Introduction
Migraine, along with other headache disorders, is the second leading cause of disability worldwide, and the leading cause of years lived with disability among those aged 15–49 years. 1,Reference Steiner, Stovner, Vos, Jensen and Katsarava2 An estimated 8.3% of Canadians (2.7 million) reported having been diagnosed with migraine in the 2010–2011 Canadian Community Health Survey, Reference Ramage-Morin and Gilmour3 although this estimate is likely higher as migraine is typically underdiagnosed.
Migraine attacks are often treated with acute medications including nonspecific, over-the-counter analgesics, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), as well as migraine-specific prescription medications such as triptans. Reference Lipton and Silberstein4 Preventive medications are another avenue of treatment for patients with migraine. According to the Canadian Headache Society, preventive medications are recommended for patients with a high burden of migraine, patients who may be at risk for medication overuse, and those who may have contraindications with acute medications. Reference Pringsheim, Davenport and Mackie5 As overuse of acute medications can lead to medication overuse headache (MOH); therefore, preventive medications are crucial in improving patient outcomes, particularly in patients who have frequent migraine attacks and are at risk of acute medication overuse. Reference Pringsheim, Davenport and Mackie5 Behavioural or non-pharmacological interventions can also be used to mitigate migraine attacks, using techniques such as behavioral therapy, trigger management, and adjustment of lifestyle factors. Reference Pringsheim, Davenport and Mackie5 A study from Canada found that opioid prescriptions to treat migraine was not uncommon, particularly in patients with chronic migraine. Reference Richer, Wong and Martins6 Opioids, when prescribed, have a higher-than-average proportion of potentially risky prescription durations, with 28.1% of prescriptions lasting longer than 7 days. Reference Pasricha, Tadrous and Khuu7 This is despite opioid-related harms reportedly outweighing any potential benefits. Reference Casucci and Cevoli8,Reference Tepper9 For example, frequent use of opioids is linked to an increased likelihood of developing MOH and/or the chronification of episodic migraine to chronic migraine. Reference Bigal and Lipton10 Due to the limited evidence evaluating the efficacy of opioids for treating migraine and significant risks, Canadian guidelines recommend against using opioids in place of other standard medications for both emergency and routine use. Reference Orr, Aubé and Becker11 Triptans are generally considered to be the most effective acute migraine medication, but only 8% of Canadian women reported using a triptan as their primary migraine medication in 2005. Reference Worthington, Pringsheim and Gawel12 More recent estimates of real-world treatment patterns in Canada are needed, to evaluate adherence to treatment guidelines and identify areas for improved care for individuals suffering from migraine.
Migraine is associated with increased healthcare resource utilization (HRU), compared to the general population, Reference Cooke and Becker13–Reference van Walraven and Colman15 with greater use among those with chronic versus episodic migraine. A Canadian study reported that 48.2% of patients with chronic migraine had a general practitioner visit related to headache in the past 3 months compared to only 12.3% of patients with episodic migraine. Reference Stokes, Becker and Lipton16 Migraine has a significant economic burden, with prescription medications and healthcare provider visits being the main direct healthcare costs in Canada. Reference Amoozegar, Khan, Oviedo-Ovando, Sauriol and Rochdi17 High- and low-frequency episodic migraine had estimated annual costs of $24,885 and $15,651, respectively, while chronic migraine had the highest estimated annual cost at $25,669 per patient. Reference Amoozegar, Khan, Oviedo-Ovando, Sauriol and Rochdi17 Comorbidities may be contributing. It was estimated that 70% of patients with chronic migraine and 42% of patients with episodic migraine take at least one drug other than for headache treatment. Reference Ferrari, Leone and Vergoni18 People with migraine were more likely to report comorbid conditions such as depression, anxiety, cardiovascular diseases, inflammatory disorders, and asthma. Reference Buse, Reed and Fanning19 Additionally, indirect healthcare costs, due to absenteeism and presenteeism, contribute significantly to the costs associated with migraine. Reference Bonafede, Sapra, Shah, Tepper, Cappell and Desai20,Reference Linde, Gustavsson and Stovner21
Although previous publications have examined HRU and cost of migraine, there is limited current real-world, population-level data examining the overall burden of migraine in Canadian populations, particularly the treatments prescribed to help manage symptoms. The study aimed to understand the current management strategies and overall burden among newly diagnosed or recurrent patients with migraine, to identify opportunities to improve the treatment approach for migraine as early as possible in the disease course. Specifically, the study objectives were to examine the demographic and clinical characteristics, treatment patterns, HRU, and associated costs of patients with new or recurrent migraine in Alberta, Canada using administrative healthcare data.
Methods
Study Design and Data Sources
This retrospective observational study examined a cohort of patients with new or recurrent migraine over a study period from April 1, 2010, to March 31, 2020, in Alberta, Canada. Administrative data were requested and approved for release by Alberta Health (Government of Alberta Ministry of Health) and included data from the provincial Alberta Blue Cross (ABC) Pharmacy Claims, National Ambulatory Care Reporting System (NACRS), Discharge Abstract Database (DAD), Pharmaceutical Information Network (PIN), Population Registry, Practitioner Claims, and Vital Statistics (deaths) datasets. 22 The data were released to the study team with anonymous identifiers, which are consistent across datasets to allow for the linkage between datasets. More details regarding the variables included in each database are available from Alberta Health. 22 The study period was selected based on the time period for which all databases have comprehensive population-level data.
Case Definitions for the Total Migraine Cohort and Sub-Cohorts
The Total Migraine Cohort included adult patients who met the case definition for migraine, which was adapted from the algorithm developed by Muzina et al. (2011). Reference Muzina, Chen and Bowlin23 Cases met the inclusion criteria if, between April 1, 2012, and March 31, 2018, they had: (1) ≥1 International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM)/International Statistical Classification of Diseases, and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) diagnostic code(s) for migraine in the DAD, NACRS, or Practitioner Claims datasets; or (2) ≥1 prescription dispense(s) for triptan, an acute migraine-specific medication. The primary population of interest (referred to as the Total Migraine Cohort) focused on patients with a new diagnostic code or dispensation for migraine; therefore, a two-year washout period was applied (April 1, 2010–March 31, 2012), removing any patients with a diagnostic code or dispensation prior to April 1, 2012, from the Total Migraine Cohort. In recognition of the possibility that some of the patients with a new diagnostic code could have had migraine before the 2-year washout period, we classified the identified patients as “newly diagnosed or recurring” (for those who could have had migraine before the washout period). The index date was defined as the first (earliest) ICD-9-CM/ICD-10-CA code for migraine appearing in any position in the DAD, NACRS, or Practitioner Claims datasets or the first pharmacy claim for a triptan appearing in the PIN or ABC datasets within the case ascertainment period (April 1, 2012–March 31, 2018). Patients were followed until the first of the following events: death, moving out of the province, or the end of follow-up on March 31, 2020. Patients were excluded if they were: (1) aged<18 years at the index date; (2) missing data for age or sex, or (3) had no records of insurance coverage eligibility in the Alberta provincial registry. Diagnostic codes and algorithm details can be found in Supplementary Material 1.
The following five migraine sub-cohorts were derived from the Total Migraine Cohort: (1) Medication Overuse Headache; (2) Patients with ≥2 Stopped Preventive Medications; (3) Patients with ≥3 Stopped Preventive Medications; (4) Emergency department (ED) visit for migraine; and (5) chronic migraine. The case definitions of these cohorts can be found in Supplementary Material 2. The sub-cohorts are reported for descriptive purposes only and results will be outlined in separate manuscripts, as the focus of this manuscript is on the Total Migraine Cohort.
Baseline Variables and Outcomes
Demographic and clinical characteristics of interest as of the index date included age, sex, geography (Alberta Health Zone), the Charlson Comorbidity Index (CCI; Supplementary Material 3), Reference Charlson, Pompei, Ales and MacKenzie24,Reference Quan, Li and Couris25 and common comorbidities (defined using ICD diagnostic codes in Supplementary Material 4). Treatment utilization during study follow-up was evaluated by class of therapy (e.g., acute and preventive medications) as well as by medication type within each class. Acute medication types included NSAIDs, triptans, antiemetics, and opioids. Preventive medications included antihypertensives (beta-blockers, calcium channel blockers, angiotensin II receptor blockers), anticonvulsants, antidepressants (tricyclic antidepressants, serotonin, and norepinephrine reuptake inhibitors), neurotoxins (onabotulinumtoxinA), monoclonal antibodies (i.e., anti-calcitonin gene-related peptide receptor antagonists [anti-CGRP), and antamines (i.e., pizotifen). The specific anatomical therapeutic chemical codes for acute and preventive medication classes are shown in Supplementary Material 5 and 6, respectively. Of note, anti-CGRP monoclonal antibodies were not yet available in Canada within the study period. The estimated annualized number of days covered (days’ supply as specified on the prescription) was used to examine medication use. The number of days a medication was available was adjusted for overlap in prescriptions.
HRU endpoints of interest included ED visits, hospitalizations, and physician encounters. Visits were reported separately for all-cause and migraine-related (i.e., migraine diagnostic code in any position) episodes of care, while physician encounters were stratified by speciality (general practitioner [GP]/family physician [FP] and specialist [SP]). Healthcare costs associated with physician claims, hospitalizations, and ED visits are reported by all-cause and migraine-related visits. Total healthcare costs were calculated for each patient as the sum of all medication, hospitalization, ED, physician, diagnostic imaging, and ambulatory costs.
Statistical Analysis
All analyses of baseline characteristics and follow-up data were conducted using the Total Migraine Cohort, which included all newly diagnosed or recurrent migraine patients. For each included patient, the follow-up period started from index date up to the earliest of death, moving out of the province, or the end of follow-up on March 31, 2020. Baseline characteristics were summarized as means and standard deviations (SDs) for continuous variables and counts and proportions for categorical variables. Variables with missing data were reported. Pharmacy claims were summarized as the total number of acute and preventive medications dispensed, the rate of medication dispenses per person-year, the number and proportion of patients with at least one medication dispense, the rate of medication dispenses per person-year among patients with at least one dispense, and the distribution of dispenses by prescriber speciality. The annualized days covered for each medication were summarized descriptively using means and SDs, reported in six-month period increments, over a two-year period from the first prescription dispense date post-index. Estimates for each six-month period were adjusted for the number of patients remaining in the cohort (i.e., uncensored) at the start of the six-month interval.
All HRU endpoints of interest were summarized as the number and proportion of patients in the cohort and patients with at least one event and as the mean and SD of events per person-year. Total costs per person-year were summarized as means and SDs. Costs were normalized to 2020 constant Canadian dollars using Statistics Canada’s all-items Consumer Price Index. All analyses were performed using SAS 9.4 (SAS Institute, Cary, North Carolina).
Ethics
The study was approved by the Health Research Ethics Board of Alberta – Community Health Committee.
Reporting
The study followed the reporting standards set by the A STrengthening the Reporting of Observational studies in Epidemiology statement. Reference Vandenbroucke, von Elm and Altman26
Results
Demographics and Clinical Characteristics
The Total Migraine Cohort included 199,931 patients identified between April 1, 2012, and March 31, 2018 (Fig. 1), with a median follow-up of 2.9 person-years. The mean (SD) age for the Total Migraine Cohort was 40.0 (14.9) years, with the majority (54.3%) of patients under age 40. Nearly three-quarters (72.3%) of the cohort was female and lived in one of Alberta’s two largest cities (Calgary: 40.7% and Edmonton: 29.4%). Additionally, more than 20% had a CCI score of ≥1, an indicator of mortality risk (Table 1). The most common clinical comorbidities were depression (19.7%), cardiovascular disease (e.g., hypertension, dyslipidemia, and stroke) (18.9%), and anxiety (16.6%). Nearly 20% of the cohort were identified with chronic migraine within one year of index and 22.7% visited an ED due to their migraine over follow-up.
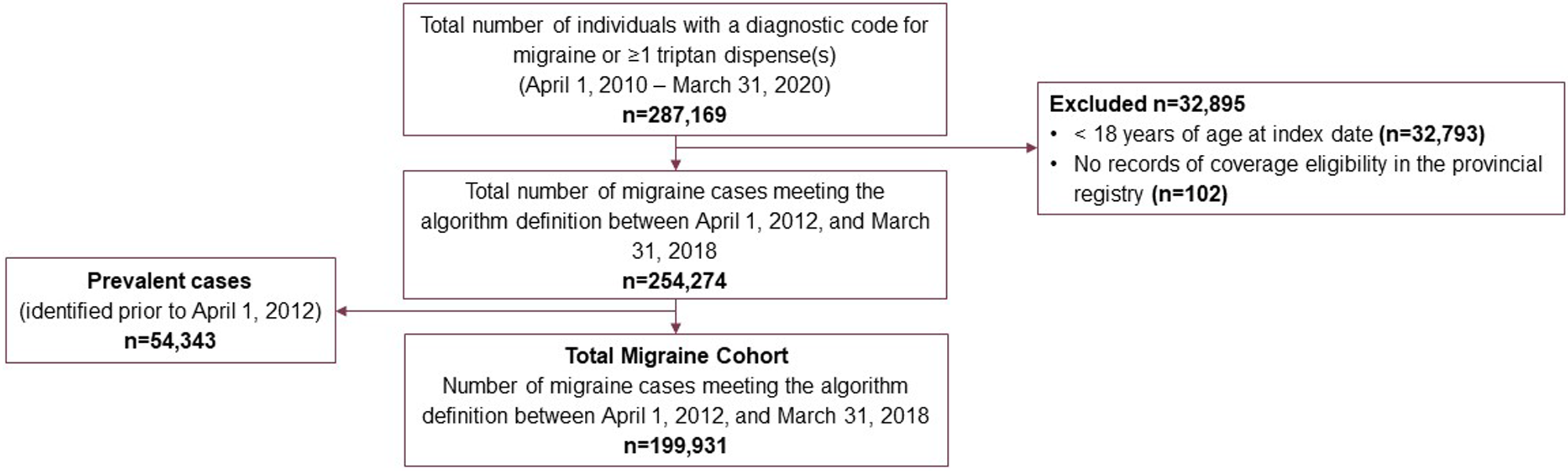
Figure 1: Derivation of the Total Migraine Cohort in Alberta, Canada, 2012–2018.
Table 1: Demographic characteristics of the total migraine Cohort, in Alberta, Canada, 2012–2018
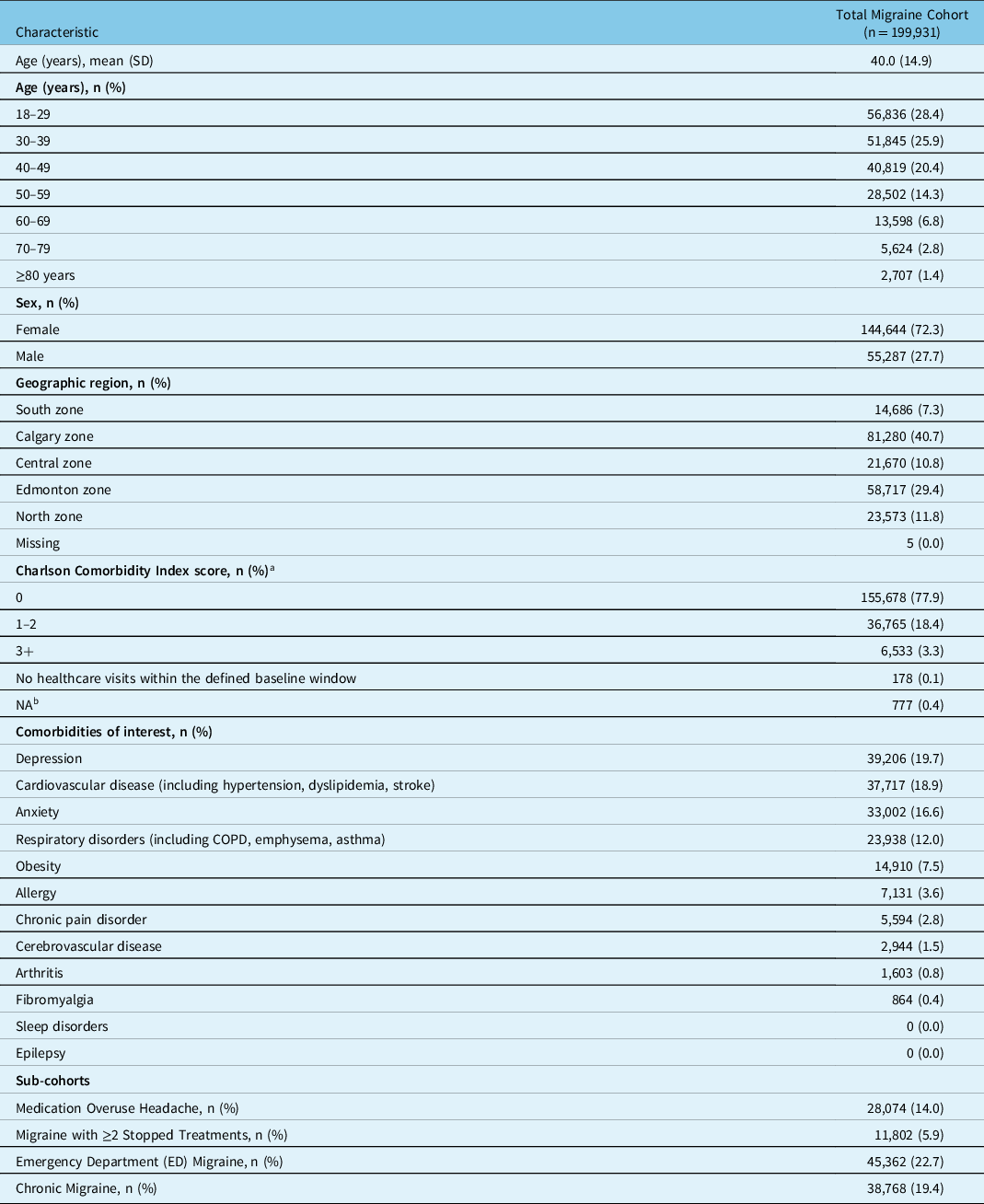
COPD = chronic obstructive pulmonary disorder; NA = not applicable; SD = standard deviation.
a The Charlson Comorbidity Index (CCI) Score is derived from the Discharge Abstract Database, National Ambulatory Care Reporting System, and practitioner claims, 2 year prior to or on index date. Based on Quan 2011, for hospitalizations on index date, do not use type M or type 2. For hospitalizations prior to index, use any diagnosis type.
b Individual was out of province at some point in the 2-year pre-index period.
Treatment Patterns
The most frequently prescribed class of acute medications across all providers over the study follow-up period was opioids, with a mean (SD) of 1.88 (12.79) medications dispensed per person-year. This was followed by triptans (mean [SD]: 0.75 [5.25]), NSAIDs (mean [SD]: 0.46 [3.34]), and antiemetic medications (mean [SD]: 0.24 [2.69]) (Table 2). Similarly, the proportion of patients receiving≥1 prescription dispense was the highest for opioids (40.84%), followed by NSAIDs (36.56%), triptans (32.88%), and antiemetic medication prescriptions (15.55%) (Table 2). The distribution of prescription dispenses by prescriber specialty showed that most prescriptions were issued by GPs/FPs; dispenses by SPs accounted for approximately one-tenth of prescription dispenses.
Table 2: Acute medication prescription dispenses per person-year among all patients and patients with ≥1 prescription dispenses, in Alberta, Canada, 2012–2018

NSAIDS = nonsteroidal anti-inflammatory drugs; SD=standard deviation.
Preventative medication utilization was lower than acute medication, with less than one-fifth of patients prescribed a migraine preventive in each medication class examined (Table 3). The highest overall mean [SD] number of prescription dispenses per person-year was observed for anticonvulsants (0.72 [7.39]), followed by antidepressants (0.70 [5.71]). Monoclonal antibodies and antamines both had a mean of <0.01 prescription dispenses per person-year. The largest proportion of patients receiving≥1 prescription dispense was observed for antidepressants (19.12%) followed by anticonvulsants (13.40%). Among patients who received ≥1 dispense of each medication, those who received anticonvulsants had the highest mean [SD] number of prescription dispenses overall (5.36 [19.57]), followed by antidepressants (3.68 [12.63]) (Table 3). SP’s accounted for a greater proportion of preventative prescription dispenses than acute medication, accounting for approximately one-third of all preventative dispenses. SPs had a higher proportion of dispenses than GPs/FPs for neurotoxin (52.6% compared to 38.3%, respectively).
Table 3: Preventive medication prescription dispenses per person-year among all patients and patients with≥1 prescription dispenses, in Alberta, Canada, 2012–2018
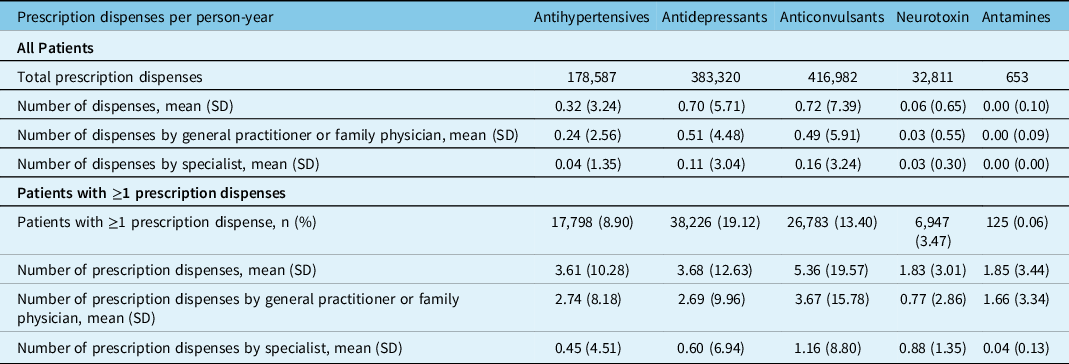
SD = standard deviation.
The mean (SD) number of days covered per year for acute and preventive medications are shown in Figure 2 and Figure 3, respectively. For NSAIDS, triptans, antiemetics, and all preventive medications, the mean number of days covered per year decreased from 0 to 6 months to>18–24 months, with the greatest decrease occurring from 0 to 6 months to >6–12 months. Notably, the mean [SD] number of days covered for patients dispensed opioids decreased from 0 to 6 months (64.9 [97.9]) but slightly increased from >6 to 12 months (47.1 [102.7]) to >18–24 months (50.6 [108.3]).
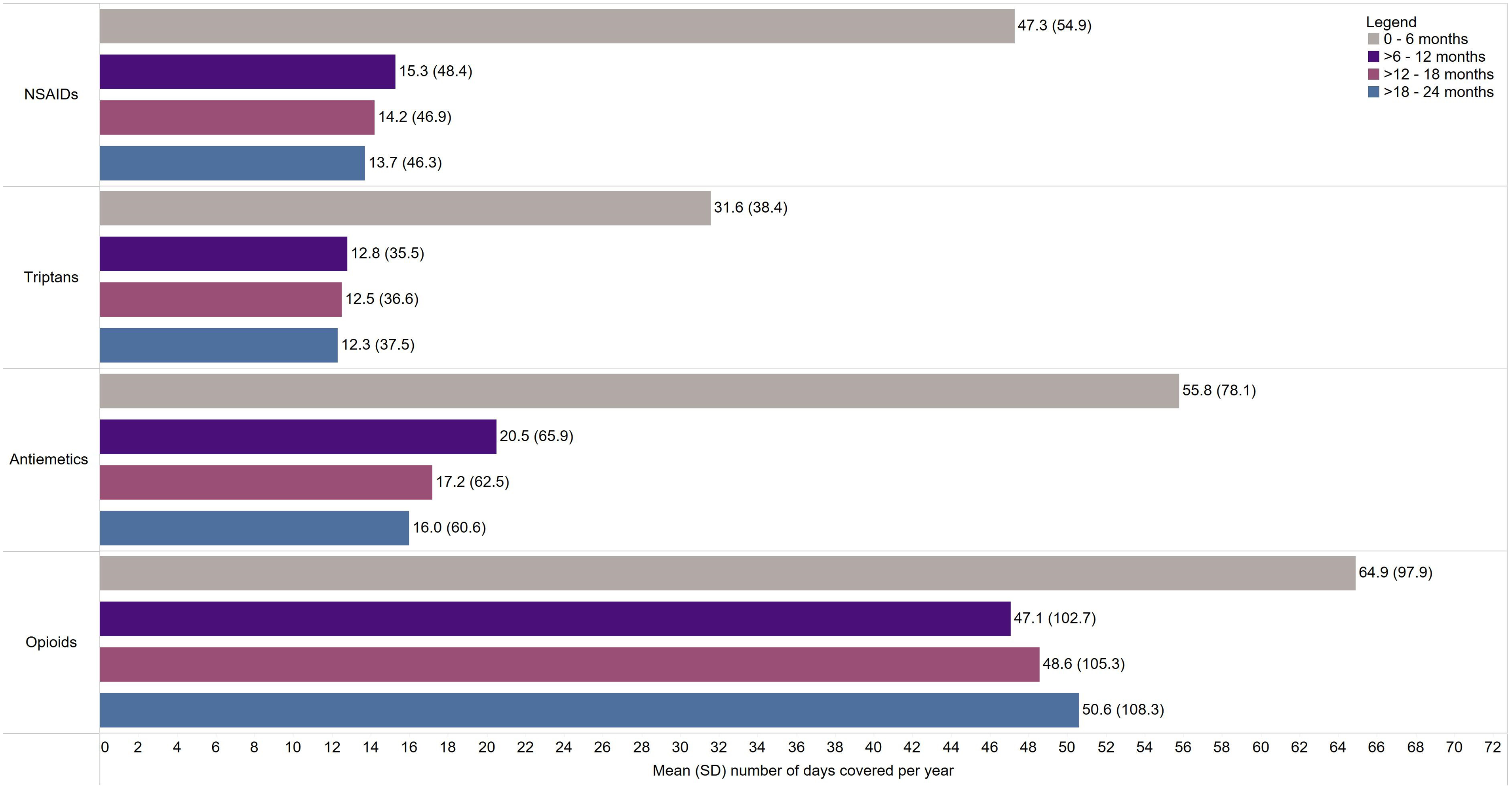
Figure 2: Number of days covered for acute migraine-related prescription dispenses per patient per year for patients with ≥1 dispense in Alberta, Canada, 2012–2018. Abbreviations: NSAIDs = nonsteroidal anti-inflammatory drugs; SD = standard deviation.
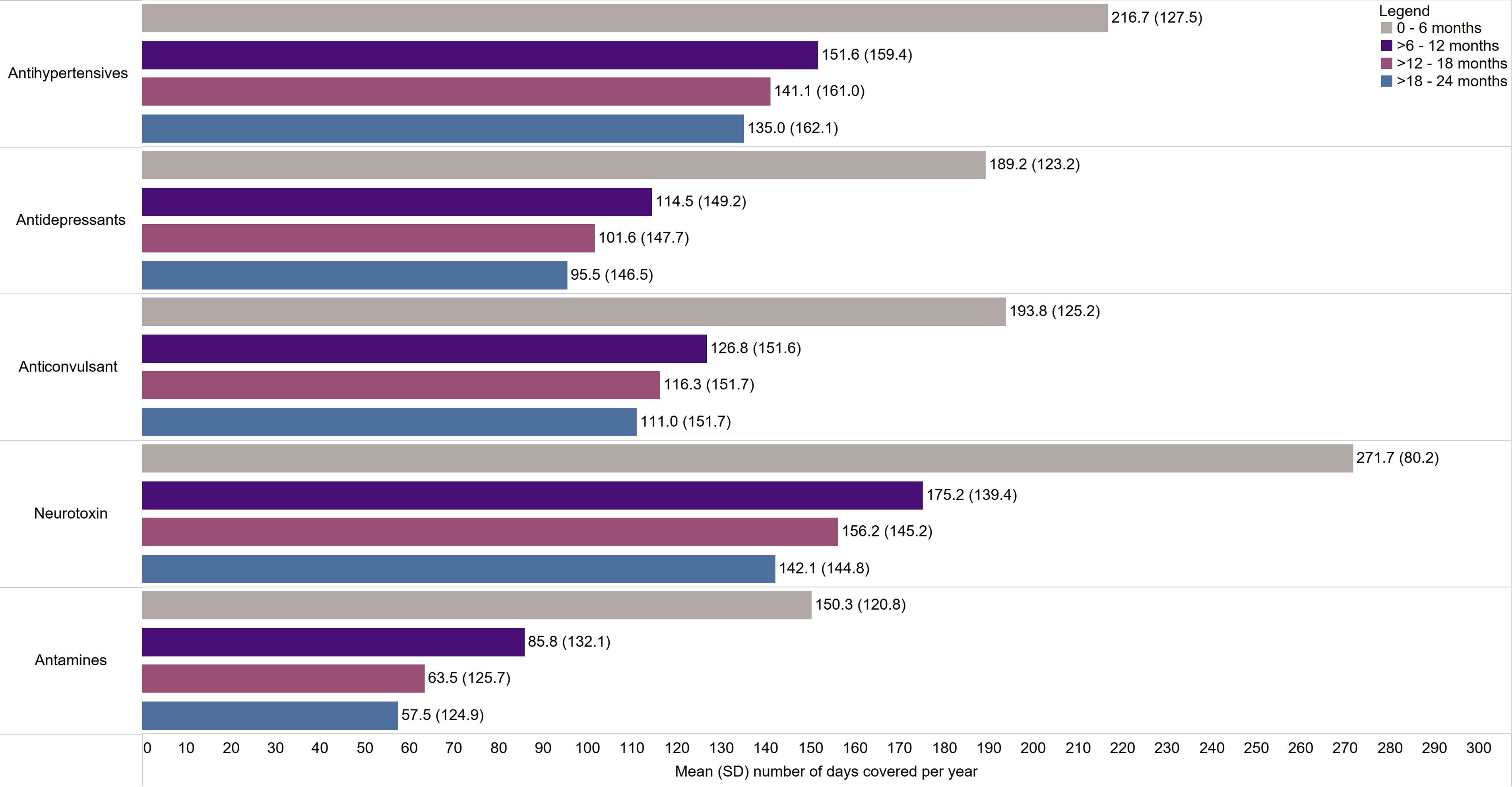
Figure 3: Number of days covered for preventive migraine-related prescription dispenses per patient per year for patients with ≥1 dispense in Alberta, Canada, 2012–2018. SD = standard deviation.
HRU and Costs
The mean (SD) annualized rates of all HRU endpoints are in Figure 4. There were 80,215 hospitalizations observed for the Total Migraine Cohort over follow-up, corresponding to a mean (SD) all-cause hospitalization rate of 0.21 (3.20). There were 620,961 ED visits, with a mean (SD) all-cause visit rate of 1.41 (7.71) over the study period. Migraine-related hospitalizations accounted for 2.50% (n = 2,006) of all hospitalizations, while migraine-related ED visits accounted for 9.89% (n = 61,261) of all ED visits recorded. Most physician visits were GP/FP visits, accounting for 64.2% of all visits. There were 4,535,499 total GP/FP visits over the study period, corresponding to a mean (SD) annual visit rate of 9.15 (14.88), compared to 2,374,403 SP visits at a mean (SD) annual rate of 4.65 (11.09). Like hospitalizations and ED visits, migraine-related GP/FP visits accounted for less than one-tenth of visits; migraine-related visits accounted for 5.89% (n = 267,083) of all physician visits and 3.09% (n = 73,485) of all SP visits.

Figure 4: All-cause and migraine-related healthcare resource use per patient per year in Alberta, Canada, 2012–2018. FP = family physician; GP = general practitioner; SD = standard deviation.
The total all-cause mean (SD) healthcare costs for all HRU endpoints were $6,403 ($39,880) per patient annually. Annual costs by HRU endpoints of interest, including ambulatory care, are shown in Figure 5. Hospitalization visits represented the single largest category of healthcare costs, accounting for a mean (SD) of $2,418 ($30,565) per person-year. These costs were largely driven by non-migraine-related visits, with migraine-related hospitalization averaging under $50 per person-year. Consistent with hospitalization visits, the distribution of hospitalization costs was skewed toward high utilizers, with more than 75% of the patients incurring no hospital costs. The next largest expenditure category for all-cause costs was physician visits (mean [SD]: $1,974 [$7,271]). Although SP visits were less common than GP/FP visits, the annual cost of SP visits per person-year (mean [SD]: $1,152 [$6,424]) exceeded that of GP/FP visits (mean [SD]: $799 [$2,332]). ED visits were the smallest category of all-cause healthcare costs, with a mean (SD) of $616 ($5,063) per person-year; these costs were largely driven by non-migraine-related visits.

Figure 5: Annual all-cause and migraine-related healthcare costs (in 2020 CAD) per patient per year, in Alberta, Canada, 2012–2018. FP = family physician; GP = general practitioner; SD = standard deviation.
Discussion
This study presents real-world evidence on the burden of diagnosed migraine in a retrospective study of newly diagnosed or recurrent patients residing in Alberta, Canada. Nearly 20% were categorized with chronic migraine, and just over 20% visited the ED due to their migraine. Notably, this study suggests an underutilization of acute and preventive medications and overutilization of highly addictive opioids in the management of migraine. HRU and costs were mainly driven by causes other than migraine, suggesting a high burden of comorbidities among patients in our study.
Evidence from the literature has shown that migraine is historically underdiagnosed and therefore, undertreated. The mean age of cohort entry in our study (40.0) was higher than the mean age of diagnosis of 26.2 years as reported in one Canadian study. Reference Ramage-Morin and Gilmour3 This observation suggests that some patients may have suffered without a diagnosis and clinical management for a significant portion of their lives or a large proportion of patients included in the cohort were experiencing a recurrence of migraine or an increase in severity of migraine requiring medical care.
The results highlight an underutilization of effective acute and preventive medications for patients with new or recurring migraine. Triptans are migraine-specific medications that are recommended as a second line of acute treatment by the Canadian Headache Society and are effective when used early; however, less than one in three of the Total Migraine Cohort tried triptans at least once. A possible reason for the low observed usage of triptans is that triptans are not included on the Alberta Formulary; 27 therefore, access may be hindered by special authorization processes and limited to patients with private coverage. Additionally, although a substantial number of patients with high frequencies of migraine would benefit from preventive therapy, not many receive it. Reference Pringsheim, Davenport and Mackie5 Several reasons may contribute to this finding, including underdiagnosis and treatment of migraine and reluctance or lack of compliance by patients due to side effects. Reference Martin, Feoktistov and Solomon28 As observed in the present study, fewer than one-fifth of patients were prescribed preventive medications for migraine in each class examined. As the study population focused on new and reoccurring patients, it is possible that preventative medication use may increase with longer follow-up should symptoms persist. Similar suboptimal prescription rates of acute and preventive medication use have been reported previously in Canada and the United States. Reference Cooke and Becker13,Reference Amadio, Lee and Yao29,Reference Woolley, Bonafede, Maiese and Lenz30 The current treatment of migraine in Alberta is indicative of unmet needs and inadequate management of migraine, which can lead to suboptimal outcomes for patients.
According to the Canadian guidelines for migraine management, opioids are not recommended for routine use in the treatment of migraine. Reference Worthington, Pringsheim and Gawel12,31 Despite this recommendation, the most prescribed acute medications per patient-year in Alberta were opioids. These findings are concerning given that prolonged opioid use may lead to more severe headache disability, such as progression to MOH and increased HRU for headache, comorbidities, and dependance. Reference Buse, Pearlman, Reed, Serrano, Ng-Mak and Lipton32 Awareness regarding opioid risks and education for healthcare practitioners may help reduce inappropriate prescribing patterns. Reference Casucci and Cevoli8 Future research aimed at understanding the characteristics of patients or settings in which opioids are prescribed may tailor this education and identify opportunities for improved care.
Treatment adherence and persistence are prominent concerns surrounding patients with migraine. According to a systematic review of oral preventive medications, adherence ranged from 41%–95% at two months and declined to 35%–56% at 12 months for observational studies, specifically. Reference Hepp, Bloudek and Varon33 In a study examining individuals with chronic migraine, persistence to initial preventives was 25% at six months and 14% at 12 months. Reference Hepp, Dodick and Varon34 Adherence to available preventive regimens may be more challenging for individuals with chronic migraine or other comorbid conditions that require additional medication. Reference Ramsey, Ryan, Hershey, Powers, Aylward and Hommel35,Reference Zebenholzer, Lechner and Broessner36 Consequently, patients with migraine – especially those with more severe or frequent symptoms – face a greater risk of unmet needs for symptom management and prevention. In the present study, the number of days covered decreased for preventive medications over the follow-up periods, with a notable decline from 0 to 6 months to >18–24 months. This finding was consistent with a study in the US, which found that most patients with migraine discontinued preventive medications by the first year. Reference Woolley, Bonafede, Maiese and Lenz30 The decrease in use of preventives over time, may in part, be due to a lack of effect, side effects, or tapering of medications after successful therapy, as recommended by Canadian guidelines. Reference Pringsheim, Davenport and Mackie5 With regard to opioids, the number of days covered increased from >6–12 months to >18–24 months, which suggests persistent and recurring use and the mismanagement of migraine.
Evidence from the literature indicates that people with migraine use more healthcare resources compared to people without migraine Reference Cooke and Becker13–Reference van Walraven and Colman15,Reference Bonafede, Sapra, Shah, Tepper, Cappell and Desai20 and subsequently incur more healthcare costs. Reference Bonafede, Sapra, Shah, Tepper, Cappell and Desai20 Specifically, patients with migraine were found to have an increased risk of ED visits and visits to GPs and SPs. Reference Wolfson, Fereshtehnejad, Pasquet, Postuma and Keezer14 In a study conducted in the United States, the total mean annual direct costs was over two times higher in patients with migraine compared to a matched cohort of patients without migraine; patients with migraine also had overall higher indirect costs. Reference Bonafede, Sapra, Shah, Tepper, Cappell and Desai20 In the present study, HRU and costs were mainly driven by causes other than migraine. This observation may be attributed to the presence of comorbidities among patients with migraine. Consistent with the literature, migraine is associated with a range of comorbidities, specifically psychiatric comorbidities and cardiovascular diseases. Reference Amoozegar, Khan, Oviedo-Ovando, Sauriol and Rochdi17,Reference Dresler, Caratozzolo and Guldolf37,Reference Wang, Chen and Fuh38 A study in the United States examining headache pain and frequency in a cohort of migraine patients found that headache pain intensity was associated with increased risk of gastric ulcer disease, inflammatory disorders, and psychiatric and sleep conditions, while headache frequency increased risk for most comorbidities examined. Reference Buse, Reed and Fanning19 Such evidence suggests that improved migraine management may positively impact comorbidities and all-cause HRU.
Strengths of this study include the large sample size and the use of population-level data, which limited the amount of missing data, and loss of follow-up. Additionally, the PIN database captures all pharmacy prescription dispenses (private and public), enabling a comprehensive analysis of prescription treatment patterns. This allowed for a comprehensive evaluation of burden of illness, including treatment burden, HRU, and costs, which are typically difficult to capture in a single study.
Although administrative data is valuable for population-level data analyses, there are some methodological limitations inherent to any “real-world” observational study. The PIN database captures dispensations of prescription medication only, which may overestimate what patients actually take. Information regarding the use of over-the-counter drugs (e.g., ibuprofen or acetaminophen 1,000 mg) is also not available in administrative data since they are not obtained by prescription. Further, the PIN does not include in-hospital dispenses. 22 As administrative data is not gathered specifically for research purposes, there is the potential for misclassification as ICD codes are not a confirmed diagnosis of disease and many patients with migraine will not have received a formal diagnosis; therefore, would not be represented in this cohort. This is also true for the comorbidities, as our study found low rates of many comorbidities (e.g., obesity, sleep disorder), which may indicate a lack of formal diagnosis or the two-year wash out period may have been insufficient to identify comorbidities. Patients in the cohort included those who received triptan; in addition to migraine, triptans can be used to treat other conditions such as cluster headaches, which can contribute to possible misclassification bias. Additionally, patients included in the sample required medical encounters associated with migraine to enter the cohort, which would omit less severe patients who are able to manage their symptoms with over-the-counter medications or without seeking medical care, thereby limiting the generalizability of the study. Further, this study focused on new and recurrent cases of migraine and omitted patients who had a migraine diagnostic code or dispensation between 2010 and 2012. Given migraine symptoms can fluctuate over time, this study was not able to differentiate between new and recurrent cases as the look-back period ended in 2010. As the study was descriptive in nature, study outcomes did not adjust for baseline covariates, which makes it difficult to attribute observed trends to migraine rather than preexisting or co-occurring medical conditions or other patient characteristics. Lastly, the study did not account for unmeasured HRU-related risk factors such as family history.
Conclusions
This retrospective observational cohort study examined a cohort of newly diagnosed or recurrent patients with migraine in Alberta. HRU and associated costs were mainly for other causes than migraine, suggesting a high burden of illness due to comorbidities. A key finding from the study was the underutilization of acute and preventive medications in the treatment of migraine, and an overutilization of opioids, which indicates a mismanagement of migraine. The high rate of opioid use for this study population is an important and concerning finding and highlights a need for additional research into the reasons for opioid use and into new approaches for effective management of migraine. Additionally, the results highlight the need to educate healthcare professionals to recognize and optimize treatment strategies to better manage migraine.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cjn.2023.299.
Acknowledgements
We would like to acknowledge Lundbeck Canada Inc. for sponsoring this study. We would like to acknowledge Claire Sharp and Heather Neilson who assisted with the writing of the manuscript.
Author contribution
JB, MH, MPL, and FA co-conceived the study, interpreted the results, and critically revised the manuscript. EG, TC, SM, and PE designed the study methodology, analyzed and interpreted the data, and critically revised the manuscript. TP and MM interpreted the data and wrote the first draft of the manuscript.
Competing interests
EG, TC, SM, PE, TP, and MM are employed by Medlior Health Outcomes Research Ltd who received funding for the study from Lundbeck Canada Inc. JB, MPL, and MH are employed by Lundbeck Canada Inc. who funded this study. FA reports receiving research support from Eli Lilly, Allergan, Novartis, and TEVA; consulting fees from TEVA, Eli Lilly, Novartis, Lundbeck, ICEBM; and speaker’s honoraria from TEVA, Eli Lilly, Novartis, Allergan, Aralez, and ICEBM.
Data availability
This study is based on data provided by Alberta Health and Alberta Health Services. The interpretation and conclusions are those of the researchers and do not represent the views of the Government of Alberta. Neither the Government of Alberta nor Alberta Health expressed any opinion in relation to this study.










