A 28-year-old female presented with a 2-week history of new onset horizontal binocular diplopia. She had a history of relapsing-remitting multiple sclerosis (MS) for 2 years that was treated with glatiramer acetate. The diplopia was worse in left gaze and was associated with right eye pain that was worse with eye movements. On examination, corrected distance visual acuity was 20/20 in both eyes and her pupils were symmetric without a relative afferent pupillary defect. External examination revealed 3 mm of proptosis of the right eye and nasal conjunctival injection without lid lag or eyelid retraction (Figure 1A). Ocular motility testing revealed a complete limitation of adduction in the right eye without nystagmus in either eye (Figure 1A). The combination of ocular pain, conjunctival injection, proptosis, and limitation of adduction localized the process to the right orbit. Specifically, a medial orbital mass causing restriction of eye movements was suspected and magnetic resonance imaging (MRI) of orbits with gadolinium was performed. This revealed marked enlargement and enhancement of the right medial rectus muscle with relative sparing of the tendon (Figure 1B). There was also mild subclinical enlargement of the left medial rectus muscle. Extensive bloodwork that included thyroid function tests, vasculitic and infectious investigations were negative and she was diagnosed with nonspecific orbital inflammation (NSOI) involving the extraocular muscles (i.e. orbital myositis). She was started on prednisone 1 mg/kg and her symptoms improved but recurred with taper after 2 months. This prompted a biopsy of the medial rectus muscle that showed signs of NSOI and her symptoms resolved with further steroid treatment at 6 months.
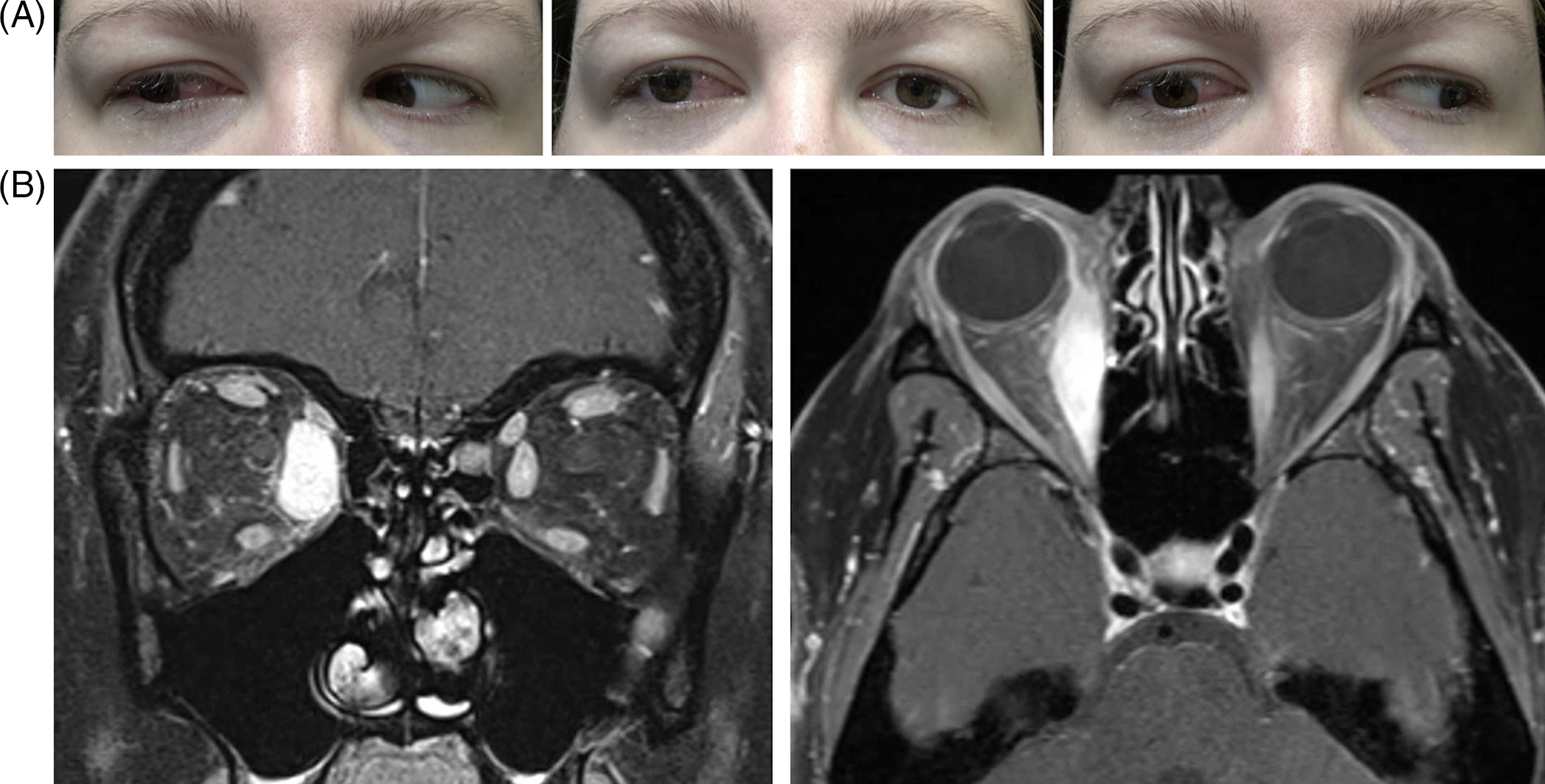
Figure 1: (A) Ocular ductions revealing a limitation of adduction in the right eye and. (B) Coronal and axial MRI T1 post-contrast demonstrating a very enlarged right medical rectus muscle.
The most common cause of adduction limitation in patients with multiple sclerosis is internuclear ophthalmoplegia (INO) and this case highlights the importance of having a broad differential diagnosis when assessing new diplopia in MS patients. This patient had orbital signs (e.g. proptosis, conjunctival injection and pain), indicating that an MRI of the orbits was the best imaging modality rather than an MRI of the brain with careful attention to the brainstem, which might miss the orbital findings. NSOI is considered a diagnosis of exclusion as other causes of orbital inflammation should be considered, such as thyroid eye disease, inflammatory (e.g. sarcoidosis), vascular (e.g. carotid cavernous fistula) and neoplastic (e.g. lymphoma) disorders. Although there is no established relationship between MS and NSOI, the presence of one autoimmune disease does confer increased risk for others. Our review of the literature retrieved only one previous published case of recurrent orbital inflammation involving the lacrimal glands in a patient with MS treated with interferon-beta.Reference Spierer and Leibovitch 1 When NSOI involves the extraocular muscles, the medial rectus is most commonly involved followed by the superior, lateral and inferior recti.Reference Eshraghi, Sonbolestan, Abtahi and Mirmohammadsadeghi 2 As seen in our patient, there is typically a prompt response to steroids in acute cases and a slow taper may avoid the need for steroid-sparing agents. This case reminds us that we should avoid automatically attributing new neurological symptoms to multiple sclerosis in MS patients to minimize misdiagnosis and improve patients’ outcome.
Statement of Authorship
MB: Manuscript write-up, manuscript revisions.
MMP: Manuscript write-up, manuscript revisions.
CDK: Critical revision, final approval.
RV: Critical revision, final approval.
NN: Critical revision, final approval.
JAM: Data acquisition, critical revision, final approval.
Conflicts of Interest
The authors have no relevant financial conflicts of interest to disclose.



