Reversible cerebral vasoconstriction syndrome (RCVS) is a clinical and radiological entity characterized by recurrent thunderclap headaches with or without other neurological deficits. Reference Calabrese, Dodick, Schwedt and Singhal1 Angiographic studies typically demonstrate multifocal segmental narrowing of cerebral arteries, which by definition resolve within 3 months. An atypical case of RCVS, identified following an atraumatic quadrigeminal cistern subarachnoid hemorrhage (SAH), is described in a patient with well-controlled hypothyroidism post-thyroidectomy.
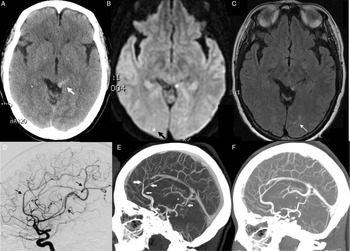
The patient, a middle-aged woman, presented 24-h after the onset of recurrent thunderclap headache occurring while bearing down during stooling. Computed tomography scan revealed a quadrigeminal cistern SAH (Figure 1A). A digital subtraction angiography (DSA) showed areas of cerebral vasoconstriction in the anterior and posterior circulations, but no evidence of aneurysm or venous anomaly were found (Figure 1D). Magnetic resonance imaging subsequently revealed bihemispheric punctate infarctions, and cerebral sulcal convexity SAH (Figure 1B, C). A lumbar puncture revealed cerebrospinal fluid containing 8750 red blood cells/mm3, 7 white blood cells/mm Reference Marder, Narla, Fink and Tozer Fink3 , and normal protein. Vasculitis and inflammatory markers were negative. A diagnosis of RCVS was made, and the patient was successfully treated with a course of nimodipine for symptom relief. Reversibility of the vessel changes was demonstrated on repeat CTA 10 weeks after the onset of symptoms (Figure 1F).
Figure 1: The initial CT scan showed a SAH in the quadrigeminal cistern (A) and CT-angiogram images showed areas of anterior cerebral artery (ACA) narrowing (E) A subsequent digital subtraction angiography demonstrated multifocal involvement in the ACA and middle cerebral artery as well as the posterior circulation (D). MRI revealed punctate ischemic hits (B) and left paramedian occipital sulcal convexity SAH (C). The multifocal vascular abnormalities (E) were shown to have resolved in a repeat CTA 10 weeks after presentation (F). CT, computed tomography; MRI, magnetic resonance imaging; SAH, subarachnoid hemorrhage.
Approximately 30%−50% of RCVS cases are complicated by SAH, Reference Ducros, Fiedler, Porcher, Boukobza, Stapf and Bousser2,Reference Marder, Narla, Fink and Tozer Fink3 and RCVS diagnostic criteria require the exclusion of aneurysmal SAH. Reference Calabrese, Dodick, Schwedt and Singhal1 When imaging is performed within 5 days of SAH onset, the distribution of the hemorrhage may guide the differential diagnosis. Reference Muehlschlegel, Kursun, Topcuoglu, Fok and Singhal4 Diffuse suprasellar or basal cistern SAH is typically caused by saccular aneurysm rupture, whereas perimesencephalic SAH more likely due to nonaneurysmal hemorrhage. Isolated cerebral convexity SAH is commonly caused by cerebral amyloid angiopathy as well as RCVS, and can also be due to posterior reversible encephalopathy syndrome (PRES) or cerebral venous thrombosis. Reference Muehlschlegel, Kursun, Topcuoglu, Fok and Singhal4 In a large retrospective study on RCVS with SAH, all 38 patients had subarachnoid blood located in the hemispheric convexities. Reference Marder, Narla, Fink and Tozer Fink3
In this patient, an aneurysm was ruled out by DSA, and the presence of multifocal vessel narrowing precluded other SAH categorizations such as cryptogenic “angiogram negative” SAH or idiopathic perimesencephalic hemorrhage. It was therefore concluded that the patient´s quadrigeminal cistern SAH was indeed secondary to RCVS. “Idiopathic” perimesencephalic hemorrhages are theorized to be caused by venous rupture Reference Van der Schaaf, Velthuis, Gouw and Rinkel5 and blood is by definition confined to the perimesencephalic cisterns centered immediately anterior to the brainstem. Nonetheless, nonaneurysmal perimesencephalic hemorrhages with blood centered in the quadrigeminal cistern have been reported, with a similar proposed etiology and course to that of the classic pretruncal variant. Reference Wallace, Vyhmeister and Viets6 A case of PRES has been described in association with perimesencephalic SAH with no evidence of vasospasm. Reference Iyer, Ramalingam, Akhtar and Muthukalathi7 The pathophysiologic mechanism of SAH in RCVS remains unknown, but abrupt stretching of vessel walls with or without small vessel rupture, or reperfusion injury have been proposed as possible mechanisms. Reference Ducros, Fiedler, Porcher, Boukobza, Stapf and Bousser2 In the present case, the hemorrhage within the quadrageminal cistern was distant from the Circle of Willis or any other artery, further supporting the venous theory. This is further substantiated by the history of intense valsalva coinciding with the thunderclap headache. Reference Matsuyama, Okuchi, Seki, Higuchi and Murao8
Disclosures
Dr Camara-Lemarroy reports personal fees from EMD SERONO, outside the submitted work. The remaining authors have no conflicts of interest to report.
Statement of Authorship
Dr GS, Dr KS, Dr MK, and EM gathered the clinical information, performed chart review, provided images, and revised the manuscript. Dr CRC-L wrote the manuscript and approved the final version.