Idiopathic intracranial hypertension (IIH) is characterized by elevated intracranial pressure (ICP) in the absence of any intracranial space-occupying lesion or cerebral venous thrombus. Increased ICP can cause significant visual impairment over time. Reference Digre1 Papilledema in IIH is typically bilateral. Reference Digre1 As such, unilateral papilledema is atypical but responds to conventional therapy. Here, we describe three cases of unilateral papilledema in the setting of IIH and review the pathogenesis.
A 33-year-old woman was referred with left optic disc swelling seen on routine optometry examination (Case 1). She endorsed several weeks of transient visual obscurations in the left eye and a 3-year history of peri-orbital headaches and pulsatile tinnitus, worsening in the last several months. She had gained 50 lbs. in the last year and was taking citalopram for anxiety.
Weight was 300 lbs.; BMI 43 kg/m2. Corrected visual acuity was 20/20 OU. Ishihara color plates were 13/13 OD and 12/13 OS. There was no relative afferent pupillary defect (RAPD). The right optic disc was normal. The left disc demonstrated Frisén grade 3 edema and was elevated with circumferential swelling and venous engorgement. Visual fields were normal to confrontation. Extraocular movements were full. 24-2 Humphrey visual field testing was normal in the right eye (mean deviation [MD] + 0.73 dB) and showed an enlarged blind spot in the left (MD −0.08 dB). Optical coherence tomography (OCT) revealed an average retinal nerve fiber layer (RNFL) thickness of 111 µm OD and 245 µm OS. The remainder of her neurologic examination was normal. CT/CT venogram (CTV) head showed no mass or thrombus. Computed tomography (CT) orbits optic canals diameters were 4.4 × 5 mm OD and 5 × 5.1 mm OS (17.3 vs. 20.0 mm2). Lumbar puncture opening pressure was 46 cm H2O. Cerebrospinal fluid (CSF) analysis was normal. She was started on acetazolamide 500 mg twice daily and counseled to lose weight. After 3 months, her headaches and transient visual obscurations had decreased. Visual acuity remained stable. Funduscopy was normal on the right and showed blurring of the nasal disc margins on the left. OCT demonstrated a reduction in RNFL thicknesses (106 µm OD, 113 µm OS). She developed nephrolithiasis, thus acetazolamide was decreased to 250 mg twice daily. She ultimately lost 31 lbs.; BMI 38.6 kg/m2. Left papilledema and enlarged blind spot (MD + 0.56 dB OD, −0.35 dB OS) was resolved after 1 year, and she has remained stable for 6 years.
A 27-year-old woman was referred with several weeks of blurred vision in the right eye with transient visual obscurations (Case 2). She described infrequent retro-orbital pressure headaches and pulsatile tinnitus. She had a history of obesity and had gained 20 lbs. in the preceding year. She otherwise had asthma, treated with salbutamol inhaler as needed, and had a copper intrauterine device in situ.
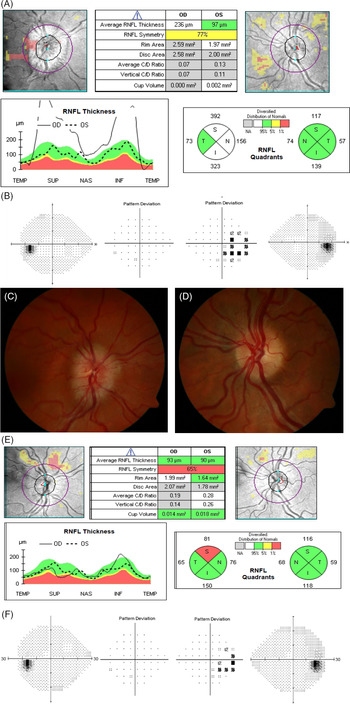
Weight was 192 lbs.; BMI 31 kg/m2. Corrected visual acuity was 20/25 OD and 20/20 −2 OS. Ishihara color plates were 15/17 OD and 17/17 OS. Pupils reacted equally to light without RAPD. Funduscopy revealed Frisén grade 2 optic disc edema in the right eye; the left optic disc appeared normal (Figure 1C and D). Spontaneous venous pulsations were absent bilaterally. Visual fields were full to confrontation. Extraocular movements were full. 24-2 Humphrey visual field testing showed an enlarged blind spot in the right eye (MD + 0.05 dB); the left was normal (MD + 1.73 dB) (Figure 1B). OCT showed an average RNFL thickness of 236 µm OD and 97 µm OS (Figure 1A).

Figure 1: Initial OCT in Case 2 (A) shows an average RNFL thickness of 236 µm OD and 97 µm OS. Initial 24-2 Humphrey visual field testing (B) shows an enlargement of the blind spot in the right eye (MD + 0.05 dB; 4% false-positive errors) with a normal field on the left (MD + 1.73 dB; 0% false-positive errors). Fundus photographs from Case 2 obtained pre-treatment show prominent optic disc edema in the right eye (C) with the absence of edema on the left (D). After 3 months of treatment with acetazolamide OCT (E) demonstrates the improvement of right optic nerve swelling and reduction of retinal nerve fiber thickness with average RNFL thickness of 93 µm OD and 90 µm OS. 24-2 Humphrey visual field testing (F) shows improvement in the enlargement of the right eye blind spot (MD −0.33 dB; 6% false-positive errors) and ongoing normal field on the left (MD + 0.57 dB; 0% false-positive errors).
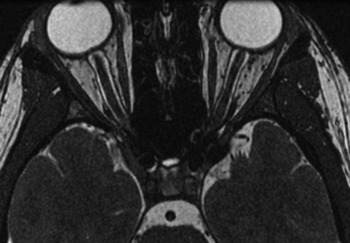
Magnetic resonance imaging (MRI) brain and venogram showed dilatation of the optic nerve sheaths bilaterally with bilateral stenosis of the distal transverse and sigmoid sinuses, no intracranial masses or venous thrombi (Figure 2). Lumbar puncture opening pressure was 28 cm H2O. CSF studies were normal.

Figure 2: Case 2 Axial T2-weighted image demonstrates dilatation of the optic nerve sheaths and flattening of the posterior aspect of the globes.
She was started on acetazolamide 500 mg twice daily and counseled to lose weight. After 3 months, headache, visual blurring, and tinnitus had improved. Funduscopy showed no evidence of papilledema in either eye. Visual acuity was 20/20 –2 OU; Ishihara color plates were 17/17 OU. 24-2 Humphrey visual field testing showed a reduction of the enlarged blind spot (MD −0.33 dB OD, + 0.57 dB OS) (Figure 1F). OCT demonstrated a reduction of RNFL thickness (93 µm OD and 90 µm OS) (Figure 1E). She lost 30 lbs. (BMI 26.1 kg/m2) and acetazolamide was tapered and stopped in 1 year. She has been stable without recurrence of papilledema for 4 years.
A 44-year-old man was referred for right optic disc edema. He had a history of stable headaches since the age of 15 (Case 3). He endorsed bilateral visual blurring without diplopia, transient visual obscurations, or tinnitus. Medical history was notable for obstructive sleep apnea on continuous positive airway pressure, hypertension, dyslipidemia, and depression for which he was on propranolol, rosuvastatin, and paroxetine.
Weight was 225 lbs.; BMI 30 kg/m2. Corrected vision was 20/20 OU. Ishihara color plates were 18/18 OU. Pupils reacted equally to light without RAPD. Visual fields were full to confrontation. Funduscopy showed Frisén grade 3 papilledema OD and normal disc OS. Extraocular movements were full. 24-2 Humphrey fields showed a partial superior arcuate defect and small inferior defect OD (MD −4.18 dB) and eyelid artifact OS (MD −6.26 dB). OCT showed an average RNFL 181 µm OD and 100 µm OS.
MRI confirmed the absence of mass lesions and demonstrated signs of intracranial hypertension with mild edema around the right optic nerve–sheath complex. CTV showed no evidence of thrombosis or stenosis; there was mild dilatation and tortuosity of the bilateral optic nerve sheaths. Bony optic canal diameters on CT were 5.6 × 4.8 mm OD and 5.4 × 4.4 mm OS (21.1 vs. 18.7 mm2). Lumbar puncture opening pressure was 29 cm H2O. CSF studies were within normal limits. He was started on acetazolamide 500 mg twice daily, which he tapered down to 500 mg daily due to frequent urination.
After 10 months, visual acuity remained stable. Funduscopy showed resolution of most of the right disc edema with only slight indistinction of the nasal margins. The left disc continued to appear normal. 24-2 Humphrey fields showed a partial biarcuate defect OD (MD −2.89 dB) and eyelid artifact superior OS (MD −2.34 dB). OCT showed an average RNFL 106 µm OD and 96 µm OS. Given this improvement, he was advised to reduce acetazolamide to 375 mg daily and continue adherence to CPAP for sleep apnea. Weight loss was encouraged, but follow-up weight was unavailable. Right optic disc edema resolved completely in 2 years.
Although the classical ophthalmologic manifestation of IIH is bilateral papilledema, there are reports of unilateral cases. Reference Huna-Baron, Landau and Rosenberg2 This is the first series to demonstrate OCT-confirmed unilateral papilledema; prior reports Reference Huna-Baron, Landau and Rosenberg2–Reference Brosh and Strassman4 have been based on funduscopy alone which may have missed subtle bilateral edema that was highly asymmetric. Cases of highly asymmetric (defined as a difference of two or more Frisén grades between eyes) papilledema are seen in up to 23% of patients with IIH. Reference Lepore3
Several mechanisms have been proposed to account for the gross asymmetry of papilledema in IIH. Underlying each is the principle that papilledema arises from axoplasmic flow stasis within the optic nerve head. Reference Tso and Hayreh5 Experimental models by Hayreh suggest that either increased CSF pressure or low intraocular pressure can result in stasis. Reference Hayreh6 Subsequent studies have failed to demonstrate a strong association between asymmetric intraocular pressures and discordant papilledema. Reference Huna-Baron, Landau and Rosenberg2,Reference Brosh and Strassman4 Our present understanding suggests that axoplasmic stasis occurs secondary to the transduction of elevated CSF pressure to the lamina cribrosa through the perioptic subarachnoid space. Reference Tso and Hayreh5
It has been postulated that age-related loss of compliance in the lamina cribrosa contributes to asymmetric papilledema. Reference Lepore3 Supportively, Bidot’s study of 20 IIH patients with very asymmetric papilledema found a significant association between older age and asymmetric presentation. Reference Bidot, Bruce, Saindane, Newman and Biousse7 As demonstrated in the MRI from Case 2, the optic nerve sheaths were distended bilaterally, which may suggest that variable compliance in the lamina cribrosa mitigates pressure transmission to the optic nerve head. It has also been proposed that microscopic nerve sheath anomalies and variations in the trabecular meshwork Reference Killer, Laeng, Flammer and Groscurth8 might contribute to differences in CSF pressure transduction even when nerve sheath diameters are not significantly different when measured on CT or MRI. Reference Huna-Baron, Landau and Rosenberg2
Additionally, CT cisternography has demonstrated reduced contrast-enhanced CSF communication between the intracranial subarachnoid space and the intraorbital subarachnoid space resulting in optic nerve compartment syndrome in three patients with IIH Reference Killer, Jaggi, Flammer, Miller, Huber and Mironov9 suggesting that varying compartmentalization of the subarachnoid space could result in asymmetric papilledema. Further, Bäuerle and Nedelmann showed that only 5 of the 10 patients with IIH demonstrated a significant reduction in sonographically measured optic nerve sheath diameter following lumbar puncture. Reference Bäuerle and Nedelmann10 The lack of response to lumbar puncture supports the theory of CSF compartmentation in a proportion of IIH patients.
Further, Bidot et al. demonstrated a significant relationship between variant bony optic canal diameter and highly asymmetric papilledema in IIH. In their series, lower grades of papilledema were associated with a smaller diameter bony optic canal. Reference Bidot, Bruce, Saindane, Newman and Biousse7 Mechanistically, they postulate that the tighter canal impedes transduction of CSF pressure from the suprasellar cistern to the perioptic subarachnoid space. Reference Bidot, Bruce, Saindane, Newman and Biousse7
In Cases 1 and 3, there was a respective 14% and 12% difference between optic canal size and the larger canal was associated with papilledema as in Bidot’s study. Unfortunately, Case 2 declined CT to assess the optic canals. Overall, the association between papilledema and optic canal diameter in our patients is acknowledged, but the small difference in diameter is unlikely to fully account for the degree of asymmetry seen.
In summary, unilateral papilledema is a rare manifestation of IIH. The mechanism behind its development is multifactorial with probable contributions from differences in optic canal diameter, variations in microscopic nerve sheath trabeculations, loss of compliance of the lamina cribrosa, and differential compartmentation of the perioptic subarachnoid space. Regardless of pathogenesis, it is important to recognize this unusual presentation as it may respond to treatment with acetazolamide and weight loss to prevent visual deterioration.
Conflicts of Interest
The authors have nothing to report.
Statement of Authorship
ES: wrote and revised the manuscript. PJM: provided analysis of neuroimaging and critical review of the manuscript. ANES: conception and critical review of the manuscript.