild dysfunction from the same time period.
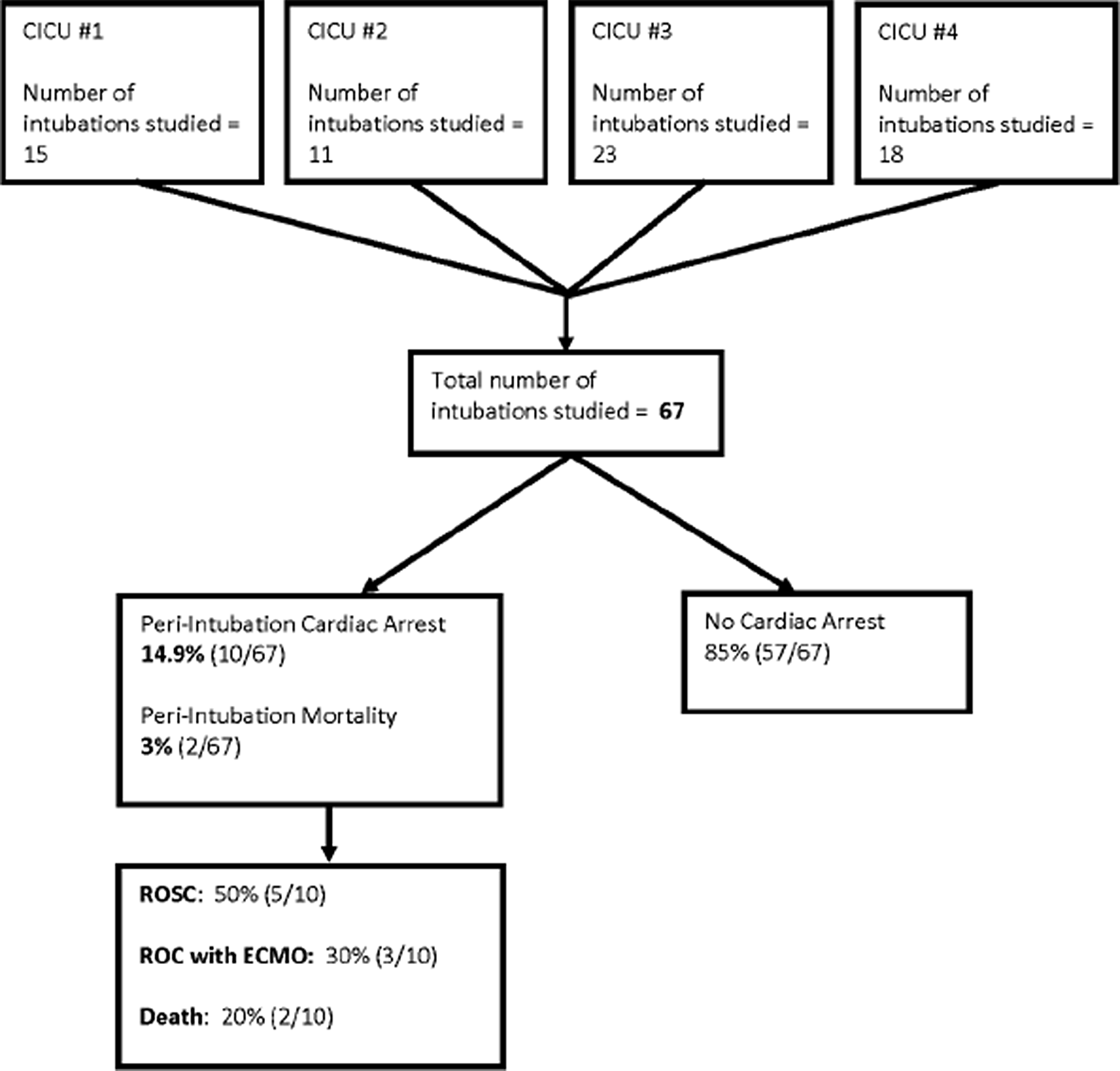
Figure 1. Flowchart showing sources and outcomes of intubation events occurring in patients with significant systolic dysfunction (n = 67). CICU, cardiac ICU. ROSC, return of spontaneous circulation. ROC, return of circulation. ECMO, extracorporeal membrane oxygenation.
Significant systolic dysfunction group
Patient characteristics
Median age was 4 months [IQR 0.7−41], and 29 patients (43.3%) were male. Median weight was 4.6 kilograms (IQR 3.5−13). Of 67 intubation events, 24 (35.8%) occurred in patients with moderately diminished systolic function of their systemic ventricle, as recorded in the most recent echocardiogram; 43 (64.2%) occurred in patients with severely diminished systolic function. Supplementary table S1 summarises patient demographics of the group with significant systolic dysfunction (n = 67).
Ten of 67 (14.9%) were performed in patients with dilated cardiomyopathy, 8 (11.9%) were performed in patients with critical coarctation, 4 (6%) were in patients who were status post-orthotopic heart transplant, 3 (4.5%) were in patients with myocarditis, 2 (3%) were in patients with critical aortic stenosis, and 2 (3%) in patients with anomalous left coronary artery from the pulmonary artery. The remainder of the cohort had other forms of CHD, sepsis, or arrhythmias.
There were 15 intubations (22.4%) in patients who were less than one month after cardiac surgery; of these, 3 (4.5%) were less than three days post-operation. There were 52 intubations (77.6%) in patients who were pre-surgical, non-surgical, or had had cardiac surgery > 1 month prior. There were 20 intubations (29.9%) in pre-Glenn procedure single ventricle patients. Trisomy 21 occurred in 3 (4.5%) patients, and there was one patient (1.5%) with each of the following syndromes – DiGeorge syndrome, Turner’s syndrome, and Williams syndrome.
Of 67 intubations, 23 (37.1%) patients already had oxygen saturations that were more than 10% below expected/baseline prior to the first intubation attempt. Likewise, 23 (37.1%) patients were hypotensive prior to first intubation attempt, with a drop in mean arterial pressure of more than 20% from baseline. Serum lactate was ≥ 5mmol/L in 22 (32.8%) cases. Indications for intubation included (not mutually exclusive) work of breathing (n = 22; 32.8%); shock (n = 21; 31.3%); hypoxaemia (n = 15; 22.4%); hypercarbia/respiratory acidosis (n = 12; 17.9%); metabolic acidosis (n = 12; 17.9%); and heart failure exacerbation (n = 10; 14.9%).
Provider characteristics
The first intubation attempt was performed by intensive care attending physicians in 18 cases (26.8%), anaesthesiology attending physicians in 10 cases (14.9%), intensive care fellows in 26 cases (38.8%), and nurse practitioners in 9 cases (13.4%).
Procedure characteristics
Video laryngoscopy was only used in 4 cases (6%). Majority of cases (51; 76%) required only one laryngoscopy attempt (direct or video laryngoscopy). Atropine was used in 3 cases (4.5%).
Medications used to facilitate intubation included fentanyl in 49 cases (73.1%), ketamine in 24 cases (35.8%), etomidate in 11 cases (16.4%), and midazolam in 8 cases (11.9%). One patient received propofol (1.5%), one received morphine (1.5%), and 3 received dexmedetomidine (4.5%). Supplementary table S2 shows the drug combinations used in each patient.
Cardiac arrest events & risk factors
Of the 67 intubation events in patients with significant systolic dysfunction, there were 10 that resulted in peri-intubation cardiac arrest (rate of 14.9%). By contrast, the peri-intubation cardiac arrest rate among the patients in the cohort with normal function or mild dysfunction was 3.8% (7/183 intubations).
Median cardiopulmonary resuscitation duration for the 10 arrest patients was 14 minutes [IQR 10-45 min]. Majority (6/10; 60%) of the cardiac arrests were classified as pulseless electrical activity. There were 2 deaths of 67 intubations, resulting in a peri-intubation mortality rate of 3% (20% of peri-intubation cardiac arrest cases). Supplementary table S3 summarises the types and outcomes of cardiac arrest in the 10 peri-intubation cardiac arrest cases.
Table 1 shows comparison of variables between the arrest group (n = 10) and non-arrest group (n = 57). Statistically significant differences included serum lactate levels and serum pH; patients who suffered peri-intubation cardiac arrest were more likely to have had serum lactate > 10mmol/L and serum pH < 7.0 compared to patients who did not suffer cardiac arrest with intubation. In addition, pre-intubation hypotension (mean arterial pressure decrease ≥20% from baseline) was twice as common in the peri-intubation cardiac arrest patients (66.7% versus 30.9%), although this difference did not reach statistical significance (p = 0.09). Since hypotension could be a confounder for its association with both lactate acidosis and cardiac arrest, we had aimed to perform multivariable regression analysis to determine the independent effect of the serum lactate and serum pH variables. However, a significant multivariable regression analysis could not be performed due to the small number of patients in the arrest group.
Table 1. Intubation events in paediatric cardiac patients with significant systolic dysfunction (n = 67). Data presented as n(%). Denominators provided if different from rest of column due to missing data

IQR, interquartile range. MAP, mean arterial pressure. NPO, nil per os. CRNA, certified registered nurse anaesthetist.
Between arrest (n = 10) and non-arrest (n = 57) groups, there was no statistically significant difference in type of respiratory support that patients had immediately prior to intubation; 23.9% of all patients had been placed on bilevel positive airway pressure before the decision to intubate. There was also no statistically significant difference in post-operative status or in exposure to different sedative agents used for induction.
Clinician practices: Comparison of events without significant dysfunction
Table 2 shows comparison of provider practices when intubating the patients with significant systolic dysfunction (n = 67) versus when intubating the patients without significant systolic dysfunction (n = 183).
Table 2. Provider practices: Comparison of intubation events in cardiac ICU patients with moderate-severe dysfunction (n = 67) versus patients with normal function or mild dysfunction (n = 183). Data represented as n (%)
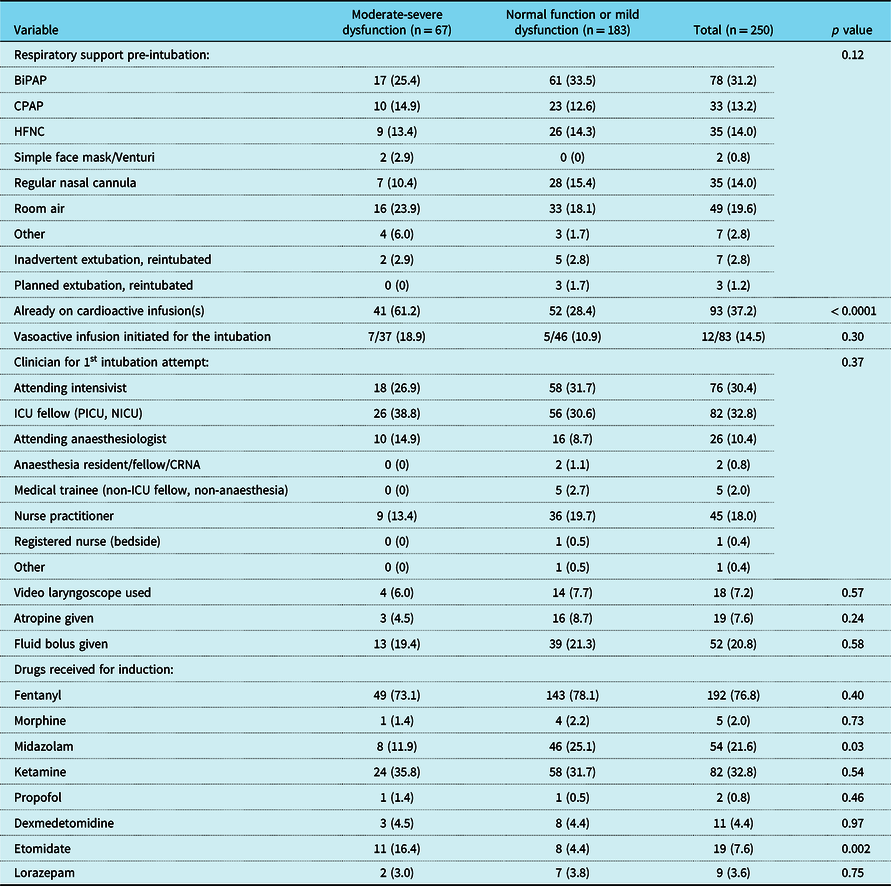
BiPAP, bilevel positive airway pressure. CPAP, continuous positive airway pressure. HFNC, high flow nasal cannula. CRNA, certified registered nurse anaesthetist.
There was a lower rate of use of midazolam for induction in the group with significant systolic dysfunction (11.9% versus 25.1%; p = 0.03). The use of etomidate in this group was significantly higher (16.4% versus 4.4%; p = 0.002). There was no other difference in use of sedative induction drugs. Fentanyl was the most common sedative-analgesic agent used in all patients (76.8%; 192/250), regardless of ventricular function.
Patients with significant systolic dysfunction were more likely to already be on a cardioactive infusion prior to intubation (usually milrinone) (61.2% versus 28.4%; p < 0.0001). However, there was no significant difference between the two groups in the proportion of patients who were started on an inotrope specifically for the intubation procedure.
There were also no significant differences in clinician who performed first intubation attempt, administration of a fluid bolus, administration of atropine, or use of video laryngoscopy.
Discussion
In the cohort of critically ill paediatric cardiac patients with significant (moderate or severe) systolic dysfunction, the peri-intubation cardiac arrest rate was 14.9% and peri-intubation mortality rate was 3%. In our previous study including only 3 institutions, we found a peri-intubation cardiac arrest rate of 7% in critically ill paediatric cardiac patients admitted to high-acuity stand-alone cardiac ICUs, and the subgroup with significant systolic dysfunction had a peri-intubation cardiac arrest rate of 20.7%. Reference Esangbedo, Byrnes, Brandewie, Ebraheem, Yu, Zhang and Raymond5 Prior studies from the National Emergency Airway Registry for Children (NEAR4Kids) had revealed a peri-intubation cardiac arrest rate between 1.28-1.7% in critically ill children, with a slightly higher peri-intubation cardiac arrest rate (2.8%) in patients with a cardiac diagnosis. Reference Shiima, Berg and Bogner8,Reference Gradidge, Bakar and Tellez9 The NEAR4Kids population was mostly (but not entirely) admitted to general paediatric ICUs, and details about the acuity of cardiac diagnoses and surgical status were not known. This study demonstrates and confirms a much higher peri-intubation cardiac arrest rate in the presence of significant systolic dysfunction in critically ill children.
The overall rate of cardiac arrest associated with elective general anaesthesia in children is very low (<0.05%). Reference Hansen, Børke and Isohanni10,Reference Engelhardt, Ayansina and Bell11 Very few studies have evaluated the rate of haemodynamic complications in paediatric heart failure patients undergoing general anaesthesia. Murphy et al showed that a small cohort of children with heart failure undergoing elective general anaesthesia had a cardiac arrest rate of 10%, although these arrest events were not reported to be in the peri-intubation period. Reference Murphy, Smith and Ranger7
There are pathophysiologic considerations during endotracheal intubation in patients with systolic dysfunction. Drugs with myocardial depressant effects may lead to cardiovascular collapse. A transition to positive intrathoracic pressure with decreased venous return may not be tolerated. Metabolic or respiratory acidosis and hypoxaemia may also be poorly tolerated. Our study found a higher occurrence of serum lactate elevation and pre-intubation acidosis in the patients with systolic dysfunction who suffered cardiac arrest compared to those who did not arrest.
In comparing the patients with significant systolic dysfunction (n = 67) to patients from the same time period with normal function or only mild dysfunction (n = 183), we found that clinicians were less likely to use midazolam and more likely to use etomidate for intubation. There were no other statistically significant differences in clinician practices. Use of other sedative agents, video laryngoscopy (versus direct laryngoscopy), atropine, and inotrope initiation did not differ between the groups. The consultation of an anaesthesiologist to assist with intubation in the ICU also was not different between the groups.
Drugs with direct myocardial depressant effects were avoided. Propofol has a known negative inotropic effect Reference Gelissen, Epema and Henning12,Reference Bovill13 and was used in only one patient with significant systolic dysfunction. Ketamine has a direct negative inotropic effect, but this may be masked by its central sympathetic stimulation as well as inhibition of neuronal catecholamine uptake, in cases where there is no depletion of catecholamines. Reference Gelissen, Epema and Henning12 Ketamine was used in 35.8% (24/67) of patients in this cohort with significant systolic dysfunction. Etomidate has minimal effects on the cardiovascular system and was used in 11/67 patients (16.4%). Fentanyl, which may cause a relative bradycardia in patients who are critically dependent on a high heart rate, Reference Lucas, Nasr, Ng, Joe, Bond and DiNardo14 was the most common agent that patients in this cohort were exposed to [73.1% (49/67) of patients with significant systolic dysfunction; 76.8% (192/250) of all patients regardless of ventricular function].
In general, risk factors for peri-intubation cardiac arrest may be modifiable or non-modifiable. In critically ill children with systolic dysfunction, clinicians should be prepared for cardiopulmonary resuscitation which may include notifying teams for extracorporeal cardiopulmonary resuscitation where available. Modification of risk may include determining ways to optimise haemodynamics before intubation. Lactic acidosis, which was associated with peri-intubation cardiac arrest in our cohort, may be considered non-modifiable if a patient presents late. However, in patients that present the opportunity, then early intubation before the development of metabolic acidosis may help.
Pre-intubation checklists may be used to aid in accounting for risk factors for peri-intubation cardiac arrest. Although the published data are conflicting as to their overall effectiveness (15–24), several studies have demonstrated a benefit in the utilisation of pre-intubation checklists. In a systematic review and meta-analysis that included studies of endotracheal intubation in various hospital settings, Turner et al showed that implementation of a pre-intubation checklist did not improve peri-intubation mortality, but did reduce the incidence of hypoxaemia with intubation. Reference Turner, Bucca and Propst24 We previously have demonstrated that hypoxaemia during the intubation procedure was associated with peri-intubation cardiac arrest in the paediatric cardiac ICU. Reference Esangbedo, Byrnes, Brandewie, Ebraheem, Yu, Zhang and Raymond5
Limitations
Our study has limitations. Our sample size is relatively small. Echocardiography reports of severity of systemic ventricular systolic dysfunction carry subjectivity. We did not use slightly more objective measurements such as ejection fraction, because oftentimes the systemic ventricles being assessed were right ventricles. This study also made the assumption that the most recent echocardiogram performed reflected the state of each patient’s heart at the time of intubation. We did not collect data on duration of time period between the most recent echocardiogram and endotracheal intubation.
Conclusion
The association between haemodynamic adverse events and endotracheal intubation in patients of all ages with cardiac disease is well-established. This is the first study to describe the rate of and risk factors for peri-intubation cardiac arrest in critically ill paediatric cardiac patients with systolic dysfunction based on echocardiography. Intubation in this specific population of paediatric cardiac ICU patients carried a higher rate of cardiac arrest when compared to previously established peri-intubation cardiac arrest rates in other critically ill children with heart disease. Higher serum lactate levels in this population were associated with higher rates of peri-intubation cardiac arrest. In our cohort, ICU clinicians modified their choices of induction medications when intubating cardiac patients with systolic dysfunction, being significantly more likely to use etomidate and to avoid midazolam.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1047951122001160
Acknowledgements
The authors would like to thank the four institutions that contributed data to this multicenter project: University of Texas Southwestern Medical Center (Children’s Medical Center Dallas), Dallas, Texas; Cincinnati Children’s Hospital and Medical Center, Cincinnati, Ohio; University of Florida (Shand’s Children’s Hospital), Gainesville, Florida; and University of Alabama, Birmingham, Alabama.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.






