Hockey is one of the most popular sports played by Canadian youth. During the 2015-2016 season, over 500,000 athletes were registered in organized hockey across Canada. 1 Among the most common injuries sustained in competitive youth hockey is concussion,Reference Emery and Meeuwisse 2 - Reference Houghton and Emery 4 a form of traumatic brain injury (TBI) that results in clinical symptoms that typically resolve within 1-4 weeks.Reference Davis, Anderson and Babl 5 , Reference Williams, Puetz, Giza and Broglio 6 Studies suggest that optimizing the clinical care of pediatric concussion patients requires early injury recognition and multi-disciplinary management by a team of healthcare professionals with expertise in traumatic brain and spine injury.Reference Ellis, Ritchie and McDonald 7 , Reference Makdissi, Cantu, Johnston, McCrory and Meeuwisse 8
To help improve the health and safety of its athletes, several professional sport leagues have established standardized concussion protocols that outline measures that must be taken to ensure proper recognition, medical evaluation, and clearance of those who sustain a suspected concussion.Reference Cochrane, Owen, Ackerson, Hale and Gould 9 More recently, Canadian government, sport, and health stakeholders have recommended that organizations operating youth sport activities with a risk of concussion also establish similar standardized concussion protocols for their athletes.Reference Fremont, Bradley, Tator, Skinner and Fischer 10 , 11 Despite these advances and recommendations, the authors are not aware of any published reports evaluating the feasibility and implementation of a standardized medically supervised concussion protocol for any youth sport in Canada.
Accordingly, we present a single-season (2016-2017) review of injury surveillance, as well as clinical and healthcare utilization data, for all athletes evaluated through a standardized concussion protocol established between a city-wide AAA hockey organization and a provincial multi-disciplinary pediatric concussion program. We also present the results of post-season surveys from coach and parent stakeholders who were responsible for athletes competing during the same season. Drawing from this experience and recently published national guidelines, we highlight several key elements that should be considered by sport stakeholders when developing standardized concussion protocols for youth sports in Canada.
Methods
Standardized Concussion Protocol and Participants
Beginning in the 2013-2014 season, Winnipeg AAA Hockey and the Pan Am Concussion Program established a standardized medically supervised concussion protocol for all athletes. Winnipeg AAA Hockey is the governing body responsible for the organization and operation of a youth minor hockey league that typically includes 250-280 male Bantam (age 12-14 years) and Midget (age 15-17 years) athletes playing full contact hockey at the highest competitive level in Winnipeg, Manitoba, Canada. The Pan Am Concussion Program is a provincial government-funded clinical program that provides multi-disciplinary evaluation and management of children and adolescents with concussion and other forms of TBI throughout Manitoba. Outside of the Winnipeg AAA Hockey concussion protocol, patient access to the pediatric concussion program requires a referral from a physician. However, patients who sustained repeat injuries after discharge from the pediatric concussion program can be seen without a physician referral. All patients referred to this pediatric concussion program undergo medical assessment and Return-to-Sport medical clearance by a single neurosurgeon who has access to a multi-disciplinary team of experts in neuropsychology, vestibular and cervical spine physiotherapy, exercise science, and other sub-disciplines, as well as off-site diagnostic imaging (i.e., radiography, magnetic resonance imaging, MRI).Reference Ellis, Ritchie and McDonald 7
The primary objective of the Winnipeg AAA Hockey concussion protocol was to provide clear instructions to athletes, parents, and coaches regarding measures that must be taken to ensure standardized medical evaluation, follow-up, and clearance of all Winnipeg AAA Hockey athletes who sustained a suspected concussion or more serious head or neck injury during a game or practice. On the basis of feedback from sport and medical stakeholders obtained over the first 3 years of implementation, the original concussion protocol underwent several minor revisions. In summary, the 2016-2017 Winnipeg AAA Hockey concussion protocol specified that all athletes with a suspected serious head or spine injury undergo on-ice evaluation by emergency medical services and referral to Winnipeg’s Health Sciences Children’s Hospital (HSC-CH). All athletes who sustained a suspected concussion resulting in non-life-threatening acute symptoms were to be immediately removed from play and evaluated at HSC-CH or the nearest hospital. After initial emergency department assessment, these patients were instructed to seek follow-up care at the Pan Am Concussion Program. Athletes who developed delayed concussion symptoms following an injury could receive direct access to the Pan Am Concussion Program. In the case of athletes who sustained a suspected concussion and had on-site access to a medical doctor (MD) or athletic therapist, sideline assessment was to be carried out using the Sport Concussion Assessment Tool 3 (SCAT3) to document initial neurological status. However, because SCAT3 testing can be normal in adolescents with an acute concussion,Reference McCrory, Meeuwisse and Aubry 12 all athletes with a suspected concussion were to be referred for medical assessment irrespective of the SCAT3 results. For each athlete removed from play for a suspected concussion or more serious head or spine injury, the athlete’s parent, coach, or trainer was instructed to contact the designated Winnipeg AAA Hockey Concussion Protocol Coordinator who was responsible for injury surveillance and facilitating referrals for initial assessment and follow-up care at the Pan Am Concussion Program. In cases in which the pediatric concussion program was notified directly of an injured Winnipeg AAA Hockey player, the athlete’s parents were advised to report the injury to the Winnipeg AAA Hockey Concussion Protocol Coordinator before the athlete being scheduled for clinical assessment. Before returning to full contact and/or game play, all athletes were required to obtain medical clearance by a single neurosurgeon and were not to be allowed to return to play without a written medical clearance letter issued by the pediatric concussion program.
To ensure that all parents and coaches were informed of the standardized concussion protocol, a parent for each athlete was required to attend a pre-season orientation session held by Winnipeg AAA Hockey. The standardized concussion protocol was provided to each head coach before the start of the season and the protocol was posted online on both the Winnipeg AAA Hockey and Pan Am Concussion Program websites. Last, all head coaches were required to attend a pre-season coaches meeting that included a presentation on concussion and the concussion protocol.
Clinical Assessment and Definitions
Athletes referred to the Pan Am Concussion Program through the concussion protocol underwent clinical assessment by a single neurosurgeon. All athletes completed the Post-Concussion Symptom Scale (PCSS), which is a valid and reliable measure of concussion symptoms,Reference Kontos, Elbin and Schatz 13 , Reference Lovell, Iverson and Collins 14 at all clinical appointments. The diagnosis of concussion was made by the neurosurgeon based on the definition set forth by the International Consensus Statement on Concussion in Sport.Reference McCrory, Meeuwisse and Aubry 12 Diagnostic imaging and referrals to other multi-disciplinary team members were arranged based on the clinical discretion of the neurosurgeon. In general, patients were deemed clinically recovered when they were asymptomatic at rest, were tolerating full-time school without symptoms, had a normal neurological examination, and had successfully completed the graduated Return-to-Sport protocol set forth by the 4th International Consensus Statement on Concussion in Sport.Reference McCrory, Meeuwisse and Aubry 12 In select cases, assessment of clinical recovery was supplemented by the use of graded aerobic treadmill testing at the discretion of the treating neurosurgeon.Reference Cordingley, Girardin and Reimer 15 Written medical clearance was provided by the neurosurgeon to athletes before a return to full contact and/or full game play.
In some cases, athletes were referred through the concussion protocol for precautionary reasons (a high-velocity body-check that resulted in no symptoms, development of non-specific symptoms unrelated to any head injury) where a definitive diagnosis of concussion could not be made based on the results of the clinical history, physical examination, and other tests (i.e., graded aerobic treadmill testing). These patients were managed on an individualized basis and also received medical clearance before returning to full contact practice and/or game play.
Injury Surveillance
During the 2016-2017 season, the Winnipeg AAA Hockey Concussion Protocol Coordinator maintained a list of athletes who reported concussions and were managed through the concussion protocol during the 2016-2017 season. At the end of the season, injury surveillance data from the Concussion Protocol Coordinator was cross-referenced with medical records at the Pan Am Concussion Program to confirm that athletes who reported their injuries were indeed evaluated and received final medical clearance to return to full contact practices and/or game play. In addition, a medical records search of all Winnipeg AAA Hockey players evaluated during the 2016-2017 season was also conducted to determine whether any players were evaluated at the Pan Am Concussion Program but did not report their injury to the Winnipeg AAA Hockey Concussion Protocol Coordinator.
Coach and Parent Surveys
Electronic surveys were sent to available email addresses obtained from Winnipeg AAA Hockey for all 14 head coaches and one parent of 233 of the 272 players who participated in the 2016-2017 season. The purpose of these surveys was to assess compliance with the standardized concussion protocol during the 2016-2017 season, to obtain coach and parent feedback on awareness and communication related to the concussion protocol, and to obtain their general perspective on concussion protocols and awareness. Electronic surveys were emailed to coaches and parents monthly over a 4-month period.
Statistical Analysis and Ethical Approval
The characteristics of the athletes were presented as means with standard deviations (or medians with intraquartile ranges if data were not normally distributed) or percentages. The results from the surveys were tabulated. All statistical analyses were conducted using the STATA v13.0 statistics package. Institutional ethics approval was obtained from the University of Manitoba for this study.
Results
Clinical Data
During the 2016-2017 season, 28 athletes were evaluated through the medically supervised concussion protocol, with two athletes undergoing evaluation for repeat injuries (a total of 30 suspected injuries and consultations). During the season, 29/30 (96.7%) injuries were reported to the Winnipeg AAA Hockey Concussion Protocol Coordinator. The one injury not reported directly to the coordinator occurred in a patient who sustained a repeat injury during the same season. Of those who were managed through the standardized concussion protocol, the mean age was 14.42 years (ranging from 12 to 17 years) including 15 male Bantam and 13 male Midget athletes. Among the 28 athletes who were evaluated through the protocol, 12 (42.9%) had a history of previous concussion. In this cohort, 29 of the 30 suspected injuries occurred during hockey-related activities, including 22 that occurred during game play, three that occurred during practice, and four that occurred during an unspecified hockey-related activity. One athlete sustained a non-sports-related injury secondary to a fall down the stairs. Six patients underwent evaluation in the emergency department before initial assessment at the pediatric concussion program. The mean number of days from injury to clinical assessment at the pediatric concussion program for all injuries was 2.33 days (SD: 1.5). On the basis of clinical assessment by the neurosurgeon, a definitive diagnosis of concussion was made in 23/30 (76.7%) consultations, including two athletes who sustained two concussions in the same season. The median initial PCSS score among athletes diagnosed with a concussion at the time of initial assessment was 10 (intraquartile range 1-15). At the time of assessment, five athletes diagnosed with concussion were also diagnosed with co-incident whiplash-type cervical spine injuries and one was diagnosed with post-traumatic benign paroxysmal positional vertigo. Diagnostic imaging resources utilized by this cohort included routine cervical spine radiographs (three patients), and CT, MRI, and flexion-extension radiographs of the cervical spine (one patient). Multi-disciplinary consultations that were arranged to help assist with management of these 30 injuries included referral to an exercise physiologist for graded aerobic treadmill testing (11 patients); referral to a vestibular physiotherapist (one patient); referral to a cervical spine physiotherapist (two patients); and consultation with a musculoskeletal radiologist (one patient). Among the athletes who were initially evaluated through the standardized concussion protocol, 27/28 (96.4%) were medically cleared to return to play during the same season. The mean number of days from initial injury to final medical clearance among athletes with a diagnosed definitive concussion was 12.71 days (SD: 5.71). Among the two athletes who sustained repeat concussions during the season, one athlete sustained a repeat concussion ~1 month after the initial injury. Clinical recovery in this athlete was documented at 28 days post injury, and return to play was not considered because the athlete’s season had ended. The other athlete sustained a repeat concussion ~2.5 months after the initial injury. Clinical recovery in this athlete was documented 11 days post injury; however, the athlete was advised to take the rest of the season off owing to the potential risk of repeat injury.
One patient underwent initial assessment for a suspected concussion at an emergency department and was discharged home without medical follow-up after undergoing routine radiographs and CT imaging of the cervical spine. The patient was evaluated through the concussion protocol the following day where the patient was found to have isolated neck pain, no other concussion-like symptoms, and a normal neurological examination. The previously obtained diagnostic imaging studies were reviewed by the neurosurgeon and a musculoskeletal radiologist and an urgent MRI and flexion-extension radiographs of the cervical spine were arranged that confirmed the presence of a previously unrecognized T1 vertebral body compression fracture. The patient was withheld from hockey for the remainder of the season and managed conservatively.
Discussion
This study provides preliminary evidence that adopting and implementing a medically supervised league-wide concussion protocol for youth hockey in Canada is feasible but highlights a number of key factors that must be considered by sport stakeholders when developing these protocols.
First, compliance with standardized concussion protocols is critically dependent on optimizing pre-season education and awareness across all sport stakeholders, as well as ensuring clear communication between medical and sport stakeholders in instances in which athletes are managed through the concussion protocol. Although we found mixed reviews regarding the quality of communication coaches and parents felt they had received from the league about the concussion protocol, the results of our surveys suggest that the vast majority of responding coaches (90%) and parents (91%) were well aware that there was a standardized concussion protocol in place for the 2016-2017 season. This level of awareness among sport stakeholders was associated with 96.7% of athletes managed through the concussion protocol being captured by the Concussion Protocol Coordinator and 100% of eligible athletes undergoing complete medical follow-up and clearance to return to full hockey activities. However, despite dedicated clinical pathways to expedite post-injury concussion care and league investment in a designated Concussion Protocol Coordinator, the results of coach and parent surveys suggest that there were indeed athletes who sustained suspected concussions during the season that were not reported to the concussion protocol coordinator and thus not managed through the concussion protocol. Taken together, the results of this study suggest that medically supervised concussion protocols can be established for youth hockey; however, compliance is difficult to assess and is dependent on sport stakeholder awareness and education, as well as reliable injury recognition and reporting.
Second, the results of this study underscore the importance that all athletes with a suspected concussion undergo medical assessment and medical clearance by a physician. Expert consensus guidelines, as well as standardized concussion protocols in professional sports leagues, consistently recommend that all athletes removed from play with a suspected concussion undergo urgent medical assessment by a physician.Reference Cochrane, Owen, Ackerson, Hale and Gould 9 , 11 , Reference McCrory, Meeuwisse and Aubry 12 , 16 , Reference McCrory, Meeuwisse and Dvorak 17 To provide comprehensive medical assessment and clearance of athletes with a suspected concussion, a trained clinician must exclude more severe forms of TBI, cervical spine injuries and other medical and neurological disorders and must do so based on features of the clinical history, physical examination findings and the use of diagnostic imaging as needed.Reference Ellis, Ritchie and McDonald 7 In the majority of Canada, only MDs and nurse practitioners are licensed to perform medical assessments, order diagnostic imaging studies, and initiate referrals to other sub-specialty physicians. A review of clinical and healthcare utilization obtained from this study revealed that most patients who entered the standardized concussion protocol were managed successfully with proper education and supervised progression through their Return-to-Sport strategy. However, a number of patients benefitted from timely access to diagnostic imaging and multi-disciplinary consultation with other healthcare professionals with licensed expertise in vestibular and cervical spine physiotherapy and exercise science. Importantly, follow-up medical assessment in one patient resulted in timely neuroimaging and diagnosis of a previously unrecognized thoracic spine fracture. This important element of the concussion protocol was supported by our survey results where 100% of coaches and 85.4% of parents indicated that all athletes with a suspected concussion should be evaluated by a MD. Taken together, we recommend that all established standardized concussion protocols, especially those implemented in high-risk sports such as hockey, require that all athletes with a suspected concussion undergo medical assessment and clearance by a physician (or nurse practitioner)—ideally by one with clinical training and experience in traumatic brain and spine injuries.
Third, the results of this study support previous recommendations from the Canadian Concussion Collaborative that all concussion protocols should undergo a process of periodic review and evaluation.Reference Fremont, Bradley, Tator, Skinner and Fischer 10 In addition to providing sport stakeholders the opportunity to assess protocol compliance, feedback from coaches and parents can also help identify areas of the concussion protocol that can be improved. Two aspects of the present concussion protocol that were identified as needing improvement were athlete education and communication between medical professionals and coaches. Although proper identification of athletes with a suspected concussion is highly dependent on athletes recognizing and reporting concussion symptoms, historically pre-season sport stakeholder concussion education had not been included as a mandatory component of the concussion protocol. Although survey data indicated that 70% of coaches and 45.5% of parents felt that the athletes received enough education on concussion, there was inconsistent support for mandating annual concussion education for all athletes, parents, and coaches. Survey data also suggested that although head coaches received written documentation indicating when an athlete was medically cleared to return to games, communication regarding what activities the athletes were cleared to participate in during the Return-to-Sport process could be improved.
Although the results of this evaluation and review process helped guide future revisions to the Winnipeg AAA Hockey concussion protocol, this process also benefitted from recent work completed on the Concussion Protocol Harmonization Project, a federal government initiative to develop a national guideline on concussion education, prevention, and management in Canada, as well as sports-specific concussion protocols for several national sports. 18 Released in July 2017, the Canadian Guideline on Concussion in Sport outlines a standardized clinical pathway to help guide the development of sport-specific concussion protocols including measures to optimize pre-season sport stakeholder education, injury recognition, and medical assessment and clearance (see Figure 1). 11 Therefore, to address some of the limitations of the concussion protocol identified in this study and incorporate recommendations from the Canadian Guideline on Concussion in Sport, the 2017-2018 Winnipeg AAA Hockey concussion protocol underwent significant revision including adding a requirement that all athletes, parents, and head coaches complete a standardized pre-season concussion education sheet 11 (see Supplementary Material). The revised protocol also incorporated the use of the Medical Assessment and Medical Clearance Letters included in the guideline to help improve communication between medical professionals and athletes, parents, coaches, and league organizers.
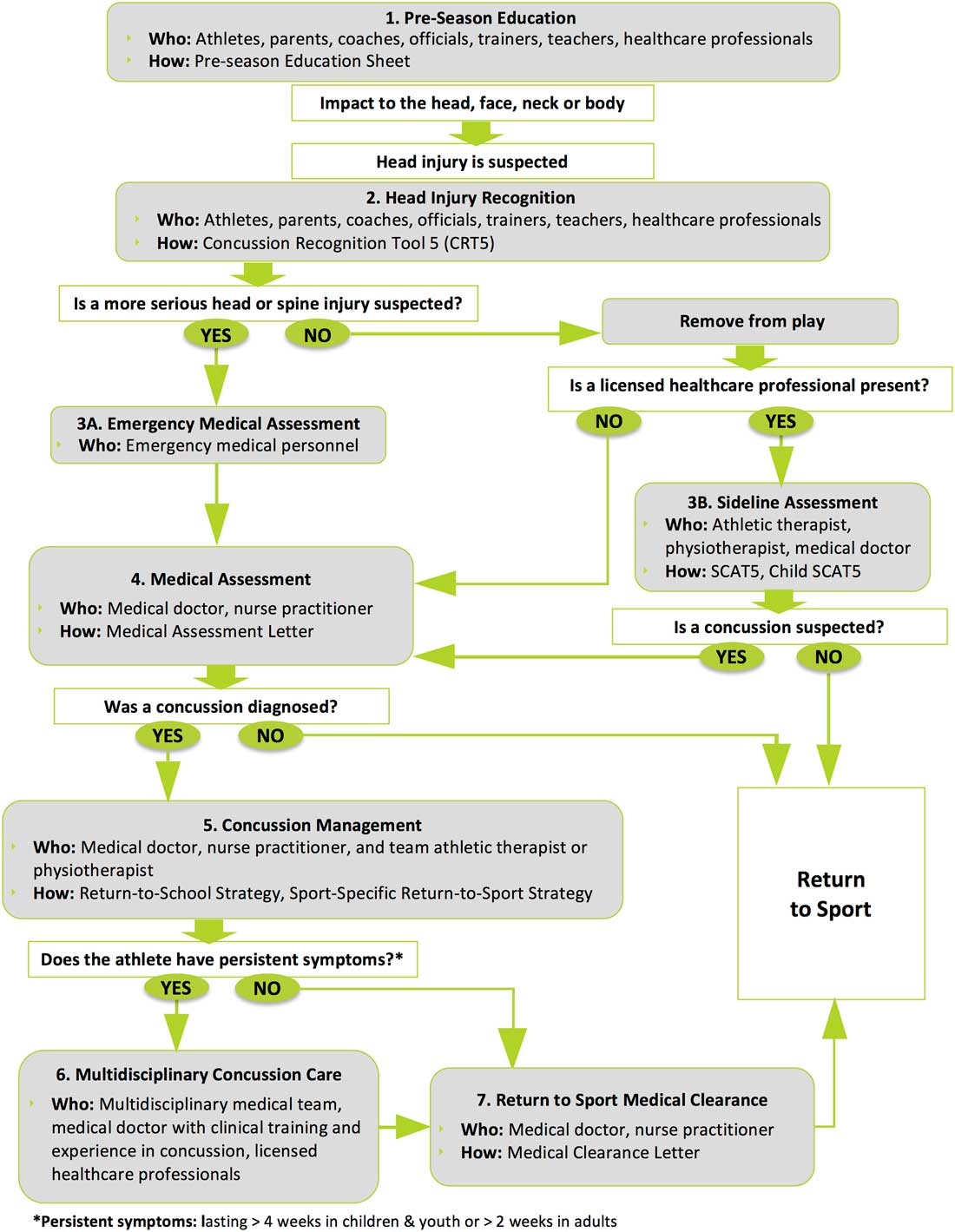
Figure 1 The Canadian sport concussion pathway (Reproduced with permission from Parachute Canada; Parachute: Canadian Guideline on Concussion in Sport. 2017. www.parachutecanada.org, accessed November 5, 2017).
This study has several important limitations. First, although the survey response rates for head coaches (71.4%) and parents (52.8%) were acceptable, we did not receive responses from all head coaches and parents. Therefore, it is possible that there were additional athletes who sustained a suspected concussion during the study season who were not managed through the standardized concussion protocol. As we did not obtain survey responses from athletes who participated in the 2016-2017 season, there may have also been injuries that were not reported to parents and coaches and thus were not captured. Indeed, under-reporting of concussions remains a persistent concern in youth sports,Reference Register-Mihalik, Guskiewicz, McLeod, Linnan, Mueller and Marshall 19 , Reference Rivara, Schiff, Chrisman, Chung, Ellenbogen and Herring 20 and future studies assessing compliance with standardized concussion protocols in youth sports should consider including athlete surveys. Second, the coaches and parents who provided post-season feedback on the concussion protocol were aware that the surveys were being undertaken by the pediatric concussion program, which may have influenced responses to certain questions. However, survey recipients were notified that their names or identifying characteristics were not being collected, which should have minimized any pressure to answer questions favorably.
In conclusion, this study suggests that adoption and implementation of a standardized medically supervised concussion protocol for elite youth hockey in Canada is feasible but identifies a number of key elements that should be considered in the development and periodic evaluation of these protocols. This study provides supportive evidence that standardized concussion protocols for high-risk youth sports such as hockey must ensure that all athletes with a suspected concussion have timely access to physicians and multi-disciplinary experts in TBI to ensure comprehensive medical management and safe return to play. Future research is needed to examine whether revisions to the 2017-2018 Winnipeg AAA Hockey concussion protocol lead to enhanced compliance and an improvement in sport stakeholder feedback.
Acknowledgments
The authors would like to thank Russ Cassidy, VP AAA Hockey, Kelsey McCuspey, Concussion Protocol Coordinator, and all coaches and parents for their support of Winnipeg AAA Concussion Protocol and this study.
Discloure
MJE reports receiving an honorarium from Parachute for his role as co-chair of the Expert Advisory Concussion Subcommittee. JL, DMC, KR, JK, and KR have nothing to disclose.
Conflicts of Interest
MJE is the co-chair of the Expert Advisory Committee for Parachute Canada, a non-profit injury prevention organization, who partnered with the Public Health Agency of Canada and National Sport Organizations to develop the Canadian Guideline on Concussion in Sport. He also represents the Canadian Neurosurgical Society on the Canadian Concussion Collaborative.
Statement of Authorship
Co-authors MJE and KFR conceptualized and designed the study, drafted the initial manuscript, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. JL, DMC, KR, and JK carried out data collection for the study, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2018.30