A 53-year-old female developed acute onset dysarthria, right-sided tongue deviation, and neck pain without sensory or taste alteration 2 h after a session of chiropractic neck manipulations. Her past medical history included gastroesophageal reflux disease. Initial computed tomography of the head and neck with angiogram did not demonstrate any intracranial abnormality or signs of carotid or vertebral artery dissection. There was no fracture, dislocation, or subluxation demonstrated (Figure 1A). She was referred to the urgent neurology clinic 3 weeks later and neurological examination demonstrated dysarthria, right-sided tongue deviation, and atrophy (Figure 1B). The rest of the neurological examination was within normal limits, including normal palate and uvula elevation and intact brainstem reflexes. Magnetic resonance imaging (MRI) of the head and cervical spine with angiogram, T1 fat suppression and Fast Imaging Employing Steady-state Acquisition sequence 3 weeks after onset of symptoms did not demonstrate any dissection, thrombosis, vascular compression, upper cervical spine fracture, dislocation, subluxation, or edema. No definite abnormality of the right hypoglossal nerve (HN) was identified intracranially. Her symptoms completely resolved in 4 weeks without intervention. Follow-up MRI of the head 5 months later was unremarkable with no abnormality seen in relation to the intracranial course of the right HN (Figure 1C).
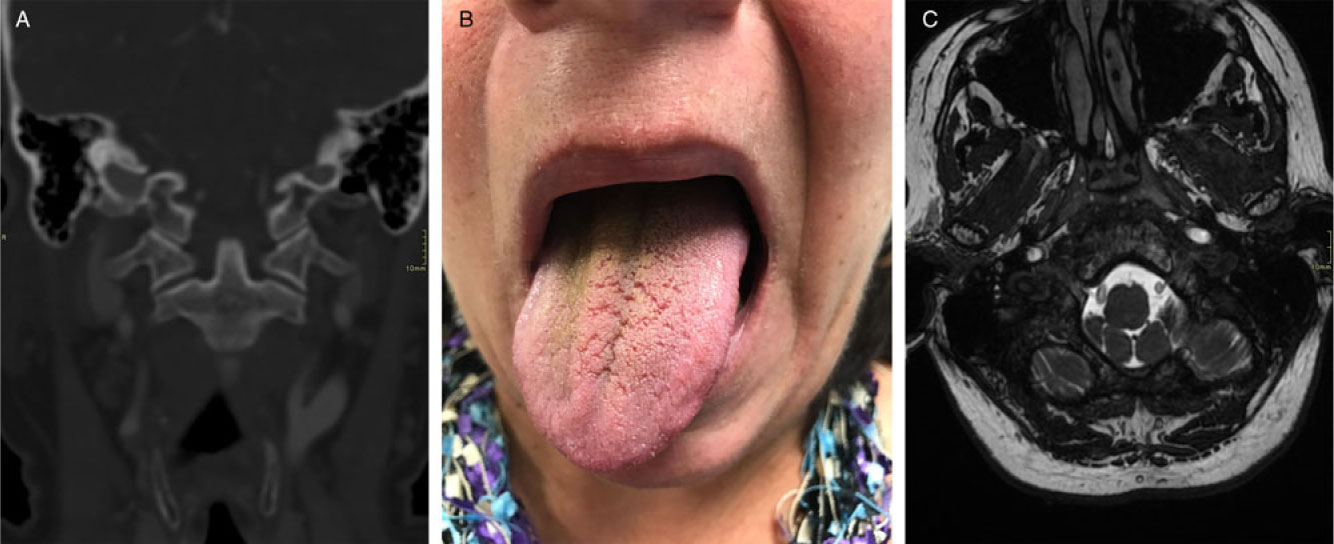
Figure 1: (A) Computed tomography (CT) of the head (Coronal view, bone window). No fracture, dislocation, subluxation and misalignment were demonstrated at the level of the occipital condyle, atlas and axis on CT imaging of the head 2 days after onset of symptoms. (B) Photograph of patient. During a physical examination 3 weeks after chiropractic manipulation, protrusion of the tongue revealed right-sided deviation and atrophy suggestive of ipsilateral right hypoglossal nerve injury. (C) Magnetic resonance imaging (MRI) of the head (FIESTA sequence). No abnormality was seen in relation to the intracranial course of the right hypoglossal nerve on MRI of the head performed 5 months after onset of symptoms.
This patient developed symptoms and signs consistent with a right HN injury following chiropractic maneuvers of the neck. The HN exits the base of the skull through the hypoglossal canal and descends in the neck between the sternocleidomastoid and internal carotid artery, lateral to the vagus nerve, to reach the stylopharyngeal, styloglossus, and stylohyoid muscles.Reference Iaconetta, Solari and Villa1,Reference Lin and Barkhaus2 The HN is joined by the C1 nerve fibers which branch off to innervate the geniohyoid and thyrohyoid muscles, also supplying descending nerve fibers to the infrahyoid muscles.Reference Lin and Barkhaus2 These descending fibers receive contribution from C2 and C3 nerve fibers as well, which is known as the ansa cervicalis.Reference Lin and Barkhaus2
Tongue weakness following trauma has been well described in the context of hematoma,Reference Vito, Wanamaker and Shields3 localized swelling,Reference Harrison and Hilmi4 internal carotid artery dissection,Reference Hennings, Hoehn, Schumann-Spaeth and Weber5 and cervical fracture (occipital condyle),Reference Yoon, Lim, Park and Lee6 but these structural findings were not relevant in our patient. Our patient’s symptoms were transient and fully recovered without evidence of structural abnormalities on imaging. The mechanism of injury was likely secondary to sudden high-velocity movements of the neck, causing traction or compression injury (neurapraxia) of the proximal HN near the skull base and occipital condyle causing ipsilateral tongue deviation. This localization is in keeping with other cases of HN palsy after high-velocity neck trauma involving the HN at the level of the occipital condyle.Reference Yoon, Lim, Park and Lee6 Transient facet joint subluxation affecting nerve root fibers innervating the ansa cervicalis is not likely due to an absence of clear cervical root symptoms. A localization proximal to or within the hypoglossal canal is unlikely to be affected by high-velocity neck movements. Normal imaging studies do not rule out a HN injury, as HN beyond the hypoglossal canal cannot be readily visualized with standard imaging techniques. This case also highlights the clinical importance of eliciting a history of recent trauma related to the neck in patients with otherwise unexplained HN dysfunction, despite all available imaging studies being normal.
This is the first report in the medical literature presenting with tongue weakness following chiropractic treatment and represents a new potential rare neurological complication of the maneuver. Serious but rare neurological complications following chiropractic manipulation have been well described and may include cervical or vertebral artery dissection, stroke, myelopathy, and radiculopathy.Reference Stevinson, Honan, Cooke and Ernst7 Furthermore, vigilant reporting of various potential complications of chiropractic neck manipulations is required to improve awareness among medical practitioners and patients about the potential safety and risks of this common therapeutic procedure.
Acknowledgments
We acknowledge the patient for allowing us to publish her case.
Disclosures
Dr. TLHC, Dr. DDK, Dr. MS and Dr. MJ have no disclosures to report. “Patient Consent for Publication” form was obtained from the patient.
Statement of authorship
Dr. TLHC and Dr. MJ examined the patient. All authors wrote the manuscript and created the figures.



