Introduction
“Access to healthcare—particularly in rural areas—goes far beyond proximity of services. Achieving accessibility also necessitates choice, economic and informational resources, and care that is perceived to be effective and appropriate”. Reference Sutherns and Bourgeault1
Canada is a geographically expansive and multicultural country, where rural areas account for more than 90% of the total land mass and are home to nearly one-third of the population.Reference Kulig and Williams2 Higher proportions of Indigenous peoples live in rural and remote areas and are a majority population in the north.Reference Kulig and Williams2 Some advocates have characterized medical care in Canada as a two-tier system, split by rural and urban or by Indigenous and settler populations.Reference Ahmed, Wiebe, Mann and Ohinmaa3,Reference Banerji4 Others have highlighted opportunities; Bell and Menec described rural areas as “a hub for innovation” to “demonstrate innovative models of delivery that can be translated to urban areas later”.Reference Bell and Menec5
Highlight Box: Opportunities for Action
• Ease the burden of travel for neuromodulation follow-up by enabling distributed care models, increasing local competencies in device management, offering resources to offset travel costs, and considering other clinically appropriate treatment options with lower long-term maintenance requirements.
• Increase awareness and advocacy for advanced neurotechnologies and treatment refractory functional conditions within the medical community and the general public.
• Improve health systems efficiencies through the sharing of information across health care networks, referral systems, and jurisdictional changes under the auspices of a national strategy for equitable access to functional neurosurgery.
• Develop cultural competencies within the Canadian neurological sciences community about diverse meanings of brain wellness and disease.Reference Harding, Marra, Manohara and Illes13
For Canadians living with neurologic disorders such as Parkinson’s disease, epilepsy, chronic pain and mental illness, access to advanced healthcare is considered essential and is codified in Canada’s Health Act.6 Modern neurotechnologies that intervene on the brain such as deep brain stimulators (DBS) and magnetic resonance imaging-guided focused ultrasound (MRgFUS) can offer hope, dignity, and the remediation of unbearable symptoms. As functional neurosurgery is only offered in major academic medical centres, geographic, social, political, and economic factors shape access. Honey and colleagues, for example, reported significant variability in DBS implantation rates between provinces based on more than 700 implantations that occurred in Canada between 2015 and 2016.Reference Honey, Malhotra, Tamber, Prud’homme, Mendez and Honey7 They also reported that the median household incomes of communities where people received DBS were significantly higher than the national median household income. They did not identify any access differences between rural and urban communities. There were no implantations in persons from the Territories; however, a finding that they attributed to the short study time frame and a relatively small, young population. Harding and Illes conducted a secondary analysis of the data to compare the expected number of implantations in the urban and rural areas of each province with the national rate and reported a possible access issue in the Atlantic provinces.Reference Harding and Illes8 Crispo and colleagues reported significant regional variation in DBS implantation rates in Ontario.Reference Crispo, Lam and Le9
Recently, two priority areas that have been identified for neuroethical inquiry are “issues of equity, resource allocation, and distributive justice” Reference Rommelfanger and Jeong10 and the cultural meanings of advanced neurotechnologies.Reference Gaudry, Ayaz and Bedows11 To our knowledge, no Canadian study has looked at whether access may differ across the lines of race, ethnicity or culture, or applied qualitative methods to investigate access disparities. This gap is significant because the varying definitions of rural and remote and the size of populations can impact results and conclusions derived from quantitative models.Reference Crispo, Lam and Le9,Reference Weise12
Case Study
Methods
Design
We used a mixed-mode approach to consult with Canadian and international medical experts, identified through their affiliation with two relevant professional organizations, who refer patients to neurosurgery or who use functional neurosurgery to ameliorate the symptoms of neurologic and mental health disorders. We conducted individual semi-structured interviews between January and April 2020 involving a series of open-ended questions focusing on the current level of access to functional neurosurgery as well as barriers, facilitators, and opportunities for access for specific populations including adults and children, people living in rural and remote communities, and people from a range of cultural backgrounds (Box 1). In the preamble to the interviews, we specified that our focus was on access for interventions to the brain. All interviews were audio recorded, transcribed professionally, and made software-ready for analysis using NVivo 12 software (QSR International).
Box 1: Semi-structured interview questions

Box 2: Likert Scale questions (abbreviated)

Participants also responded to 20 Likert-scale questions evaluating the likelihood and imperative (0: none; 4: high) of access to neuromodulation or ablation and resection for individuals living in rural and remote communities in their country of residence for movement disorders, epilepsy, chronic nonmalignant physical pain, and mental illness, and in general (Box 2). Deep brain stimulation (DBS), motor cortex stimulation and responsive neurostimulation, and the technologies used for ablative and resective brain surgeries were in scope for the interview. Noninvasive technologies such as transcranial direct current stimulation (tDCS), transcranial magnetic stimulation and electroconvulsive therapy, spinal and peripheral nerve interventions including vagal nerve stimulation and spinal cord stimulation, infusions, cell and gene therapies, and neurowearables were out of scope.
The research was approved by the University of British Columbia Research Ethics Board (#H19-03196), and consent was obtained from study participants prior to all consultations.
Data Analytic Approach
We applied qualitative content analysis and thematic analysis methods to derive themes from the interviews,Reference Braun and Clarke14,Reference Elo and Kyngäs15 guided by a pragmatic neuroethics interpretive framework.Reference Racine16 Our goal for the analysis was to provide an overall description of this under-researched area.Reference Braun and Clarke14 The process involved bracketing our own presupposed notions on the topic from influencing our analysis,Reference Moustakas17 and then engaging in multiple rounds of iterative category formation using a constant comparison method and a rich coding strategy so that more than one theme could be applied to a single statement.Reference Braun and Clarke14,Reference Glaser and Strauss18 We refined the final set of themes based on prevalence within the dataset, the quality of the supporting data, and each theme’s importance for answering the research question.Reference Braun and Clarke14 Prevalence was calculated as the number of interviewees who articulated each theme. Major thematic categories were defined as the broad organizing themes; minor themes constitute the major themes identified, and subthemes in turn constitute the minor themes.
LH was the primary coder, and a trained research assistant (JM) co-coded 15% of the transcripts to test for interrater reliability.Reference O’Connor and Joffe19 Discrepancies were discussed until there was consensus.
We also used Wilcoxon signed-rank tests to test the a priori hypothesis that the median rating of the likelihood of access to neuromodulation in general for people living in rural and remote areas is lower than for ablation and resection. This hypothesis was based on our prediction that the burden of maintaining the functionality of a reversible neuromodulatory intervention (e.g., programing, battery replacement) that requires travel is greater than the burden of undergoing a more invasive, one-time irreversible ablative or resective procedure.
Results
Demographics
We interviewed 22 experts practicing medicine in Canada and two practicing abroad (n = 24). Twenty-one are subspecialized physicians; three are nurses specializing in neuromodulation (Table 1). All are involved in some stage of care for patients who undergo functional neurosurgery, involving the assessment and referral to surgery through continuing care and follow-up. Seventeen interviewees work only with adults; seven with both adults and children. One interviewee works exclusively with spinal cord stimulation and ablation for pain. Most are involved in research. Only six interviewees had experience in rural areas, of which four had worked rurally. Mean length of the interviews was 27 minutes.
Table 1: Demographics of interviewees (n = 24)

Qualitative Results
A Cohen kappa of 0.9 was achieved in the analysis of transcript coding indicating high intercoder reliability. The content from the interviews fit into seven major thematic categories (Figure 1): 1. Health care system; 2. Neurotechnology features; 3. Patient demographics; 4. Target condition features; 5. Ethics; 6. Upstream barriers and enablers; 7. Areas of opportunity. A pedigree depicting the first six major themes and the minor and subthemes that constitute them are provided in Table 2. The seventh major theme is shown in Table 3.
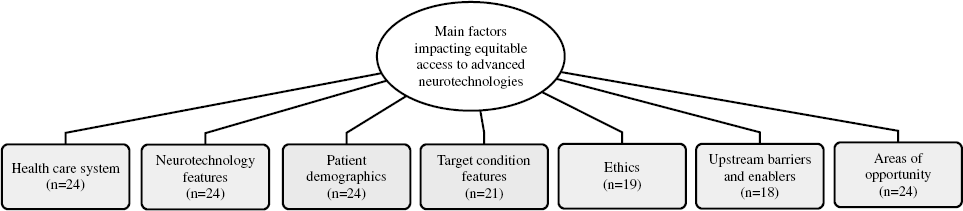
Figure 1: Concept map of the major thematic categories of the qualitative analysis. N represents the number of interviewees who discussed the theme.
Table 2: Pedigree of five major themes and the minor themes and subthemes that constitute them. N represents the number of interviewees who discussed the theme

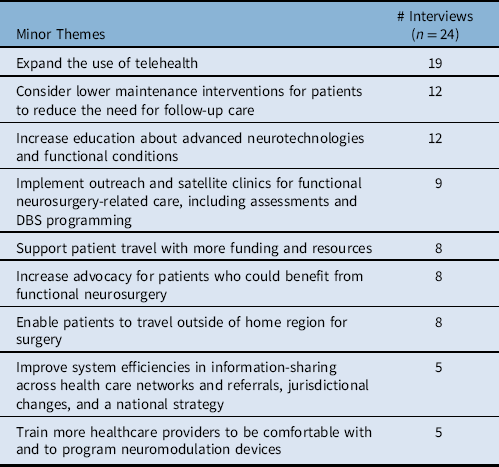
Table 3: Minor themes describing future areas of opportunity for equitable access to advanced neurotechnologies. N represents the number of interviewees who discussed the theme
1. Health care system
In the major thematic category Health care system (n = 24), Resource allocation (n = 23) was the largest minor theme and encompassed comments about how the processes that underlie the allocation of scarce health resources can prevent or enable equitable access (n = 23). The two subthemes were Economics (n = 17) and Politics and policies (n = 12):
“And any time a new government comes in or a new budget comes in, I think these things change.” (Interviewee #11)
The second minor theme was Physically centralized medical system (n = 21), and the third was Collaboration and information sharing among healthcare professionals (n = 6):
2. Neurotechnology features
The theme Neurotechnology features describe how the features of advanced neurotechnologies can impact access. It consisted of nine minor themes and two subthemes (Table 2). Follow-up care requirements were the most prevalent minor theme (n = 23) and focuses on the requirement of Programming neuromodulation devices (n = 18). Most interviewees also spoke about a state of Limited awareness and diverse perceptions among the medical community and public about advanced neurotechnologies (n = 22), which included both a shortage of general knowledge about the interventions and the misconceptions and differing opinions that can exist about them:
“[…] that’s sort of like a natural taboo that someone’s going to stick something into my brain, am I going to be a different person when I wake up? There’s a different fear associated with brain surgery as opposed to peripheral general surgery.” (Interviewee #19)
Many interviewees also described a state of Limited and variable availability of advanced neurotechnologies across the country (n = 21) with extensive Waitlists in many areas (n = 9):
“[I]n general, Canadians are underserved for this, even in urban populations” (Interviewee #01).
The Highly specialized nature of functional neurosurgery (n = 20), the Nature of the evidence about each intervention (n = 19), Effectiveness and benefit (n = 17), the High costs associated (n = 13), Invasiveness (n = 13) and variable levels of Risk (n = 12) were the other minor themes:
“I think only kind of a perception of neurosurgery maybe being a very, very big expensive field where you know, most people wouldn't think about working closely with their local neurosurgeon” (Interviewee #02)
3. Patient demographics
All interviewees spoke about how Patient demographics (n = 24) can shape an individual’s access, especially in the context of Community features (n = 24). Interviewees took into consideration not only the rurality, remoteness, or northernness of a patient’s home community, but also the distance to a centre that offers functional neurosurgery:
“[…] it would be interesting to see if the distance from centre, you know, its effect on number of patients per hundred thousand treated or referred or whatever. Because I'm sure it’s quite profound. Because, you know, the people that we treat tend to be relatively close by. Especially with these mental health interventions.” (Interviewee #03)
Twenty interviewees spoke about Pediatric populations. The two subthemes were: More caution with children (n = 7) and More resources for children (n = 5):
“Because, I mean, governments and societies will sort of bend over backwards to make sure the kids are taken care of,” (Interviewee #10).
Seventeen interviewees spoke about how a patient’s membership in a particular Cultural, ethnic, racial, or religious group may impact their access, and fifteen spoke about Clinical suitability. The minor theme Personal resources (n = 14) split into subthemes about the level of Social and caregiver support (n = 13) and Financial resources (n = 11) available to each patient:
“And so a huge, you know, financial burden for people to take time off work. Or for family to take time off work, caregivers, whatnot, to come here for the programming, which could be every week for a little while – every other week and then monthly for a short time.” (Interviewee #08)
4. Target condition features
The theme Target condition features consists of three minor themes that describe how the Prevalence (n = 17), Functional nature (n = 10), and Severe and treatment refractory nature (n = 6) of the conditions that functional neurosurgery targets contribute to the current picture of access. Statements captured in this theme were frequently related to the management of scarce healthcare resources:
“Because it’s quality of life surgery it seems that it’s a greater battle for us to get funding allocated as opposed to more emergency things, right?” (Interviewee #11)
5. Ethics
The ethics content from the interviews fit into two minor themes: Distributive justice and fairness and Exclusion and bias.
Principles of distributive justice and fairness were expressed by over 50% of the interviewees (n = 13):
“[…] there’s no reason why, as we’re one nation from coast to coast to coast, that anybody should have reduced access to appropriate care because of their location. […] The fact that you are a resident and a citizen of Canada, as such you should be entitled to access as anybody in Vancouver.” (Interviewee #19)
“I mean if there’s a truly effective modality, we should try to advocate for better awareness of them - you know, who would be candidates for them. We shouldn't let them linger with a refractory disease without thinking about other options.” (Interviewee #23)
“I think it’s important to look at this through many different perspectives and to ensure that you know, Canadians have equal access to health care as one of our core tenants.” (Interviewee #28)
The minor theme Exclusion and bias was discussed in nine interviews, primarily in the context of specific cultural, racial, ethnic, or religious groups, or people who live in communities that are rural, remote, or otherwise far away from major health care centres. Within this minor theme, several interviewees spoke specifically about Indigenous populations:
“I do certainly have an Indigenous patient here who […] always asks me every time he comes why there are no studies looking at Indigenous people with Parkinson’s disease.” (Interviewee #08)
“And we have a large Indigenous population […] where I work and I see patients from those communities all the time, even in my practice. But I can probably count on one hand the number of them that have undergone the neuromodulation treatments that I offer. […] I also think that it’s possible, being self-critical of our own program, it’s possible that because one of these things – particularly for implanted devices – we want to make sure is in place is a kind of supportive environment for a patient and a motivated patient that can look after a device and so on. I think it is possible that […] there’s some unconscious bias there and that Indigenous populations are not offered the treatments because there might be the sense that the environment is not suitable for them to be able to look after these devices. […] I’m not sure that there’s anything intentional there specifically, right?” (Interviewee #11)
Another interviewee spoke to the potential impact of living in a remote community:
“[…] just the bias people probably have that if you’re living in a remote area, you’re probably capable of accepting a decreased accessibility to care. In other words: the bias of practitioners that, well you live so far away you’re probably happy with less. […] why else would we be advocating for people who are from remote areas to get better access? […] there is the assumption of relative neglect.” (Interviewee #15)
6. Upstream barriers and enablers
Eighteen interviewees spoke about barriers and enablers encountered in early upstream stages of care that can impact a patient’s chances of gaining access to functional neurosurgery downstream. This includes critical bottlenecks and challenges that impact the likelihood of first receiving a timely diagnosis and appropriate treatment, and then being referred to a functional neurosurgeon for assessment as soon as it may be indicated:
“You have to talk to your family doc who has to talk to the neurologist who has to talk to the neurosurgeon, and because there are multiple steps in order to get in contact with - or on the pathway for deep brain stimulation, it is imaginable that there could be disparities.” (Interviewee #28)
“Getting referred, getting into the system, I think there’s the main barrier.” (Interviewee #20)
7. Areas of opportunity
Nine minor themes comprise the major theme Areas of opportunity (Table 3). Except for two instances, these pertain to health systems and policy changes:
“And whether that’s making telemedicine more widely available, training more specialists, easing the ability of patients to make visits etc., it has to be built into the policies that govern the use of this technology.” (Interviewee #22)
“[…] it would just be nice […] if somebody just realized that maybe this should be a national policy rather than 10 different individual provincial policies.” (Interviewee #10)
The two exceptions suggest that some patients can gain access to functional neurosurgery by seeking care out of their home province or internationally, or by advocating for themselves:
“It’s often patient referral, self-referral, by harassing their doctor to be able to get into some sort of a program like this.” (Interviewee #06)
A subtheme of follow-up care requirements for neuromodulation recurred across several areas of opportunity. Ten out of 12 interviewees who spoke about the opportunity of considering lower maintenance interventions referred to how reducing the need for follow-up visits for programing can improve access for some patients. Thirteen out of 19 interviewees who discussed telehealth indicated the need for technology to program neuromodulation devices remotely. The call to train more healthcare providers to be comfortable with neuromodulation devices included doctors and nurses within both major urban centres and more remote areas:
“It’s not that every centre has to be able to do DBS, but the knowledge of DBS has to be more widespread and more people should be able to at least access the DBS device, to interrogate it.” (Interviewee #25)
Quantitative Results
The number of responses to each Likert-scale question ranged from 18 to 23, and median ratings ranged from 1 to 4. Descriptive statistics suggest that respondents perceive a disparity between the likelihood and imperative of access (Figure 2). Without exception, the median ratings for each imperative question were at least one unit higher than for likelihood. Likelihood and imperative scores were also strongly associated: a higher imperative was generally accompanied by a higher likelihood. The medians for likelihood ranged from 1 to 2, and the medians for imperative ranged from 2 to 4.

Figure 2: Percentage distribution of rating scale responses (Low: 0; High: 4). Imp.: imperative; lik.: likelihood; movement dis.: movement disorders; mental ill.: mental illness; pain: chronic nonmalignant physical pain; general: in general for any clinical indication.
Access to neuromodulation for movement disorders ranked the highest, and for mental illness the lowest overall. Participants were unified in their low rankings of the likelihood of access to functional neurosurgery for mental illness but were considerably divided on the question of imperative. Questions about the imperative of access for mental illness received more responses at the extreme ends of the rating scale than for any other application.
The Wilcoxon signed rank tests did not reveal a statistically significant difference between the median rating of the likelihood of access to neuromodulation as compared to ablation and resection in general for people living in rural and remote communities (p = .34).
Synthesis of Qualitative and Quantitative Results
Taken together, the results suggest that exceptional barriers exist to accessing neuromodulation for people living in rural and remote areas:
“So, is living in a rural area of Canada a contraindication to having a gizmo? No. But it certainly makes the logistics a bit more complicated given the complexity of care.” (Interviewee #01)
Looking at the specific medical conditions, low ratings for access to neurosurgical interventions for pain may relate to a larger issue of how chronic pain is treated:
“The major barrier is that the treatment of chronic pain is a big black hole in our medical system. It’s not done that well in general.” (Interviewee #16)
Similarly, the low ratings for the likelihood and imperative of access to neurosurgery for mental illness related to remarks about the continuing impacts of the negative history of psychosurgery:
“And so I think that it’s important to be mindful of the historical legacy of unbridled enthusiasm on the part of researchers and clinicians for trying certain things without regulations. And we also need to be mindful of making sure that any intervention we try is hypothesis-driven, is done judiciously, and done in a regulated fashion and is done in a way that has a lot of evidence behind it.” (Interviewee #22)
Opportunities
Discussion
In this case study of expert perceptions of functional neurosurgery for rural, remote, and ethnically diverse communities in Canada, seven major themes emerged: Health care system, Neurotechnology features, Patient demographics, Target condition features, Ethics, Upstream barriers and enablers, and Areas of opportunity. Neuromodulation emerged in both parts of this mixed-methods project as carrying unique considerations and potential challenges.
Neurologic disorders such as Parkinson’s disease and epilepsy are perceived to have a higher likelihood of being successfully treated with functional neurosurgery for people living in rural and remote areas than disorders involving physical pain and mental health. While the cohort of medical professionals had little direct experience with rural and remote communities, per se, they were able to identify a range of factors that can impact equitable access based on their clinical and research experience.
The interviewees shared a number of ideas about how to improve equitable access for diverse populations. These included possibilities for more distributed care models than are currently available, funding for patient travel, lower maintenance interventions to reduce the burden of travel for follow-up care, increasing awareness and advocacy for advanced neurotechnologies, improving the efficiency of health care systems and, for patients who can afford it, traveling outside of their home region for the surgery. A recurring focus across many areas of opportunity was the need to ease the burden on patients of traveling for frequent neuromodulation device programing appointments.
The findings of this study add to the body of research that has assessed the state of health care access for rural and remote populations in Canada living with movement disorders, epilepsy, chronic pain, and mental illness (e.g., Reference Friesen20–Reference Rice and Webster23). Statements about cultural, ethnic, and racial disparities add to what is known about the historical and ongoing injustices that Indigenous peoples face in the Canadian health care system and the need for culturally safe care,Reference Cameron, Carmargo Plazas, Salas, Bourque Bearskin and Hungler24,Reference Holt, Hansen, McKinney and Mendez25 and relate to evidence from other countries such as the United States from which racial disparities to DBS and epilepsy surgery have been reported.Reference Burneo, Black, Knowlton, Faught, Morawetz and Kuzniecky26–Reference Willis, Schootman, Kung, Wang, Perlmutter and Racette32
Limitations
Twenty of the experts had little to no direct experience working in rural and remote communities. Their views are expert but can be taken as hypothetical and anticipatory only. We could not disclose information on the countries of the two international interviewees for reasons of confidentiality. While the sample size provided a sufficient range of interviewee demographics for a rich qualitative analysis,Reference Sandelowski33 it may not have been sufficiently powered for statistical testing of the Likert-scale questions. Additionally, diversity in the years of experience and countries of practice of the interviewees may have been sources of uncontrolled variability in the data. Finally, the interviews were prior to the COVID-19 pandemic. Recent advancements in remote health care delivery models that were developed in response to the health crisis were not captured (e.g., Reference Fasano, Antonini and Katzenschlager34–Reference Sharma, Safarpour and Mehta36).
Conclusion
Differences in health care access between rural and urban populations or ethnic groups are unacceptable and unethical. This mixed mode study of interviews with medical experts depicts a complex picture of access to functional neurosurgery in Canada with pockets of excellence and a motivation to improve the availability of care for all populations.
A coordinated Canadian strategy is needed to ensure that clinical innovations improve health for all populations, and close rather than widen gaps. Beyond the opportunities identified in the present study, the development of cultural competencies within the Canadian neurological sciences community about diverse meanings of brain wellness and disease can support this movement.Reference Harding, Marra, Manohara and Illes13 Bi-directional approaches that directly engage patient communities are essential in this process given the evidence showing differences between how clinicians and patients perceive the risks, benefits, and invasiveness of the procedures,Reference Cabrera, Courchesne and Bittlinger37,Reference Das, Matias and Ramesh38 as well as the enabling effects of patient education highlighted in the present study. Taken together, positive actions drawn from medical, legal, and ethical initiatives can improve care for culturally diverse patients living with severe, treatment refractory conditions, address historic distrust, achieve government support for equalizing access, and realize an ethically grounded future for advanced neuromodulatory and ablative technologies.
Acknowledgements
We thank participants for generously sharing their time with us, reviewers for their helpful suggestions, and members of Neuroethics Canada for providing their input and assistance at various stages of the research. Neuroethics Canada is located on the traditional, ancestral, unceded territory of the xʷməθkʷəỳəm (Musqueam people).
Author contributions
The study was conceptualized by JI and LH. The interview questions were developed by JI and LH in collaboration with PJM and CRH. Interviews were conducted and analyzed by LH. LH and JI drafted the manuscript. JM conducted the quantitative data analysis, co-coded the transcripts, and contributed to respective sections of the paper. CRH and PJM made critical revisions throughout the writing process.
Funding
This work was generously supported by the North Growth Foundation (JI), National Institute of Mental Health (JI; RF1#MH117805 01), a Canadian Institutes of Health Research Canada Graduate Scholarship Master’s Award (LH; #6556), and a W. Maurice Young Centre for Applied Ethics Graduate Fellowship (LH). JI is a University of British Columbia Distinguished University Scholar and Distinguished Scholar in Neuroethics.
Conflicts of interest
LH and JM have no conflicts of interest to declare. CRH has received a grant from the National Spasmodic Dysphonia Society and lecture fees from Boston Scientific and Medtronic. PJM has received a grant from NIH, is a Chair on the Ethics Committee of the Royal College of Physicians and Surgeons of Canada and is a past President of the Canadian Neurosurgical Society. JI offers lectures on the topic of research with Indigenous populations, is the Vice Chair of the CIHR INMHA IAB, a member of the AAN Ethics, Law, and Humanities Committee, and Chair of the International Brain Initiative.









