Megalencephaly–capillary malformation–polymicrogyria (MCAP) syndrome (OMIM #602501) is characterized by megalencephaly, midline capillary malformations, and cortical malformations.Reference Riviere, Mirzaa and O’Roak1,Reference Mirzaa and Adam2 This genetic overgrowth syndrome is associated with mosaic gain-of-function pathogenic PIK3CA variants (OMIM #171834).Reference Riviere, Mirzaa and O’Roak1
A 3-day-old girl had macrocephaly and ventriculomegaly noted on prenatal ultrasounds. She had macrocephaly (42 cm), generalized overgrowth, craniofacial dysmorphic features, and midline facial capillary malformation (Figure 1). Neurological examination revealed axial hypotonia and joint hypermobility. Brain MRI showed megalencephaly, ventriculomegaly, bilateral perisylvian polymicrogyria, and cerebral sinovenous thrombosis (CSVT) involving the torcula and left transverse sinus (Figure 2). Platelets were initially critically low (5 × 109/L) but normalized within 48 h. Initial prothrombin time was elevated (18.7 s, reference range 13.0–15.2) with normal partial thromboplastin time. As the CSVT was initially nonocclusive, and there were no signs of focal neurological consequence of the thrombus (either clinically or radiographically), the initial decision was to not anticoagulate and instead follow closely with repeat imaging.

Figure 1: Craniofacial abnormalities. The patient has frontal bossing and midline facial capillary malformation.
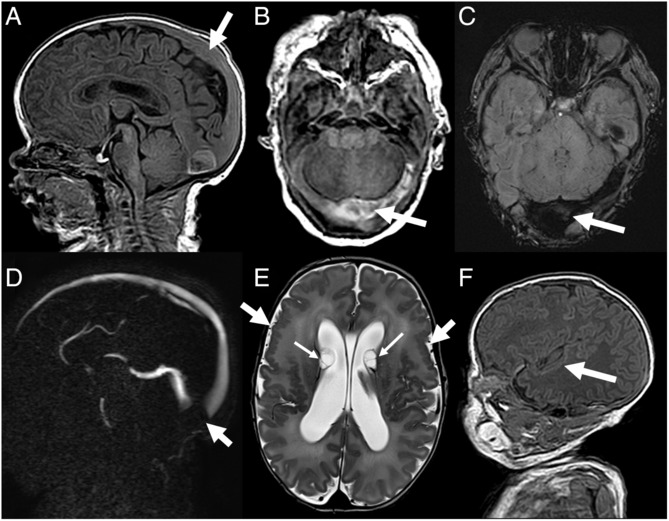
Figure 2: Brain MRI. Sagittal 3D T1 GRE (A) and axial reformations (B) showing enlarged superior sagittal sinus (arrow), with abnormal heterogeneous increased signal intensity in the torcula and left transverse venous sinus, with associated increased magnetic susceptibility on SWI (C). On phase contrast MRV (D), there is a corresponding large “filling defect” (absence of flow related enhancement), consistent with thrombosis (arrow). Axial T2 (E) and sagittal T1 (F) images demonstrate bilateral symmetrical enlargement of the lateral ventricles and extensive bilateral frontal, insular, and peri-insular polymicrogyria (thick arrows). Nonspecific subependymal cysts were also seen bilaterally (thin arrows).
Follow-up MRI 6 days later showed CSVT progression, with thrombosis of right transverse and sigmoid sinuses, torcula, and descending segment of superior sagittal sinus, so enoxaparin was started (discontinued after 7 months). Clinical diagnosis of MCAP was made; genetic testing revealed mosaic (9% of sequencing reads in serum) c.1133 G > A (p. Cys378Tyr) PIK3CA pathogenic variant. On follow-up at age 12 months she had global developmental delay, unable to sit independently and not babbling.
In MCAP, PIK3CA gain-of-function pathogenic variants induce upregulation of the PI3K-AKT-mTOR pathway and subsequent overgrowth. Reference Riviere, Mirzaa and O’Roak1,Reference Mirzaa and Adam2 These sporadic mutations are usually mosaic, giving rise to variable clinical phenotypes depending on the type and localization of the affected tissue. MCAP is part of the PIK3CA-related overgrowth spectrum (PROS), which also includes hemimegalencephaly, congenital lipomatous asymmetric overgrowth of the trunk, lymphatic, capillary, venous, and combined-type vascular malformations, epidermal nevi, skeletal and spinal anomalies (CLOVES) syndrome, and fibroadipose hyperplasia (FH). Reference Mirzaa and Adam2 Although CLOVES and FH have a phenotype that includes patchy segmental overgrowth of limbs, skeletal structures, and lipomatous, lymphatic and vascular tissues, MCAP has a specific neurological phenotype because of the prominent central nervous system (CNS) involvement of the somatic PIK3CA mutations. Reference Mirzaa and Adam2
The core features of MCAP are megalencephaly; craniofacial dysmorphisms, including dolichocephaly and frontal bossing; capillary malformation, including midline facial nevus flammeus or generalized cutis marmorata; and cortical malformations, usually bilateral perisylvian polymicrogyria. Other common features include connective tissue dysplasia (joint laxity, skin hyperelasticity) and distal limb abnormalities (syndactyly, postaxial polydactyly). Reference Mirzaa and Adam2–Reference Mirzaa, Rivière and Dobyns4 In addition to megalencephaly and polymicrogyria, patients often show ventriculomegaly, and cerebellar tonsillar ectopia with posterior fossa crowding; a Chiari I-like malformation may develop. Patients also frequently have hypotonia, global developmental delay, and seizures. They also show variable levels of somatic overgrowth (symmetric or asymmetric).
Individuals with PROS may have increased thrombosis risk; the underlying pathophysiology is unclear, though phlebectasia causing stagnant flow is one possibility, and is observed in CLOVES. Reference Alomari5 Furthermore, MCAP has been associated with CNS venous malformations, aberrant vasculature, and dilated venous sinuses; however, CSVT has only rarely been reported. Reference Mirzaa and Adam2–Reference Mirzaa, Rivière and Dobyns4,Reference Keppler-Noreuil, Lozier and Oden6–Reference Conway, Pressman and Dobyns8 Nevertheless, MRI with venous imaging should be performed for patients with MCAP and acute neurological change. Reference Mirzaa and Adam2,Reference Mirzaa, Rivière and Dobyns4
Disclosures
Dr. Fortin reports no disclosures. Dr. Ashour reports no disclosures. Dr. Lacroix reports no disclosures. Dr. Sabapathy reports being the site PI for a Daiichi and Bayer study, and received a speaker’s stipend from Shire. Dr. Myers reports no disclosures.
Statement of Authorship





