Case Summary
A 70-year-old woman with dyslipidemia, longstanding smoking, and known bilateral carotid stenosis (left >70% and right 50–70%) presented with acute onset left hemiparesis, left hemianesthesia with tactile neglect, rightward gaze deviation, and left homonymous hemianopia. Her initial National Institute of Health Stroke Scale score was 12. Noncontract CT head exhibited early ischemic changes in the right posterior cerebral artery (PCA) territory. CT perfusion imaging demonstrated established core tissue in the right PCA territory congruent with ischemic changes on CT. Mean transit time was increased in both the right PCA and middle cerebral artery (MCA) territories. CT angiogram demonstrated occlusions in the proximal right internal carotid artery (ICA), right persistent trigeminal artery (PTA), and P1/P2 junction of the right PCA (Figure 1C and D). Thrombolysis and endovascular thrombectomy were not pursued due to the amount of established infarcted tissue and being outside the thrombolytic time window. Follow-up MRI revealed restricted diffusion in the right PCA territory (Figure 2).

Figure 1: Right posterior cerebral artery and persistent trigeminal artery (PTA) occlusion secondary to ipsilateral internal carotid thrombo-embolism. Prior axial and reconstructed MRI time-of-flight angiogram images demonstrating a patent PTA connecting the distal internal carotid and basilar arteries (open arrowhead, A and B). Axial and reconstructed CT angiogram images demonstrating right ICA occlusion (arrow in C) with reconstructed images showing right PCA (arrowhead in D) and PTA occlusions (asterisk in D).
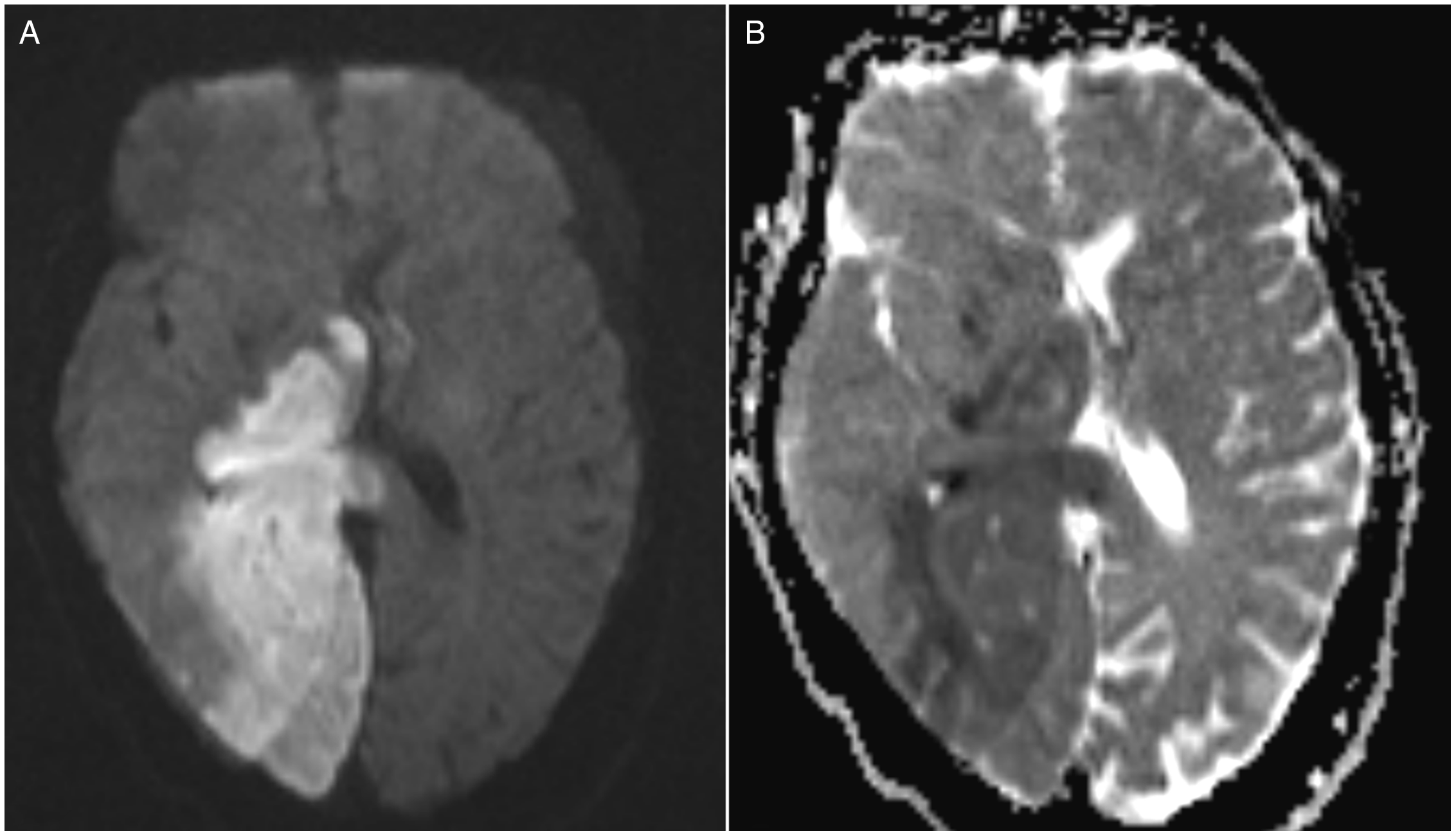
Figure 2: Right posterior cerebral artery infarction secondary to thromboembolic occlusions via persistent trigeminal artery (PTA). Axial diffusion-weighted (A) and ADC (B) MRI demonstrating right PCA territory infarction.
The patient was admitted and subsequent inpatient cardioembolic workup was negative. She was continued on aspirin and high dose statin therapy, with her left hemiparesis improving over the next month, and subsequent transfer to inpatient rehabilitation hospital.
The trigeminal artery, along with the otic artery, the hypoglossal artery, and the proatlantal artery, is an anastomosis between the carotid and vertebro-basilar circulatory systems, developing at approximately 28 days of gestational age. Reference Menshawi, Mohr and Gutierrez1 The incidence of PTA is in the range of 0.1–0.6% and has been reported as secondary cause of trigeminal neuralgia, compressive cranial nerve palsies, and cavernous sinus syndrome from PTA fistulisation. Reference Meckel, Spittau and McAuliffe2 While most cases of PTA with concurrent cerebrovascular disease depict a heightened risk of posterior circulation stroke, Reference Meckel, Spittau and McAuliffe2 a role for the PTA during proximal large vessel occlusion as a protective collateral distally has been described. Reference Xu, Kong, Xu and Wang3
Our case highlights an uncommon cause of posterior circulation infarction with simultaneous anterior circulation hypoperfusion. Our patient’s initial presentation was in keeping with a suspected partial right MCA infarction due to gaze deviation and neglect, but imaging with noncontrast CT and MRI revealed a large isolated right PCA territory infarction. The additional right hemispheric cortical symptoms were likely due to acute occlusion of the right ICA producing transient hypoperfusion in the right MCA territory without causing definite infarction. The mechanism of right occipital infarction was concluded to be artery-to-artery thromboembolism from right carotid disease, with embolism through the PTA.
Acknowledgements
None.
Funding
There is no study funding to report.
Disclosures
Dr. Chu reports no disclosures. Dr. Khan reports no disclosures.
Statement of Authorship
NC performed the patient’s clinical assessment, drafted the manuscript, created the figures, and wrote the corresponding legends. KK assisted in the patient’s clinical assessment and performed a critical revision of the manuscript for intellectual content.




